Wolf-Parkinson-White syndrome (WPW syndrome) is the presence of signs of a sudden increase in heart rate (tachycardia) due to the formation of an additional pathway (atrioventricular bundle of Kent) between the upper (atria) and lower (ventricles) parts of the heart. Excitation of the ventricles in this case occurs earlier than through physiological pathways. Cardiologists at the Yusupov Hospital successfully diagnose this pathology and provide modern, effective, minimally invasive treatment.
WPW syndrome - what is it?
According to statistics, heart rhythm disturbances due to WPW syndrome are detected only in 0.15–2% of cases.
The disease is more common among men and usually appears between 10 and 20 years of age. It leads to severe heart rhythm disturbances, requires a special approach to diagnosis and treatment, and can pose a threat to the patient’s life. Classification of WPW syndrome
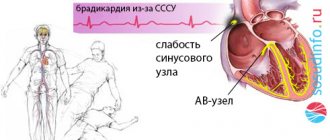
In cardiology, a distinction is made between the phenomenon of SVC and SVC syndrome. The first is characterized by electrocardiographic signs of cardiac impulse conduction through additional connections and overexcitation of the ventricles. In this case, there are no clinical manifestations of AV reciprocal tachycardia. WPW heart syndrome is a combination of ventricular overexcitation with symptoms of tachycardia.
Taking into account the morphological substrate, scientists identify the following anatomical types of SVC syndrome:
1. With additional muscle AV fibers. Muscle fibers can:
- pass through the accessory right/left parietal AV junction;
- go from the right/left atrial appendage;
- be associated with a sinus of Valsalva/middle vein vein aneurysm;
- go through the fibrous aortic-mitral junction;
- be paraseptal, septal superior/inferior.
2. With bundles of Kent (muscle AV fibers) originating from rudimentary tissue:
- and entering the myocardium of the right ventricle;
- and entering the right bundle branch (atrio-fascicular).
According to the nature of the manifestation they are classified:
- Manifesting WPW syndrome. Characterized by the constant presence of a delta wave, episodes of atrioventricular reciprocal tachycardia and sinus rhythm;
- Transient WPW syndrome (also known as intermittent WPW syndrome). The ECG diagnoses sinus rhythm, transient ventricular preexcitation, verified atrioventricular reciprocal tachycardia;
- Hidden WPW syndrome. Described by retrograde conduction along the bundle of Kent. The ECG reveals episodes of atrioventricular reciprocal tachycardia (at rest, the anomaly is not diagnosed using an ECG). Manifested by attacks of tachycardia.
According to the location, Keta bundles can be:
- left-sided (go from the left atrium to the left ventricle);
- right-sided (go from the right atrium to the right ventricle);
- paraseptal (go near the cardiac septum).
The location of the additional pathway is taken into account by cardiologists-arrhythmologists when choosing the most effective surgical access technique (through a vein or through the femoral artery).
SVC syndrome and pregnancy
SVC syndrome, which does not manifest itself clinically, does not require additional treatment. But during pregnancy, the disease can manifest itself with paroxysmal heart rhythm disturbances. Then a consultation with a cardiologist and selection of effective treatment is necessary.
With very frequent attacks of tachycardia against the background of WPW syndrome, pregnancy is contraindicated. This is explained by the fact that the disease at any period can develop into a life-threatening rhythm disorder. In addition, tachycardia often provokes insufficient blood circulation in organs and tissues, which negatively affects not only the condition of the mother, but also the development of the fetus.
Forecast
Determining the prognosis for patients with CLC syndrome is always difficult, since it is not possible to predict in advance the occurrence of certain rhythm disturbances, the frequency and conditions of their occurrence, as well as the occurrence of their complications.
According to statistics, the life expectancy of patients with short PQ syndrome is quite high, and paroxysmal rhythm disturbances most often occur in the form of supraventricular rather than ventricular tachycardias. However, in patients with underlying cardiac pathology, the risk of sudden cardiac death remains quite high.
The prognosis for the phenomenon of shortened PQ remains favorable, and the quality and life expectancy of such patients do not suffer.
Causes of WPW syndrome
SVC syndrome is a congenital disorder. The reason for its occurrence is a gene mutation, due to which, during the formation and formation of the heart in the prenatal period, bridges are formed between the ventricle and the atrium. A bunch of Kent grows.
