Peter Ullrich, neurosurgeon
He is a world-renowned expert in neurosurgery and performs all types of operations in complex areas of the brain, base of the skull or spinal cord
Read more about the specialist →
source: ©stockvault.net
In most cases, up to 85%, the disease is diagnosed in the anterior part of the brain: the internal carotid artery (ACI), anterior cerebral artery (ACA) and middle cerebral artery (MCA). Localization in the posterior part: in the basilar (a. basilaris) and posterior cerebral (PCA) arteries occurs much less frequently, namely in 15% of all cases.
About 3 in 100 people are diagnosed with a brain aneurysm . Some people develop multiple aneurysms. Most of them do not change, are asymptomatic and are most often diagnosed accidentally. Treatment in Germany for such pathologies consists of surgical exclusion of aneurysms from the bloodstream. However, not everyone is operable; when indicating surgical intervention, the following factors should be taken into account:
- individual clinical characteristics of the patient;
- risk of aneurysm rupture during life;
- localization of pathology;
- size and number of aneurysms;
- tone of blood vessels;
- risks of surgical treatment.
Methods for removing a cerebral aneurysm
If you don't have symptoms and are at increased risk of rupture, you don't necessarily need therapy. In such cases, regular diagnosis of brain aneurysm is carried out: control CT or MRI studies are prescribed over time every 1-3 years. However, the decision for or against prophylactic shutdown of the aneurysm is, of course, made by you, based on the doctor’s recommendation. Therefore, when choosing a clinic or doctor, the latter’s specialization and experience play a decisive role.
If a cerebral aneurysm ruptures, surgery is inevitable. The tactics of surgical access are chosen by the neurosurgeon himself. Today there are two methods:
- clipping - open craniotomy operation;
- coiling - endovascular embolization.
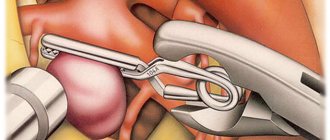
Clipping of a vascular aneurysm of the brain
A traditional method in which a neurosurgeon makes a hole in the skull. Through this hole, he identifies the artery on which the aneurysm has formed and clamps the neck of the aneurysm with a special titanium clip. This allows you to turn off the aneurysm from the bloodstream and prevent its further growth or rupture.
Open surgery is now rarely resorted to and only in extreme cases (with rupture and heavy hemorrhage), since after clipping of a cerebral aneurysm there is an increased risk of disability.
Boiling
Unlike open surgery, the endovascular method is minimally invasive and involves shutting off the cerebral aneurysm from the inside using miniature platinum coils and without opening the skull. The patient is hospitalized (registered as a hospitalist) as a rule, the day before surgery. On this day, routine preoperative procedures are performed:
- ECG;
- blood pressure measurement;
- blood analysis;
- diagnostic angiography.
Within the framework of the latter, the exact location, volume and shape of the aneurysm is determined, and a 3D image of the vessels is formed. This allows the neurosurgeon to design the course of the planned operation. During the operation itself, the patient is under general anesthesia, access is carried out through puncture of the femoral artery with the introduction of a cannula approximately 2-4 mm thick (guidewire) through it.
Then a catheter is inserted through it, allowing the vessel to be monitored, thereby controlling the progress of surgical procedures. In addition to the guidewire, a minicatheter with a diameter of up to 0.5 mm is also inserted there. With the help of the latter, direct access to the aneurysm is provided and the coiling itself is installed, that is, a spiral is formed from platinum wire with a diameter of up to 0.25 mm.
For large aneurysms, there may be several coils. This allows you to fill the saccular space of the aneurysm from the inside, until it is completely excluded from the bloodstream. After surgery, without blood supply, the cerebral aneurysm ceases to be active , no longer poses a risk of rupture, gradually becomes overgrown with connective tissue, and decreases in size until it completely dries out. If the vessel lumen is wide, a stent is installed first, and then coil embolization. This allows you to strengthen the fragile vessel and protect it from possible perforation during the coiling process. Upon completion of the operation, all auxiliary instruments are removed and the inguinal artery is closed. The patient spends one night in the intensive care unit and, in the absence of complaints, is discharged a day later.
A comment
Giant fusiform aneurysms of the main arteries of the brain represent a complex problem in the treatment of hemorrhagic stroke, challenging modern methods of vascular neurosurgery.
