DlyaSerdca → Diagnostics → Frederick's syndrome: clinical features and diagnosis
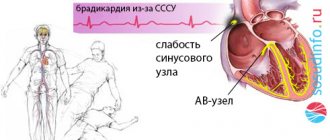
Frederick's syndrome is a combination of two heart rhythm disorders - complete atrioventricular block and atrial flutter or fibrillation.
This combination of disorders, detected primarily using the electrocardiographic method (ECG), is also called the Frederick phenomenon.
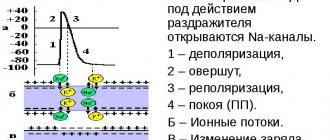
Complete atrioventricular block implies the impossibility of the passage of nerve impulses that stimulate the contractile activity of myocardial cells from the atria to the ventricles.
Normally, the nerve impulse originates in a specialized atrial node (sinoatrial node), and then spreads through the fibers of the conduction system to the ventricular myocardium.
This ensures coordinated contractions of the atria and ventricles, therefore, the coordinated functioning of all parts of the heart. With the disease in question, nerve impulses originate in the atria, but are not conducted into the ventricles.
Frederick's syndrome
This causes the muscle fibers of the atria to contract chaotically, experiencing excessive nerve stimulation (that is, flutter, and possibly even atrial fibrillation, develops).
The conduction system of the ventricles, in turn, not receiving nerve impulses from the upper parts, generates them independently, triggering the so-called ventricular rhythm of the heart. These processes underlie the phenomenon.
The question naturally arises as to why this syndrome develops.
The reasons may be:
chronic ischemic heart disease;- large-focal post-infarction cardiosclerosis;
- various types of cardiomyopathies;
- myocarditis of various etiologies;
- heart defects (both congenital and acquired).
Thus, it becomes clear that the basis of the disease is always gross organic pathology, creating a mechanical obstacle to the passage of nerve impulses. As a rule, these are gross cicatricial or degenerative changes in the myocardium.
What is Frederick's syndrome
In this condition, the atria contract chaotically, irregularly, that is, their fibrillation is recorded. In some cases, fibrillation is replaced by atrial flutter. In this case, the rhythm of atrial contraction becomes regular, but it remains very frequent and is accompanied by a violation of intracardiac hemodynamics (blood movement from the atria to the ventricles).
In atrial fibrillation (atrial fibrillation), impulses from the atria are sent to the ventricles along the conduction pathways, through the atrioventricular node. With Frederick's syndrome, there is a complete cessation of the movement of electrical signals from the atria to the ventricles. This condition is called complete atrioventricular (complete transverse, third degree) block.
Since the ventricles of the heart cease to receive excitatory impulses from the atria, foci that produce electrical signals are activated in their wall or in the lower part of the atrioventricular node. This phenomenon is physiologically determined and protects the heart from stopping. The ventricular rhythm replaces normal contractions. However, the frequency with which the ectopic lesion produces impulses is significantly lower than in normal sinus rhythm. It ranges from 40 to 60 pulses per minute, and in many cases even less. The ventricles of the heart contract slowly, the volume of pumped blood decreases, and the body begins to lack oxygen. Clinical signs of Frederick's syndrome appear.
Risk factors
There are so-called risk factors that do not directly cause the onset of pathological changes, but actively push the body to the line:
- Genetic predisposition. Heredity plays an important role. As was said, some of the deviations are transmitted as a result of disorders of intrauterine development, others - as a result of a fundamental change during the process of embryogenesis.
- Frequent inflammatory and infectious diseases of one kind or another.
- Long-term or improper use of heart medications, antihypertensive drugs, psychotropics, antibiotics, progestin contraceptives.
- Metabolic disorders of generalized type.
Causes
Severe organic heart diseases lead to the appearance of complete atrioventricular block:
- chronic ischemic heart disease (angina pectoris and rest);
- post-infarction cardiosclerosis;
- acute myocardial infarction;
- cardiomyopathy;
- myocarditis;
- severe heart defects.
With these diseases, sclerotic processes develop in the myocardium, accompanied by the growth of connective tissue in the cardiac muscle. In addition, inflammation and dystrophy of the heart muscle are important. The resulting connective tissue replaces normal cells that generate and conduct electrical impulses. As a result, the conduction function is disrupted and a transverse block occurs.