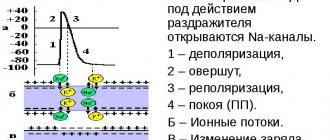
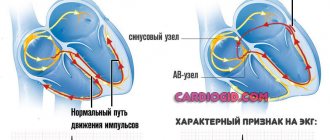
In patients with WPW syndrome, the propagation of excitation from the atria to the ventricles occurs along abnormal conduction pathways. As a result, the ventricular myocardium is excited earlier than if the impulse propagated in the usual way (AV node, bundle and branches of His). On the ECG, overexcitation of the ventricles is reflected in the form of a delta wave (an additional wave of depolarization). In this case, the QRS duration increases, and the PQ(R) interval, on the contrary, shortens.
At the moment the main wave of depolarization enters the ventricles, their collision in the heart muscle is recorded in the form of a slightly widened and deformed QRS complex.
Abnormal excitation of the ventricles provokes a violation of the sequence of repolarization processes. On the ECG, this looks like a discordant QRS complex, a shift in the RS-T segment and a change in the polarity of the T wave.
The development of atrial fibrillation and flutter, supraventricular tachycardia in WPW syndrome is explained by the formation of a circular excitation wave. The impulse moves along the AB node in the direction from the atria to the ventricles, and along additional pathways - from the ventricles to the atria.
Medical reference books
Pre-excitation syndrome
ICD-10: I45.6
Introduction
In 1930, L. Wolff, J. Parkinson and PD White published an article describing 11 patients who suffered attacks of tachycardia, and during sinus rhythm had a short PR interval and a wide QRS complex on the ECG, reminiscent of bundle branch block. After these authors, the syndrome they described was called Wolff-Parkinson-White (WPW) syndrome. WPW syndrome is one of the variants of “pre-excitation” of the ventricles. As defined by Durrer et al. (1970), the term “preexcitation” of the ventricles means that the ventricular myocardium is activated by the atrial impulse earlier than would be expected if the impulse entered the ventricles through the normal specialized conduction system. WPW syndrome is more common than other types of ventricular preexcitation. It is based on a congenital anomaly in the structure of the conduction system of the heart in the form of an additional bundle of Kent, connecting the myocardium of the atria and ventricles directly, bypassing the atrioventricular junction, and capable of rapidly conducting impulses. The conduction anomaly in WPW syndrome is manifested by characteristic ECG changes and a tendency to develop supraventricular tachycardias.
Pathophysiology
The bundles of Kent are formed in the embryonic period in the form of muscle bridges passing through the fibrous ring between the atria and ventricles. The electrophysiological characteristics of the Kent bundles (conduction velocity, refractoriness) differ from the properties of the atrioventricular connection, which creates the prerequisites for the development of arrhythmias through the mechanism of re-entry of the excitation wave (re-entry). The ability of the Kent bundles to rapidly conduct atrial impulses bypassing the atrioventricular junction determines the possibility of an unusually high heart rate during the development of atrial fibrillation/flutter, which in rare cases can cause ventricular fibrillation and sudden death.
Epidemiology
· Ventricular preexcitation occurs in the general population with a frequency of 0.1-0.3%. 60-70% of patients have no other signs of heart disease. · WPW syndrome is more common in men than in women. · The age of patients may vary. Typically, WPW syndrome is detected in childhood or adolescence when seeking emergency care for tachyarrhythmias. The speed of conduction along accessory pathways decreases with age. Cases have been described in which ECG signs of preexcitation completely disappeared over time. · Up to 80% of patients with WPW syndrome experience reciprocal (circular) tachycardia, 15-30% have atrial fibrillation, 5% have atrial flutter. Ventricular tachycardia is rare.\
Mortality
The risk of sudden arrhythmic death in patients with WPW syndrome is very low - about 0.15-0.39% over a follow-up period of 3 to 10 years. Sudden death as the first manifestation of the disease is relatively rare. On the contrary, in 1/2 of people with WPW syndrome who died suddenly, the cause of death was the first episode of tachyarrhythmia. The risk of sudden death increases when certain drugs (digoxin) are used to treat arrhythmias.