The article presents an interesting clinical case of treatment of this pathology using a rare variant of revascularization surgery - the creation of an extra-intracranial anastomosis between the superficial temporal and pericallosal arteries. A detailed description of the surgical technique is presented, and an interesting technique for intraoperative monitoring of evoked potentials is described in order to identify signs of the development of cerebral ischemia. However, the question arises about the advisability of performing revascularization in the given case, taking into account the signs of good collateral compensation of cerebral blood flow in the distal parts of the pericallosal artery. This is indicated by the patient’s well-tolerated long-term clamping of this artery—259 minutes—as well as the initially low values of volumetric blood flow through the shunt—18 ml/min. In this regard, the question also arises about the functioning of the anastomosis in the long-term postoperative period.
At the same time, the described option for successful surgical treatment of a giant fusiform aneurysm of the pericallous artery certainly arouses interest and allows specialists involved in the treatment of this pathology to expand the arsenal of possible surgical techniques.
Yu.V. Pilipenko (Moscow)
Cost of surgery to remove a cerebral aneurysm in Germany
Prices for regular diagnostics in Germany, rehabilitation and recovery after removal of an aneurysm are calculated based on the patient’s condition at the time of contacting the Nordwest clinic. You can consult a doctor to identify an aneurysm by signing up for a video consultation. The acute course of the disease requires immediate hospitalization. Patient relationship managers will provide you with assistance in organizing your treatment as soon as you contact them and go through all the stages of interaction. They will also be able to advise you how much the operation costs to prevent complications in the form of rupture or stroke if the diagnosis has already been established.
results
The results of patient treatment are presented in the table.
Results of treatment of patients with large and giant aneurysms of the SBB Note. OA - basilar artery, VA - vertebral artery, PICA - posterior inferior cerebellar artery, SMA - superior cerebellar artery, FD - flow diverter, flow-directing stent, AS - assisting stent, stent used for assistance.
In 7 patients, it was possible to achieve immediate exclusion of the aneurysm from the blood flow or a marked slowdown of blood flow in the aneurysm. In 6 cases, no increase in neurological symptoms was noted. In 1 patient with a combination of PICA aneurysm and AVM, increased diplopia was noted in the early postoperative period. A patient with a fusiform aneurysm of the middle and lower third of the trunk of the basilar artery, with a volumetric effect on the pons, was planned to implant a flow-directing stent into an assisting stent (with the aim of maximizing positioning of the flow-directing stent only in the area of the artery defect, assisting (in a relatively unchanged area) - the upper third main artery). In the early postoperative period (day 1), the patient developed symptoms of ischemic damage to the brain stem caused by thrombosis of the perforating branches of the basilar artery, which led to the patient’s death on the 3rd day after surgery.
In 2 cases, due to persistent symptoms, the second stage of surgery was performed, which consisted of decompressive trepanation of the posterior cranial fossa and removal of the aneurysm sac, which exerts a compressive effect on the brain stem (Fig. 2).
Rice. 2. Giant aneurysm of the right superior cerebellar artery. a, b, c — MRI in coronal, sagittal and axial projections, T1 mode V.I. A giant aneurysm sac is visualized, roughly compressing the brain stem; d — SCT angiography, the white arrow indicates the filling part of the aneurysm; d — stage of the operation to remove thrombotic masses from the aneurysm cavity. Intraoperative photo. AA—aneurysm sac, Cer—cerebellum; e — SCT of the brain after surgery, there is a significant decrease in the size of the aneurysmal sac with a decrease in trunk compression.
Long-term results were monitored in 5 patients from 3 to 48 months after surgery. In 4 patients there was almost complete regression of existing symptoms. According to control cerebral angiography, the aneurysm does not fill in 4 patients, and slight filling remains in 1 patient. All patients also underwent a control MRI of the brain, according to which a decrease in aneurysm size was noted in 3, and no change in size in 2.
Initial clinical manifestations of aneurysm rupture, acute extensive subarachnoid hemorrhage
During the short moment of aneurysm rupture, when extensive subarachnoid hemorrhage acutely develops, intracranial pressure reaches the value of mean arterial pressure, with a decrease in cerebral blood supply (CPP, cerebral perfusion pressure).
In 45% of cases, after this, patients suddenly lose consciousness, which is then restored. Sometimes a patient's sudden loss of consciousness is preceded by a short moment of excruciating headache, but most patients, upon regaining consciousness, first of all complain of a headache.
In 10% of cases, bleeding from a ruptured aneurysm can be quite massive and cause loss of consciousness in the patient for several days.
Approximately 45% of patients after a rupture of an aneurysm complain of intense headache, usually worsening with tension, but they do not experience loss of consciousness. Patients often describe this headache as “the worst headache of their entire life.” Designations such as “tearing” and “breaking” headaches are often used. Typically, patients indicate that they have pain in “the whole head” or “the back of the head and neck.”
Whatever the onset of the disease, one of its symptoms of aneurysm rupture is vomiting. When vomiting and sudden headache are combined, the patient should always suspect acute subarachnoid hemorrhage.
Although the hallmark of a ruptured aneurysm is sudden headache in the absence of focal neurological symptoms, patients often also experience neurological deficits.
Paralysis of the muscles innervated by the third oculomotor nerve that occurs in the patient on the side of the hemorrhage makes one think about a ruptured aneurysm of the posterior communicating artery.
The often observed paralysis of the rectus externus muscle of the eye (innervated by the abducens VI nerve) is of little importance for the location of the lesion, but is often observed with rupture of a subtentorial aneurysm.
When an aneurysm of the anterior communicating artery or bifurcation of the middle cerebral artery ruptures, blood flows into the subdural space or into the basal cisterns of the subarachnoid space, and the resulting blood clot can be quite large and cause a local mass effect. As a result, a neurological deficit develops, including weakness of the muscles of one half of the body (hemiparesis), speech disorder (aphasia) with damage to the dominant hemisphere, impaired recognition (hemitype anosognosia), and with damage to the non-dominant hemisphere - memory loss and abulia.
When an aneurysm, located at the bifurcation of the middle cerebral artery, ruptures, blood can enter the Sylvian cistern, the temporal lobe, or upward into the frontal and parietal lobes. Such hemorrhages may be characterized by manifestations of a volumetric process in the patient and may be mistaken by the doctor for intracerebral hemorrhages. Often the accompanying cerebral edema leads to aggravation of the patient’s condition, which in some cases requires emergency neurosurgical intervention.
Sometimes patients immediately after aneurysm rupture develop acute unilateral edema of the cerebral hemisphere, combined with focal neurological symptoms and stupor. The causes of this cerebral edema have not been established. It is possible that there is a transient cessation of cerebral circulation in this arterial basin, possibly secondary to vascular spasm in the area of the artery trunk. It is often difficult to explain the cause of a patient's initial neurological deficit, and in most cases symptoms regress over time. To determine the tactics of patient management and the time of occurrence and development of residual neurological symptoms, careful documentation of the initial neurological deficit is of great importance. This is necessary to find out its cause, as well as carefully monitor its dynamics.
Subarachnoid hemorrhage severity rating scale:
Degree | Hunt-Hess scale | Glasgow Coma Scale (GCS) |
| 1 | Moderate headache, clear consciousness, cranial nerves and motor functions are not impaired | GCS score 15, without motor deficit |
| 2 | Severe headache, clear consciousness, possible dysfunction of cranial nerves | 13–14 GCS points, without motor deficit |
| 3 | Drowsiness, confusion, possible cranial nerve dysfunction or mild motor deficits | 13–14 GCS points, presence of motor deficit |
| 4 | Stupor (lethargy), moderate or severe motor deficit, possible intermittent reflex muscle hypertonicity | GCS score 7–12, with or without motor deficit |
| 5 | Coma, reflex hypertonicity or muscle flaccidity | GCS score 3–6, with or without motor deficit |
In case of subarachnoid hemorrhage, the initial clinical manifestations of aneurysm rupture can be assessed using the Hunt-Hess scale or the Glasgow Coma Scale (GCS) of the World Association of Societies of Neurosurgeons. When an aneurysm ruptures, the patient's prognosis worsens as the grade on this scale increases. For example, for patients scoring 1 on the Hunt-Hess scale, death is not typical if the ruptured aneurysm was treated in a timely manner. At the same time, the mortality rate of patients with grade 4 or 5 on the Hunt-Hess scale can be above 80%.
Clinical manifestations of complications in subarachnoid hemorrhage
After suffering a subarachnoid hemorrhage due to a rupture of a cerebral artery aneurysm, the patient may experience complications. Such complications include:
- thrombophlebitis with pulmonary embolism
- stress-induced perforated duodenal ulcer
- ECG changes indicating myocardial infarction or ischemia
Subarachnoid hemorrhage in the cranial cavity triggers increased activity of the sympathetic nervous system. This causes myofibrillar degeneration of the heart muscle (myocardium). When an aneurysm ruptures with subarachnoid hemorrhage, cardiac arrhythmia may develop. For such patients, beta-blockers are recommended. Their use in patients should be carried out with caution, especially in the presence of atrioventricular block. A possible complication for the patient is a decrease in the level of sodium in the blood plasma (hyponatremia). Hyponatremia occurs when there is inappropriate secretion of antidiuretic hormone (ADH) or secretion of natriuretic hormone. Treatment of such patients is limited to free fluid restriction while maintaining sufficient intravascular volume.