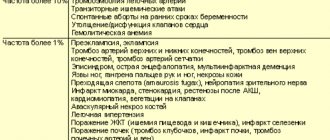
Possible complications
Possible consequences of the pathological process:
- Cardiogenic shock. A total disorder of cardiac function develops against the background of conduction disturbances, especially often. The lethality of the process is almost one hundred percent, regardless of the form.
- Heart attack. Necrosis of cardiomyocytes and scarring of affected areas.
- Heart failure. It is not accompanied by preliminary symptoms and occurs suddenly. Almost always lead to death due to the unpreparedness of the patient and his loved ones for such a scenario.
- Vascular dementia. Accompanied by signs inherent in Alzheimer's disease. It is potentially reversible at the first stage.
- Stroke.
- Multiple organ failure or dysfunction of individual systems.
Clinical signs
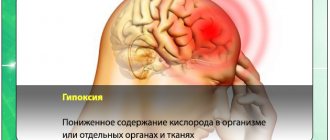
Symptoms of Frederick's syndrome are caused by a decrease in the pumping function of the heart. A rare pulse is accompanied by oxygen starvation of the brain.
Brain hypoxia can manifest itself as weakness, dizziness, shortness of breath, and low exercise tolerance. In severe cases, so-called Morgagni-Adams-Stokes attacks appear.
They occur when pauses in the heart last more than 5 seconds. This condition can develop in the absence of ventricular escape rhythm. In addition, a rare rhythm with complete atrioventricular block may be accompanied by ventricular extrasystole and a tendency to paroxysmal ventricular tachycardia. The development of paroxysms of tachycardia may also be accompanied by loss of consciousness.
Prevention, or How to avoid illness
Unfortunately, there is no prevention of a disease such as Frederick's syndrome, since it is usually a consequence of previous illnesses. To prevent this phenomenon, it is necessary to prevent and properly treat the ailments that provoke this disease.
At the slightest suspicion of this disease, it is recommended to immediately contact a specialist and be examined for the presence of this disease. One of the most dangerous conditions for human life is oxygen starvation, which in Frederick's syndrome can last about 7 seconds. This time will be enough to activate irreversible changes in the human brain.
If you discover at least one of the symptoms inherent in this disease, you should immediately contact a specialist. Timely diagnosis and treatment is the key to further full life. The prognosis for this disease is favorable and encouraging.
Diagnostics
The diagnosis of Frederick's syndrome is based on the characteristic electrocardiographic pattern. There are no P waves on the electrocardiogram, reflecting normal atrial contraction. Instead, small frequent ff waves are recorded, which are a reflection of atrial fibrillation, or larger and rarer FF waves, reflecting atrial flutter.
The ventricular rhythm is regular. When it is formed in the lower part of the atrioventricular junction, the ventricular complexes are narrow and of normal morphology. When the source of the rhythm is in the conduction system of the ventricles, the ventricular complexes are dilated and deformed.
Frederick's syndrome is an indication for 24-hour Holter electrocardiogram monitoring. Using this method of functional diagnostics, you can evaluate the rhythm frequency at different times of the day, the heart’s response to stress, determine the presence of pauses, ventricular extrasystoles or paroxysms of ventricular tachycardia.
Additionally, echocardiography (ultrasound examination of the heart) is performed, which makes it possible to clarify the nature of the underlying disease and the degree of morphological changes in the heart.
Main symptoms
The syndrome is a life-threatening arrhythmia; it indicates a complication of the underlying cardiovascular disease. In the early stages, while the body compensates for the lack of oxygen necessary for the functioning of the heart and brain, the patient almost does not feel the symptoms of the disease.
Early manifestations may include slight dizziness, feeling unwell and weak after minor physical activity, which do not significantly impair quality of life. They are usually attributed to “accumulated” fatigue, anemia, vitamin deficiency, etc.
Frederick's syndrome rapidly progresses, manifestations of heart failure (the heart does not provide normal blood supply to organs and tissues) and cerebral ischemia intensify, and the quality of life at this stage greatly deteriorates. It is difficult for the patient to perform even simple everyday activities; he becomes completely unable to work.