Clinical picture
History · Paroxysmal tachycardias in WPW syndrome often occur in childhood, but may first develop in adults. Having begun in childhood, arrhythmia can disappear for a while, then it recurs. If attacks of tachycardia have not stopped after the age of 5 years, the probability of their continuation in the future is 75%. · During an attack of tachycardia, various symptoms are possible - from minor discomfort in the chest, palpitations, dizziness to lightheadedness or loss of consciousness, severe hemodynamic disturbances and cardiac arrest. · Syncope can occur as a result of cerebral hypoperfusion against the background of tachyarrhythmia, or as a result of depression of the sinus node during tachyarrhythmia with the development of asystole after its cessation. · After the end of the paroxysm, polyuria may be observed (stretching of the atria during an attack leads to the release of atrial natriuretic peptide). · Signs of ventricular preexcitation can be detected by random ECG recording in individuals without rhythm disturbances (WPW phenomenon). · Asymptomatic patients rarely become symptomatic after age 40. With increasing age, there is a possibility of developing fibrosis in the area of attachment of the bundle, and therefore it loses the ability to conduct impulses from the atria to the ventricles. Physical findings WPW syndrome has no characteristic physical findings other than those associated with tachyarrhythmias. In young people, symptoms may be minimal even with a high heart rate. In other cases, during an attack there is coldness of the extremities, sweating, hypotension, and signs of congestion in the lungs may appear, especially with concomitant heart defects - congenital or acquired.
Diagnostics
1. Standard ECG WPW syndrome is characterized by the following ECG changes (
): · Short interval pQ < 0.12 s. - the result of accelerated entry of the impulse into the ventricles along the accessory pathway. · Delta wave – a gentle slope in the initial part of the QRS complex (the first 30-50 ms). - reflects the initial excitation of the ventricle through the accessory pathway, which runs away from the specialized conduction system and gives rise to a relatively slow transmission of impulse from fiber to fiber of the myocardium.
· Wide QRS complex > 0.10-0.12 s. - the result of excitation of the ventricles from two directions - leading through the accessory pathway, and immediately following this - through the AV connection. · Secondary changes in repolarization - the ST segment and T wave are usually directed in the direction opposite to the orientation of the delta wave and the QRS complex. Analysis of the polarity of the delta wave in various ECG leads allows us to determine the localization of the accessory pathway. An additional pathway can be manifest or hidden. — Manifest path - the ECG shows the above signs of pre-excitation, the bundle is capable of antegrade impulse conduction (from the atria to the ventricles). — Hidden path - there are no signs of pre-excitation on the ECG (the bundle conducts impulses only in the retrograde direction, from the ventricles to the atria, being the retrograde part of the re-entry circle in orthodromic tachycardia). In some patients, preexcitation may be intermittent (not constant), with a variable ECG pattern in the complexes of one recording or on cardiograms taken several days and even hours apart ().
2. Daily Holter ECG monitoring Allows you to record arrhythmias and detect intermittent ventricular preexcitation.
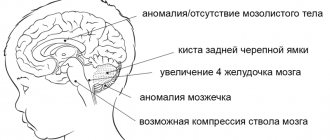
3. Echocardiography Allows you to evaluate the function of the left ventricle, myocardial contractility in various segments, exclude concomitant heart defects - valve defects, Ebstein's anomaly, corrected transposition of the great vessels, ventricular and atrial septal defects, hypertrophic cardiomyopathy, which can be combined with WPW syndrome.
4. Electrophysiological study (EPS) When examining some patients, a special electrophysiological study may be necessary. EPS can be non-invasive (method of transesophageal electrical stimulation of the heart - TEES) and invasive, endocardial. The last method is the most accurate. EPI allows you to clarify the mechanism of development of tachycardia, determine the localization of the accessory pathway and evaluate its electrophysiological properties (conductivity and duration of the refractory period). Beams with a short refractory period (less than 250-270 ms), and therefore capable of conducting pulses at high frequencies, are potentially dangerous.
Arrhythmias in WPW syndrome
In patients with WPW syndrome, various rhythm disturbances may occur, but the most common are 2 types of tachycardia: reciprocal (circular) tachycardia and atrial fibrillation/flutter.