There are no specific symptoms by which the syndrome could be diagnosed; it is similar to many cardiovascular diseases:
- dizziness;
- shortness of breath (first after physical activity, and then at rest);
- weakness;
- episodes of heart rhythm disturbances;
- rare pulse (up to 40 beats per minute);
- swelling of the ankles.
After the appearance of such a symptom of cerebral ischemia as temporary loss of consciousness, the patient’s further prognosis sharply worsens: about 95% die within 3 years.
Diagnostics
The specific nature of the work of the atria and ventricles, typical of Frederick's syndrome, is fully revealed only on the ECG:
- There are no (P) waves, indicating normal atrial contractions.
- They are replaced by waves of frequent and chaotic atrial contraction (flutter (F) and flicker (f).
- The heart rhythm (R–R) is correct (the same intervals between contractions are maintained).
- Signs of complete atrioventricular block (blockade of impulse transmission from the atria to the ventricles) are recorded, and the shape of the ventricular complexes (QRS) is changed.
- The number of ventricular contractions is reduced (up to 40), and extrasystoles (extraordinary contractions) may appear.
The pathology is confirmed by 24-hour Holter ECG monitoring.
Treatment
Frederick's syndrome is an indication for implantation of an artificial pacemaker. The most commonly used is single-chamber ventricular pacing (VVI or VVIR). To do this, an electrode is installed in the ventricle of the heart, delivering impulses that excite the myocardium and cause its contraction. The frequency of contractions is programmed in advance, usually 70 beats per minute. When the VVIR stimulator is installed, the pulse frequency automatically changes depending on the patient's physical activity. This is the most physiological stimulation option.
Anticholinergic drugs, for example, atropine, are not used due to the likelihood of developing mental disorders in the patient (“atropine psychosis”).
Forecast
Prognostic assessments depend on the moment of initiation of therapy, health status, age, body weight, concomitant pathologies and other factors.
By installing a pacemaker, it is possible to improve the likely outcome quite significantly.
If mortality without therapy is 96% or higher, after implantation the figure drops to 25-30% or less; if in addition there are no risk factors, and there are many positive prognostic factors, the likelihood of a long and high-quality life is maximum.
A negative factor that neutralizes all the benefits of radical treatment is the presence of fainting and syncope in the clinical picture. This is a sign of cerebral ischemia. Such patients most often die within 2-4 years.
ECG and other examination methods
A diagnosis can be made based on the characteristic signs on. These include:
- absence of atrial waves;
- frequent and low f or F waves (they are larger and less frequent);
- QRS complexes from the lower part of the atrioventricular node are narrow, and from the myocardium of the ventricles themselves - deformed and wide, frequency no more than 40 - 60 per minute;
- the distances between the atrial waves and ventricular complexes are equal;
- The rhythm of contractions of the atria and ventricles does not coincide.
To clarify the diagnosis and assess the severity of the syndrome, it is indicated to carry out.
Additionally, an ultrasound of the heart is prescribed to determine the cause of the rhythm disturbance and study the viability of the myocardium.
Etiology and pathogenesis
The human heart is a unique organ that works according to the strictest physiological laws. Some cardiac pathologies disrupt its functioning and rhythm, which leads to hypoxia of organs and tissues.
With Frederick's syndrome, the functioning of the atria is disrupted, arrhythmia develops, nerve impulses cease to be conducted into the ventricles, and the myocardium contracts frequently and irregularly. There are no organic heart lesions.
Popular articles Acute myocardial infarction: causes and symptoms, treatment and possible complications
The ventricles begin to independently generate nerve impulses. Pathological foci appear in the atrioventricular node of the ventricles, which produce excitatory signals. The ventricular rhythm is started, protecting against cardiac arrest and preventing the death of a person. Gradually, the heart rate decreases to 40-60 beats per minute. Compensatory contraction of the ventricles occurs more slowly than in healthy people. Systemic blood flow slows down, hypoxia develops, the consequences of which are dangerous to human life.
Severe cardiac diseases lead to the development of Frederick's syndrome:
- Cardiac ischemia,
- Post-infarction sclerosis of the heart muscle,
- Acute coronary insufficiency,
- Inflammatory diseases of the myocardium,
- Heart defects
- Rheumatic carditis,
- Pronounced vagotonia,
- Connective tissue diseases
- Syphilitic myocarditis.