1. Reciprocal atrioventricular tachycardia: orthodromic, antidromic · In sinus rhythm, impulses from the atria to the ventricles are carried out through both pathways - the atrioventricular connection and the bundle of Kent; there are no conditions for paroxysm of tachycardia. The triggering factor for circular tachycardia is usually an atrial extrasystole, which occurs at a critical moment in the cardiac cycle, namely when a premature impulse can be carried to the ventricles through only one path, due to the refractoriness of the second. · Most often, the Kent bundle is refractory (90-95% of cases), and the ventricles are excited through the atrioventricular connection (orthodromic). After the end of ventricular excitation, the impulse can return to the atria along the accessory pathway, moving in a retrograde direction, and re-enter the atrioventricular junction, closing the circle of tachycardia. With this direction of impulse movement, the tachycardia is called orthodromic reciprocal AV tachycardia. Its features: 1) narrow QRS complex; 2) strict regularity of rhythm; 3) signs of retrograde excitation of the atria behind the QRS complex (P wave - negative polarity in leads II, III and avF) (
).
· Attacks of orthodromic tachycardia can also be observed in patients with hidden bundles of Kent, due to the ability of the accessory pathway to conduct retrogradely. · Antidromic reciprocal AV tachycardia occurs 10-15 times less frequently than orthodromic tachycardia. In this case, the impulse enters the ventricle through the accessory pathway (antidromically) and returns to the atrium through the atrioventricular junction in a retrograde direction. Tachycardia is formed 1) with wide QRS complexes, 2) strictly regular, with a potentially higher rhythm frequency, since the beam has a short refractory period, 3) the retrograde P wave is located in front of the QRS complex, but is usually poorly distinguishable. The ventricular complex in this case represents a continuous delta wave, coinciding in polarity in each lead with the delta wave in sinus rhythm. Such tachycardia is difficult to distinguish from ventricular (
). If the diagnosis is in doubt, this form of supraventricular arrhythmia should be treated as ventricular arrhythmia. · Antidromic tachycardia is more dangerous than orthodromic tachycardia: it is less tolerated and more often transforms into ventricular fibrillation.
2. Atrial fibrillation · Atrial fibrillation occurs in patients with WPW syndrome much more often than in people of the same age in the general population - with a frequency of 11-38%. The predisposition to the development of atrial fibrillation in WPW syndrome is explained by changes in the electrophysiological properties of the atria under the influence of frequent paroxysms of circular tachycardia, and even by the very fact of attachment of the bundle to the atrial myocardium. It is also believed that atrial fibrillation may occur as a result of changes in the atria that accompany WPW syndrome, independent of the presence of the accessory pathway. · Atrial fibrillation is the most dangerous arrhythmia in WPW syndrome, which can degenerate into ventricular fibrillation. The appearance of paroxysms of atrial fibrillation in a patient with WPW syndrome means an unfavorable turn in the course of the disease. The time of onset of atrial fibrillation may vary: it may be the first attack of tachycardia in a patient with WPW syndrome, occur in patients with a long history of reentrant tachycardia, or develop during an attack of reentrant tachycardia. · Normally, the atrioventricular connection acts as a physiological filter on the path of frequent impulses from the atria, passing no more than 200 impulses per minute during atrial fibrillation into the ventricles. In patients with WPW syndrome, impulses flow from the atria to the ventricles using both the AV junction and the bundle of Kent. Due to the short refractory period and the high speed of conduction along the accessory pathway, the number of heart contractions can reach 250-300 or more per minute. In this regard, AF in WPW syndrome is often accompanied by hemodynamic impairment, which is clinically manifested by hypotension and syncope. · Impaired hemodynamics during a paroxysm of AF causes sympathetic activation, which further increases the frequency of conduction along the accessory pathway. Too high a heart rate can cause atrial fibrillation to transform into ventricular fibrillation. · On the ECG during atrial fibrillation in patients with ventricular preexcitation, a frequent irregular rhythm (heart rate more than 200/min) with wide polymorphic QRS complexes of unusual shape is recorded. The originality of the ventricular complexes in this arrhythmia is associated with their confluent nature (the shape of the QRS is determined by the relative participation of the AV junction and the accessory pathway in the excitation of the ventricles). Unlike polymorphic ventricular tachycardia, there is no “torsades de pointes” phenomenon (
).
· Measurement of the shortest RR interval on an ECG taken during an attack of atrial fibrillation in a patient with WPW syndrome is used to assess the degree of risk: the danger is maximum if RRmin ≤ 220-250 ms.
Risk stratification
The optimal treatment strategy for WPW syndrome is determined based on an individual assessment of the risk of sudden death. · Persons with signs of pre-excitation on the ECG who have not suffered tachycardia usually do not require either treatment or additional examination. The exception is professional athletes and representatives of high-risk professions (pilots, drivers, etc.): they are recommended to undergo an electrophysiological examination to determine the properties of the accessory pathway and the associated risk of sudden death. · The intermittent nature of ventricular preexcitation, the disappearance of the delta wave against the background of increased rhythm or during physical activity, as well as after intravenous administration of procainamide or ajmaline, are characteristic of accessory pathways with a long refractory period. Such accessory pathways are usually not capable of conducting impulses frequently if atrial fibrillation/flutter develops. The risk of sudden cardiac death is low. · High-risk markers for WPW syndrome, established in a retrospective analysis of cases of sudden death of patients: 1) the shortest RR interval for atrial fibrillation less than 250 ms; 2) history of symptomatic tachyarrhythmias; 3) multiple accessory pathways; 4) Ebstein's anomaly; 5) familial form of WPW syndrome, cases of sudden death in the family history. · The risk of sudden death can be assessed most accurately by intracardial EPI.
Treatment
Patients with WPW syndrome require treatment during paroxysms of tachycardia and to prevent relapses.
Relief of tachycardias 1. Orthodromic reciprocal tachycardia (narrow QRS complex, frequency - about 200/min, retrograde P is clearly visible behind the QRS complex): treatment is aimed at slowing down conduction in the AV node. · Vagal techniques (performing the Valsalva maneuver, unilateral carotid sinus massage, immersing the face in cold water, applying an ice pack to the face) are more effective at the onset of an attack. · ATP or adenosine intravenously (ATP for adults in a dose of 10-40 mg in the form of a bolus, intravenously quickly, over 3-5 seconds; adenosine 37.5 mcg/kg, intravenously quickly, if necessary - after 2-3 min at double dose – 75 mcg/kg). - do not use for sick sinus syndrome, bronchial asthma, vasospastic angina; — effective in 90% of cases of reciprocal tachycardia with a narrow QRS complex; ineffectiveness is usually associated with inadequate administration technique (rapid bolus administration is necessary due to the short half-life of the drug); - There should be a readiness to carry out defibrillation in the event of the development of another form of tachycardia (especially atrial fibrillation) after the administration of adenosine. · Verapamil intravenously (5 mg IV over 2 minutes, if the arrhythmia persists, repeat after 5 minutes at the same dose to a total dose of 15 mg). - used if tachycardia recurs, or ATP/adenosine is ineffective, or if the patient is taking theophylline; — verapamil is not used for WPW syndrome if the patient has already had episodes of atrial fibrillation.
2. Atrial fibrillation/flutter, antidromic reentrant tachycardia are tachycardias with ventricular preexcitation (wide QRS complex). They often occur with a high heart rate, severe symptoms, hemodynamic disturbances, and, therefore, require immediate cessation. In an urgent situation with unstable hemodynamics, electrical cardioversion is indicated (1st shock energy - 100 joules). If tachycardia is well tolerated, or electrical cardioversion is ineffective, drug therapy is performed. For the treatment of this group of arrhythmias, drugs that lengthen the refractory period of the accessory pathway (procainamide, cordarone) are indicated. Blocking the accessory pathway eliminates ventricular preexcitation, and with it the threat of sudden arrhythmic death. · Novocainamide – in patients without structural myocardial damage (intravenous infusion at a rate of 20 mg per minute until tachycardia is stopped; administration of the drug is stopped when hypotension develops, the QRS width increases by 50% of the original, or when the maximum dose of 17 mg/kg is reached). · Amiodarone – in patients with structural heart disease (loading dose – 5 mg/kg in a 5% glucose solution, IV drip over 20 minutes, then continue administration at a dose of 600-900 mg over 24 hours). NB: Digoxin, verapamil and beta blockers should not be used to treat atrial fibrillation/flutter in patients with WPW syndrome. By slowing down conduction through the atrioventricular junction, these drugs increase the conduction of impulses along the accessory pathway, heart rate and contribute to the transition of arrhythmia to ventricular fibrillation. NB: Lidocaine is also not used in this situation, since it does not prolong the refractory period of the accessory pathway. In patients with ventricular preexcitation, lidocaine may increase the rate of ventricular responses in atrial fibrillation.
Prevention
There are fundamentally two ways to prevent repeated episodes of arrhythmia in patients with WPW syndrome: pharmacological and non-pharmacological. The first approach involves long-term use of antiarrhythmic drugs. For a number of reasons, this route is not optimal: 1) arrhythmias in WPW syndrome are characterized by a high rate of rhythm and are associated with a potential threat to life, while the response to drug therapy is variable and unpredictable; 2) some drugs can paradoxically increase the frequency of paroxysms or the rhythm during episodes of tachycardia; 3) WPW syndrome often occurs in children and young people, in whom long-term use of antiarrhythmics is especially undesirable; 4) one cannot ignore the risk of developing systemic side effects, for example, thyroid dysfunction, photosensitivity or lung damage when taking amiodarone. · If drug therapy is necessary, preference is given to class ІC and III drugs that can block conduction along the accessory pathway (in international recommendations - propafenone and flecainide (IC), sotalol and amiodarone (III); recommendations of Russian authors also include etacizine (IC) and gilurythmal (IA)). Evaluation of the effectiveness of amiodarone in the treatment of patients suffering from tachycardias involving the accessory pathway did not show any advantages compared with class IC drugs and sotalol. These data, as well as the risk of systemic side effects, limit the long-term use of amiodarone in WPW syndrome to prevent paroxysmal tachycardias. The exception is patients with WPW syndrome and structural heart disease.
- Propafenone – 600-900 mg/day per day in 3 divided doses.
- Sotalol – 80-160 (maximum – 240) mg 2 times a day.
- Etatsizin – 25-50 mg 3 times a day.
Amiodarone - after reaching a saturating dose of 10-12 g - 200 mg 1 time per day, daily or with a break 2 days a week.
· Long-term use of beta blockers in WPW syndrome is acceptable, especially if, according to EPI, the accessory pathway is not capable of rapid completion. · Verapamil, diltiazem and digoxin should not be prescribed to patients with ventricular preexcitation, due to the risk of increased ventricular responses if atrial fibrillation develops.
The second way, non-drug, is associated with the destruction of the accessory pathway, either using a catheter (usually by electrical radiofrequency ablation - RFA), or surgically during open-heart surgery. Currently, RFA is becoming the first-line treatment for symptomatic patients with WPW syndrome, gradually replacing both medical and surgical approaches. The effectiveness of initial ablation of the accessory pathway reaches 95%, although in 5% of cases the arrhythmia may recur after elimination of inflammation and edema in the damaged area. In such cases, the accessory tract is usually successfully destroyed when the procedure is repeated. Catheter ablation can sometimes cause complications, and in rare cases, death (0 to 0.2%).
Indications for RFA · Symptomatic reciprocal atrioventricular tachycardia. · Atrial fibrillation (or other symptomatic atrial tachyarrhythmias) with a high frequency of conduction along the accessory pathway. · Asymptomatic patients with ventricular pre-excitation (WPW phenomenon), if the safety of the patient and those around him (pilots, deep-sea divers, etc.) may depend on their professional activities during the spontaneous development of tachycardia. · Family history of sudden death. Thus, for the treatment of patients with WPW syndrome (ECG signs of pre-excitation and symptomatic arrhythmias), especially with hemodynamic instability during arrhythmia paroxysms, RFA of the accessory pathway is the method of choice. In patients with hidden accessory pathways (without pre-excitation on the ECG), with rare low-symtom attacks of tachycardia, the risk is low; the treatment approach may be more conservative and take into account the patient's preferences.
Patient education Patients with WPW syndrome should be informed about the causes of the disease and its possible manifestations. This is especially important for young asymptomatic individuals, in case of detection of ventricular preexcitation for the first time during random ECG recording (WPW phenomenon). It is necessary to recommend that the patient undergo dynamic monitoring with mandatory consultation with a doctor if symptoms appear. It is advisable that a patient with ventricular preexcitation always have an ECG with him with a conclusion. Patients receiving drug therapy should know what medications they are taking. When counseling a patient with WPW syndrome, you need to explain the following: · How to recognize the manifestations of the disease. · How to apply vagal techniques, if necessary. · What may be the side effects of antiarrhythmic drugs if the patient takes them. · The advisability of refusing to engage in competitive sports. · Possibilities of RFA in the treatment of WPW syndrome and indications for its implementation, if any appear in the future. Relatives of a patient with WPW syndrome should be recommended a screening examination to exclude ventricular preexcitation.
Symptoms of WPW syndrome
Symptoms of SVC syndrome are usually mild. These include heart rhythm disorders:
- atrial flutter;
- atrial fibrillation;
- reciprocal supraventricular tachycardia;
- ventricular tachycardia;
- ventricular/atrial extrasystole.
In turn, attacks of rapid rhythmic/irrhythmic heartbeat are accompanied by:
- “fluttering”/fading heart;
- attacks of suffocation (feeling of lack of air);
- dizziness;
- increased heart rate;
- arterial hypotension;
- weakness, loss of consciousness.
Deterioration of the patient's condition may occur after drinking alcohol, emotional or physical stress.
In most cases, paroxysmal arrhythmia in SVC syndrome can be stopped by taking a deep breath and holding the air. Prolonged attacks require emergency hospitalization and treatment under the supervision of a cardiologist.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
ICD-10 code
Wolff-Parkinson-White syndrome is a combination of premature ventricular excitation and paroxysmal tachycardia. With age, the frequency of paroxysms of supraventricular tachycardia increases. In patients under 40 years of age, 10% of cases are observed, and in patients over 60 years of age – 36%. The syndrome in most cases is a precursor (if it is recorded in people under 40 years of age) of arrhythmia. In 30% of cases the disease is combined with congenital heart defects.
I45.6 Premature excitation syndrome
Diagnosis of WPW syndrome
Diagnosis of SVC syndrome in children and adults includes a comprehensive clinical and instrumental examination. Conducted:
- Registration of ECG in 12 leads;
- Holter ECG monitoring. Electrodes are attached to the heart area and lead to a portable recorder. The patient walks with them for one day or more. At the same time, he leads a normal life, records all his actions and sensations in a diary;
- Transthoracic echocardiography. A modern method for non-invasive cardiac imaging using reflected ultrasound signals. Allows you to evaluate the morphological and functional structures of the organ;
- Transesophageal pacing. Includes insertion of an electrode into the esophagus, delivery of stimulating electrical impulses, determination of stimulation threshold values, interpretation of ECG information readings;
- Endocardial electrophysiological study of the heart. Aimed at recording and monitoring various indicators of heart function using recording equipment and special sensors. Makes it possible to accurately determine the number and location of additional pathways (Ken's bundles), verify the clinical form of the disease and evaluate the effectiveness of drug therapy or previously performed radiofrequency catheter ablation;
- Ultrasound diagnostics. Allows you to identify concomitant pathologies, heart defects, cardiomyopathy.
Electrocardiographic signs of SVC heart syndrome include:
- shortened PQ interval (does not exceed 0.12 s);
- delta wave;
- deformed confluent QRS complex.
When making a diagnosis, a differential diagnosis of SVC syndrome with bundle branch blocks is required.
Features of the pathology
Pre-excitation of the cardiac ventricles can be asymptomatic, in which case we are talking about the “pre-excitation phenomenon”. When signs of pathology appear in a patient, the disease is classified as “pre-excitation syndrome.”
There are several types of disease:
- Breschenmash (atriofascicular) - here the right atrium is connected to the trunk of the His bundle;
- Maheima (nodoventricular) - in this case, the right side of the interventricular septum is connected to the atrioventricular node;
- Kent (atrioventricular) - here the atria and ventricles are connected bypassing the atrioventricular node;
- James (atrionodal) - impulses pass between the lower part of the atrioventricular and sinoatrial node.
Important! Sometimes there are several paths of abnormal conduction of impulses. The number of such patients is no more than 10% of all cases of the disease.
CLC syndrome is clearly monitored by performing an electrocardiogram
Treatment of cardiac SVC syndrome
If there are no arrhythmia paroxysms, SVC syndrome does not require special treatment. With pronounced attacks accompanied by hypotension, symptoms of heart failure, angina pectoris, syncope, the question arises of conservative or surgical treatment.
Conservative methods are aimed at preventing attacks of rapid heartbeat (tachycardia). The patient is prescribed:
- Preventive antiarrhythmic drugs (Amiodarone, Flecainide, Propafenone, Adenosine, etc.);
- Beta blockers - prevent stimulation of receptors for norepinephrine and adrenaline (Esmolol);
- Blockers of slow calcium channels - have an effect on the cells of blood vessels and the heart, reduce the heart rate, reduce vascular tone;
- Cardiac glycosides - increase the strength of heart contractions.
In order to stop attacks of tachycardia, intravenous administration of antiarrhythmic drugs is used.
In some cases, the following help stop paroxysms of arrhythmias:
- Valsava's test;
- carotid sinus massage;
- intravenous administration of ATP.
If conservative therapy does not improve the patient's condition and the symptoms of tachycardia do not disappear, surgical treatment of WPW syndrome is performed. Indications for it also include:
- contraindications to long-term drug therapy;
- frequent attacks of atrial fibrillation;
- the presence of tachyarrhythmia attacks complicated by hemodynamic disturbances.
The operation is called radiofrequency catheter ablation. It is performed under local anesthesia. During it, a special thin tube - a conductor - is brought to the heart through the femoral vessels. An impulse is sent through it, which destroys Kent's beam. The effectiveness of radiofrequency ablation according to statistical data is 95%. In 2% of cases, relapses of the disease are possible - tissues that have undergone ablation repair themselves. Then a repeat operation is required.
It is important to know that sports are contraindicated in case of SVC syndrome.
Danger of SVC syndrome
SVC syndrome, manifested by attacks of tachycardia, reduces the patient’s quality of life. Loss of consciousness during paroxysms can lead to serious injuries and accidents.
In addition, reciprocal AV tachycardias in WPW syndrome belong to the category of prefibrillatory arrhythmias. This means that frequent attacks of the disease can lead to more dangerous and complex atrial fibrillation, which in turn can transform into ventricular fibrillation and lead to death.
What is the difference between a syndrome and a phenomenon?
Many patients, having seen the concepts of the phenomenon or CLC syndrome in the ECG conclusion, may be puzzled which of these diagnoses is worse. The CLC phenomenon, subject to a correct lifestyle and regular monitoring by a cardiologist, does not pose a great danger to health, since the phenomenon
– this is the presence of signs of PQ shortening on the cardiogram, but without clinical manifestations of paroxysmal tachycardia.
Syndrome
CLC, in turn, is an ECG criterion that is accompanied by paroxysmal tachycardia, most often supraventricular, and can cause sudden cardiac death (in relatively rare cases). Typically, patients with short PQ syndrome develop supraventricular tachycardia, which can be quite successfully stopped at the stage of emergency medical care.
Prevention of WPW syndrome
There is no specific prevention of the disease. If an ECG reveals a patient with SVC syndrome, he should be regularly examined by a cardiologist (even if the symptoms do not bother him). If signs of pathology appear, you need to immediately choose the right treatment.
Persons who are related to a patient with WPW syndrome are recommended to undergo a routine examination to exclude the development of this pathology in themselves. Diagnostics should include: daily monitoring of the electrocardiogram, electrocardiogram, electrophysiological methods.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Wolff-Parkinson-White syndrome in children
Congenital pathology in children manifests itself in the first year of life. It has been proven that hereditary predisposition is transmitted in an autosomal recessive manner.
In infants, an attack of paroxysmal tachycardia can be complicated by the development of heart failure and impaired liver function.
It is possible to suspect the presence of pathology at an early age based on the following signs:
- decreased appetite;
- manifestation of shortness of breath;
- low blood pressure;
- presence of pulsation in the chest in the area of the heart;
- low activity.
If a child has a sign of WPW syndrome once recorded on an ECG (even without a clinical picture of the disease), there is a high probability that at an older age he will develop paroxysmal tachycardia. There is a risk of developing life-threatening conditions and sudden death.