Various surgical interventions on the heart lead to the development of Frederick's syndrome. Drug intoxication is a common cause of pathology. Typically, poisoning of the body is caused by cardiac glycosides, β-blockers, slow calcium channel blockers, antiarrhythmics, and lithium salts.
Idiopathic fibrosis and sclerosis of the myocardium leads to dystrophy and dysfunction of the heart muscle. Cardiomyocytes that generate electrical activity are replaced by connective tissue cells.
Features of therapy
Treatment of Brugada syndrome is actively discussed, experts propose approaches to prescribing medications based on clinical experience and the results of their use in patients with pathology of the electrical activity of the heart, but to this day no effective drug method has been found for the prevention of ventricular arrhythmias and sudden death.
Patients in whom ECG phenomena are provoked by tests with the introduction of a sodium channel blocker, but there are no symptoms at rest, and there are no cases of sudden death in the family, need observation.
Medicines
Drug therapy consists of prescribing class IA antiarrhythmic drugs - Quinidine, Amiodarone, Disopyramide. It is worth noting that the drugs Novocainamide, Aymalin, Flecainide, belonging to class I, cause blockade of sodium channels and, accordingly, symptoms of Brugada syndrome, so they should be avoided. They provoke arrhythmia, and therefore Flecainide, Procainamide, Propafenone are contraindicated.
Quinidine is usually prescribed in small dosages (300-600 mg), is able to prevent episodes of ventricular tachycardia, and can be used in patients with a discharged defibrillator as an additional means of preventing sudden death.
Isoproterenol is considered effective, acting on beta-adrenergic receptors of the heart, which can be combined with Quinidine. This drug can help reduce the ST segment to the baseline and is applicable in pediatric practice. A new drug that “returns” the ST segment to its normal position is Phosphodiesterase.
It has been shown that many antiarrhythmic drugs cause blockade of sodium channels in cardiomyocytes, so it would be logical to assume that those that do not have such an effect - Diltiazem, Bretyllium - would be safer, but studies of their effectiveness have not yet been conducted.
Antiarrhythmic therapy is effective only in 60% of patients; in the rest, it is not possible to achieve a safe state only with the help of medications, and there is a need to correct the electrical activity of the heart using special devices.
Surgical intervention
The most effective way to prevent sudden death is the installation of a cardioverter-defibrillator, which is needed if:
- There are symptoms of SB;
- The course of the pathology is asymptomatic, but provocation causes ventricular fibrillation;
- When tested, the Brugada phenomenon type 1 occurs, and among relatives there have been cases of unexplained death at a young age.
According to world statistics, SB occurs much more often than it appears in the diagnoses of cardiologists. The low detection rate can be explained by a lack of vigilance on the part of doctors and the lack of convincing diagnostic criteria. Based on this, all patients with characteristic ECG changes, unexplained fainting, and an unfavorable family history of sudden death among young people need a thorough examination with ECG, Holter monitoring, and pharmacological tests. Relatives in families where there have already been cases of sudden death of young people also require increased attention.
Popular Articles Is a pulse of 50 beats per minute considered normal or not?
The study of Brugada syndrome continues, and to obtain high results, a sufficient number of observations is necessary, so experts are interested in identifying as many patients as possible in different countries.
To study pathology, a special International Brugada Syndrome Foundation has been created, where all persons suspected of this disease can be consulted free of charge and in absentia. If the diagnosis is confirmed, the patient will be included in a single list of patients who may in the future be subjected to genetic research in order to clarify the hereditary mechanisms of the development of the pathology.
Pathology Clinic
The peculiarity of the disease is that the signs of atrial fibrillation disappear against the background of transverse heart block. This makes it difficult to make a correct diagnosis. Patients do not have a feeling of rapid heartbeat, rhythm interruptions, but appear (loss of consciousness).
The insidiousness of Frederick's syndrome is that during the blockade the rhythm of contractions slows down, so a false impression is created that the condition is improving. Good health can remain for a long time.
But later, as the ventricular myocardium loses its ability to maintain rhythm, the patient’s condition deteriorates sharply. At a pulse rate of 20 to 30 contractions per minute, cerebral hypoxia develops, which can be fatal if there is a long pause between contractions.
Watch the video about atrioventricular block and its degree: