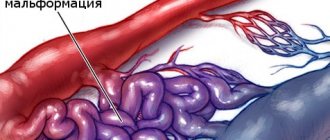
Arnold-Chiari malformation is an abnormal anatomical relationship of the bone structures of the upper part of the spine, the occipital part and the base of the skull with the lower part of the brain. Normally, the medulla oblongata, pons and cerebellum are located inside the cranium. And the brain smoothly transforms into the spinal cord at the level of the foramen magnum. In it, the nervous structures, vertebral arteries and liquor pathways are located freely.
With Arnold-Chiari malformation, part of the terminal parts of the brain extends beyond the skull and descends into the opening of the skull. As a result, the tissues of the brain, cervical spinal cord, vertebral arteries and liquor-conducting tracts are compressed. As a rule, this is a congenital pathology, less often it is a consequence of traumatic brain injuries suffered at an early age, which disrupted the correct formation of the bones of the posterior cranial fossa. The anomaly is often combined with other defects - syringomyelic syndrome, cleft vertebrae. The prevalence of clinically significant and severe forms is thousandths of a percent.
The clinical picture depends on the type of anomaly and dysfunction of the compressed structures. The course ranges from asymptomatic to incompatible with life, depending on the type.
Definition
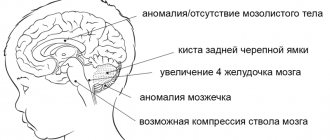
Arnold Chiari syndrome type I consists of the descent of the lower part of the cerebellum - the cerebellar tonsils - into the foramen magnum and spinal canal in the absence of other malformations associated with the spinal cord. Sometimes it is believed that the prolapse of the cerebellar tonsils should be more than 5 mm, sometimes more than 3 mm, for others the prolapse begins at 0 mm, when the tonsils are at the level of the border of the foramen magnum, in the presence of an appropriate clinical picture.
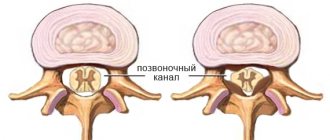
Figure 1.- The diagram shows the descent of the cerebellar tonsils and the increase in the supracerebellar space due to the displacement of the entire cerebellum towards the foramen magnum. Arnold Chiari I syndrome.
Tests and diagnostics
At the first signs, it is necessary to undergo a neurological examination and assess the severity of clinical and functional disorders. To confirm the diagnosis, the following are most often used:
- neuroimaging techniques, most preferably MRI;
- electroencephalography;
- radiography of the skull;
- myelography , which allows you to identify defects in the upper cervical spinal cord, brain stem, as well as the localization of the cerebellum below the Chamberlain line in the foramen magnum.
MRI results for Arnold Chiari malformation with syringomyelic cyst and normal
Symptoms
The clinical picture of Arnold Chiari I syndrome can be varied, the most common symptoms (from more frequent to rarer): headaches, pain in the cervical spine, paresis in the limbs, visual impairment, pain in the limbs, paresthesia, sensory disturbances, dizziness, swallowing disorders, lower back pain, memory impairment, gait disturbance, pain in the thoracic spine, imbalance, dysesthesia, difficulty expressing thoughts and finding words, sphincter disorders, insomnia, vomiting, loss of consciousness, trembling.
Symptoms and clinical picture
Many people suffering from this developmental pathology may not even be aware of its presence. Usually, they are diagnosed accidentally and do not require any treatment.
The remaining patients have more or less severe symptoms of the disease. The disease is accompanied by pain in the cervical-occipital region of the head, which tends to intensify with coughing, hiccups, and also with sneezing. A neurologist finds a decrease or complete absence of pain and temperature sensitivity of the upper extremities, muscle weakness and spasticity of the extremities. Also, fainting and dizziness are observed, there may be decreased vision, episodic apnea, and involuntary rapid eye movement. An increase in intracranial pressure is characterized by morning pain in the head, a feeling of hissing and ringing in the ears. Deterioration in coordination is manifested by tremor of the upper or lower extremities. As the disease progresses, the patient develops problems with urination, weakness and general fatigue increase. During movement, the clinical picture becomes more vivid.
Arnold Chiari types
There are 4 classical types (I, II, III, IV) and two recently described types (“0”, “1.5”):
Type I Prolapse of the cerebellar tonsils without any other malformation of the nervous system.
Type II Cerebellar tonsil prolapse with a neurovertebral malformation in which the spinal cord is attached to the spinal canal.
III type. Cerebellar tonsil prolapse with occipital encephalocele and cerebral abnormalities in Arnold Chiari II syndrome.
IV type. Dropping of the cerebellar tonsils, aplasia or hypoplasia of the cerebellum associated with aplasia of the tentorium.
“0” type Currently, cases of a clinical picture characteristic of Arnold Chiari Syndrome I, without prolapse of the cerebellar tonsils, have been reported.
“1.5” type. Recently, Arnold Chiari Syndrome 1.5 has been described with descent of the cerebellar tonsils and descent of the brain stem into the foramen magnum.
Treatment
In asymptomatic cases, constant monitoring with regular ultrasound and radiographic examination is indicated. If the only sign of an abnormality is minor pain, the patient is prescribed conservative treatment. It includes a variety of options using non-steroidal anti-inflammatory drugs and muscle relaxants. The most common NSAIDs include Ibuprofen and Diclofenac.
You cannot prescribe painkillers yourself, as they have a number of contraindications (for example, peptic ulcer). If there is any contraindication, the doctor will select an alternative treatment option. Dehydration therapy is prescribed from time to time. If there is no effect from such treatment within two to three months, surgery is performed (expansion of the foramen magnum, removal of the vertebral arch, etc.). In this case, a strictly individual approach is required to avoid both unnecessary intervention and delays in surgery.
Treatment tactics for each patient require an individual approach
In some patients, surgical exploration is the way to make a definitive diagnosis. The purpose of the intervention is to eliminate compression of the nerve structures and normalize cerebrospinal fluid dynamics. This treatment results in significant improvement in two to three patients. The expansion of the cranial fossa helps to eliminate headaches and restore tactility and mobility.
A favorable prognostic sign is the location of the cerebellum above the C1 vertebra and the presence of only cerebellar symptoms. Relapses may occur within three years after the intervention. Such patients are assigned a disability by decision of the medical and social commission.
Theories about the cause of cerebellar tonsil prolapse
Prolapse of the cerebellar tonsils can be the result of the tension that a particular malformation places on the spinal cord, with the exception of Arnold Chiari syndrome type I, in which prolapse of the cerebellar tonsils is the only disorder, and there are different theories about the cause of this disorder:
– Traditional theories:
- Hydrodynamic: prolapse of the cerebellar tonsils is a consequence of impaired circulation of the cerebrospinal fluid.
- Malformation: The theory about the small size of the foramen magnum, which provokes the descent of the tonsils into the spinal canal.
– The theory of spinal cord tension according to Filum System ®:
Dr. Miguel B. Royo Salvador's theory views the prolapse of the cerebellar tonsils in Arnold Chiari Syndrome I as a result of abnormal tension on the spinal cord due to an abnormal and tight ligament called the filum terminale. The terminal filament is not visible in the photographs.
Figure 2. - MRI of the patient at 8 and 20 months, in the second image you can observe the prolapse of the cerebellar tonsils, which appeared after the first MRI. Huang P. “Adquired” Chiari I malformation. J. Neurosurg 1994. This indicates that, in addition to the hereditary and genetic factor, there is a factor of acquired disease.
Causes
The etiology is not reliably known. According to some neurologists, the appearance of Arnold Chiari malformation in a child is due to a decrease in the size of the cranial fossa, which predisposes structures to exit through the hole as they grow. Other experts associate the pathology with an increase in the size of the brain, which contributes to the pushing out of the contents of the cranium.
Hydrocephalus, characterized by dilatation of the ventricles, provokes an increase in the clinical picture. The manifestation of the disease can be caused by a traumatic brain injury, aggravating the herniation. This is due to improper development of the bone structures of the corresponding area.
Factors influencing the development of Arnold Chiari I Syndrome
The main factors involved in the development of Arnold Chiari Syndrome I are as follows:
- Family Predisposition: Tension of the nervous system due to an abnormally tight filum terminale, which we call filum terminale disease, leads to prolapse of the cerebellar tonsils. This pathology is genetic and can be inherited.
- Sudden increase in tension on the spinal cord: After a fall or spinal injury, existing tension on the spinal cord—filum terminale disease—may increase. In these cases, due to the stronger tension, the descent of the cerebellar tonsils or compression in the foramen magnum may increase, which will affect the growth of symptoms. Trauma, in this case, is not the cause of the development of Arnold Chiari syndrome, it is only a trigger for a sudden deterioration of the condition due to an increase in tension force.
Pathogenesis
The pathophysiology is usually based on a discrepancy between the size of the posterior cranial fossa and the structures of the nervous system present in it, as well as:
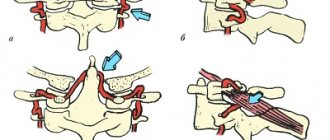
- development of anomalies of the cervical vertebral bodies, including their splitting, most often of the first (this development mechanism occurs in 5% of cases), assimilation of the atlas - fusion of the cervical vertebra with the occipital bone;
- displacement of the cerebellar structures during the period of rapid brain growth with slowly growing skull bones;
- hydrocephalus – excessive accumulation of cerebrospinal fluid;
- syringomyelia is an abnormal process of development of cavities in the spinal cord;
- myelomeningocele – a congenital defect in the development of the neural tube;
- various congenital diseases, including platybasia , Dandy-Walker anomaly .
Complications of Arnold Chiari Syndrome I
Complications from prolapse of the cerebellar tonsils may depend on the degree of tension or on tissue compression in the occipital region (compression of the tissues of the cerebellar tonsils and the spinal cord stem due to limited space in the occipital space).
- Deterioration in quality of life: with Arnold Chiari I syndrome, headaches, dizziness, pain in the back and limbs, paresis, swallowing or sensitivity disorders, cognitive impairment, visual or gait disturbances can become chronic, increase in intensity, each time worsening the patient’s condition, limiting it normal lifestyle.
- Chronic pain: Patients may need treatment in a pain management unit because conventional anti-inflammatory and pain medications may not be effective in treating headache attacks and other symptoms.
- Sudden death: the spinal cord stem controls cardiorespiratory functions; if the cerebellar tonsils put pressure on it, breathing disorders (apnea, respiratory arrest, and even sudden death of the patient) may occur during sleep. That is why timely diagnosis and early treatment are so important.
In children
The block most commonly noted is within the ventricular system and is noncommunicating hydrocephalus . This is usually caused by a narrowing of the Sylvian aqueduct or underdevelopment of the foramina of Magendie and Luschka. As a generalized disorder of the development of the nervous system, it can be combined with micro- or macrogyria, porencephaly, agenesis of the corpus callosum, fusion of the cerebral hemispheres, agenesis of the cerebellar vermis, vertebral clefts, meningocele, encephalocele, syringomyelia, hydromyelia . The cause of communicating hydrocephalus may be the formation of adhesions in the subarachnoid region at the base of the brain, perinatal subarachnoid or intraventricular hemorrhages.
The syndrome in children can occur as a result of traumatic injuries to the sphenoid-occipital and sphenoid-ethmoid region due to birth injuries. Clinical manifestations include feeding disorders ( reflux and aspiration ), episodes of apnea , stridor , cranial innervation disorders, and seizures resistant to anticonvulsants.
Arnold Chiari syndrome in the fetus
Chiari pathology is a congenital osteoneuropathy and is formed at the stage of formation and development of the neural tube in the fetus, asynchronous formation of the nerve trunk and bones of the cranial fossa.
The morphological manifestations of this pathology can be identified during an ultrasound examination and determine the further prognosis. Most often, the detection of pathology becomes the reason for termination of pregnancy.
Treatment of Arnold Chiari Syndrome I
Typically, neurosurgical treatment is used for Arnold Chiari Syndrome I with/without syringomyelia. Currently, decompression or craniotomy of the foramen magnum is the standard treatment for this diagnosis in most medical centers in the world. It is usually prescribed in cases where the symptoms cause more damage and mortality than the natural progression of the pathology.
However, since 1993, after the publication of the doctoral dissertation of Dr. Royo Salvador, who linked the tension of the entire nervous system with the filum terminale, the tension of which provokes, among other diseases, the prolapse of the cerebellar tonsils, a new treatment was developed, etiological, that is, eliminating the cause of the disease with surgical dissection of the filum terminale, which removes the pathological tension mechanism.
Our technique of filum terminale dissection is minimally invasive and is prescribed in all cases of filum terminale disease, both symptomatic and asymptomatic, and as early as possible, since the risks are minimal and much lower than from the pathology itself, in addition, this treatment stops further development of the disease.
Cutting the filum terminale with the Filum System® technique:
Advantages
1. Eliminates the cause of Arnold Chiari Syndrome I and associated pathologies.
2. Eliminates pressure in the foramen magnum and with it the risk of sudden death.
3. 0% mortality, without consequences in more than 1500 patients operated on using the Filum System® method.
4. With minimally invasive technique, surgical time: 45 minutes. Short stay in the clinic. Local anesthesia. Short period of post-operative recovery without restrictions.
5. Improves symptoms, stops the prolapse of the cerebellar tonsils.
6. Eliminates the risk of hydrocephalus due to prolapse of the tonsils.
7. Improves blood supply to the entire nervous system and, at the same time, cognitive capabilities, which may suffer due to spinal cord tension.
Flaws
1. A small suture in the coccyx area; complications such as suture infection and hematoma in the operation area are possible.
2. Improvement in spasticity is sometimes mistaken for decreased strength in the limbs.
3. During the process of restoration and improvement of sensitivity, unpleasant sensations may appear, which are usually mistaken for undesirable consequences.
4. With improved blood supply to the brain, brain activity may increase and mood swings may occur during the initial post-operative period.
Occipital craniectomy:
(Decompression of the foramen magnum)
Advantages
1. Avoiding the risk of sudden death.
2. The condition of some patients improves.
Flaws
1. Does not eliminate the cause of the disease.
2. Mortality from 0.7 to 12%, a higher percentage than sudden death with spontaneous development of the disease.
3. Aggressive surgery, crippling and possible consequences.
4. Small percentage of improvement and for a short period of time.
5. Neurological deficit: depends on the location of the injury: Emiparesia (paralysis of half the body from 0.5 to 2.1%. Changes in visual space from 0.2 to 1.4%. Changes in speech from 0.4 to 1%. Lack of sensitivity from 0.3 to 1%. Lack of balance, difficulty walking from 10 to 30%.
6. Postoperative intracerebral hemorrhage in the operated area, epidural hematoma, intra-axial hemorrhage, which can cause neurological deficit or worsening of a pre-existing deficit (0.1 to 5%).
7. Brain edema, depending on the process and situation, the risk reaches 5%.
8. Superficial, deep or intracranial infection, risk from 0.1 to 6.8%, with the formation of a brain abscess, aseptic-septic meningitis.
9. Hemodynamic changes due to manipulation of brain stem disorders.
10. Gas embolism (in patients in a sitting position).
11. Cerebrospinal fluid output is from 3 to 14% (cerebrospinal fluid fistula).
12. Postoperative hydrocephalus.
13. Pneumoencephaly
14. Tetraparesis (loss of strength in all limbs)
Due to the morbidity and mortality associated with occipital decompression, which exceeds the mortality associated with spontaneous development of Arnold Chiari I syndrome, we believe that this treatment is contraindicated.
Symptoms of the disease
If we talk about the clinical manifestations of the disease, then most often we have to remember the pathology of the 1st degree. Its first manifestations can make themselves felt only during puberty; changes are often noticed by older people. As is the case with other brain pathologies, the first signal and cause for concern may be a headache, especially if it does not disappear even after exposure to painkillers. By the way, the symptoms may vary depending on the physical condition of the person, his gender and age, but quite often these are a shaky gait, problems with fine motor skills of the hands (the inability to perform basic housework), numbness of the limbs, pain in the neck area.
Diagnosing Arnold-Chiari malformation is a very difficult task, but it can be solved, and modern diagnostic methods come to the rescue, including computed tomography and magnetic resonance imaging, and MRI is especially effective in this case. A routine neurological examination will only determine the presence of hydrocephalus (high intracranial pressure). In this case, X-rays are also powerless, recording only a violation of the condition of the skull. Quite often the disease does not manifest itself, so the diagnosis is not always made in a timely manner, just as the treatment of Arnold-Chiari malformation is not started in a timely manner. In Moscow, many institutions are engaged in this, but the best results are demonstrated by specialists from the oldest neurosurgical institution - the Scientific and Practical Center named after. Burdenko.
BIBLIOGRAFIA
- Dr. Miguel B. Royo Salvador (1996), Siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas, etiología común (PDF). REV NEUROL (Barc); 24 (132): 937-959.
- Dr. Miguel B. Royo Salvador (1996), Platibasia , impresión basilar, retroceso odontoideo y kinking del tronco cerebral, etiología común con la siringomielia , escoliosis y malformación de Arnold-Chiari idiopáticas (PDF). REV NEUROL (Barc); 24 (134): 1241-1250
- Dr. Miguel B. Royo Salvador (1997), Nuevo tratamiento quirúrgico para la siringomielia , la escoliosis , la malformación de Arnold-Chiari , el kinking del tronco cerebral, el retroceso odontoideo, la impresión basilar y la platibasia idiopáticas (PDF). REV NEUROL; 25 (140): 523-530
- M. B. Royo-Salvador, J. Solé-Llenas, J. M. Doménech, and R. González-Adrio, (2005) “Results of the section of the filum terminale in 20 patients with syringomyelia , scoliosis and Chiari malformation .” (PDF). Acta Neurochir (Wien) 147:515–523.
- M. B. Royo-Salvador (2014), “Filum System® Bibliography” (PDF).
- MB Royo-Salvador (2014), “A Brief Introduction to the Filum System®.”
Arnold Chiari syndrome I
Described: In 1883 by the anatomist surgeon John Cleland (1835-1925) from Perthshire, Scotland.
He described elongation of the cerebellar vermis, prolapse of the cerebellum and fourth ventricle in a boy with hydrocephalus, encephalosceles, and spina bifida. In 1891 and 1896, Hans Chiari described new cases and classified them. In 1894, Jules Arnold contributed to the spread of knowledge about this disease. Named: Schwalbe and Gredig in 1907 as “Arnold-Chiari malformation.” The official modern nomenclature in the codification and classification of diseases of the World Health Organization calls this disease the term “Arnold-Chiari syndrome or disease I” (Q07.0, CIE-10). (WHO, (International Statistical Classification of Diseases and Related Health Problems, 10th Revision (c) Geneva, OMS, 1992)).
Frequency: One case per thousand newborns, other authors indicate less than 1% of the population. In both cases, we are talking about prolapse of the cerebellar tonsils by more than 3 or 5 mm.
Filum terminale disease
After the research of Dr. Royo Salvador and his doctoral dissertation (1992), it was found that several diseases whose cause was previously unknown, such as: Arnold Chiari I syndrome, idiopathic Syringomyelia and Scoliosis, Platybasia, Basilar Impression, Axial vertebral tooth displacement, An angular bend at the level of the arch of the atlas is part of a new pathology - Diseases of the filum terminale - and arises for the same reason: tension in the spinal cord and the entire nervous system.
The tension force of the entire nervous system during filum terminale disease is present during the formation of all human embryos; to a greater or lesser extent, everyone suffers from its consequences and various forms of manifestation and intensity.
The following diseases may be associated with filum terminale disease: intervertebral hernias, some cerebrovascular insufficiency syndromes, facet syndrome, Bostrup syndrome, fibromyalgia, chronic fatigue, nocturnal enuresis, urinary incontinence and acute paraparesis.
For accurate diagnosis, selection of treatment and monitoring of a patient with filum terminale disease, the Filum System® method was created.
Diagnostics
The diagnosis of type 1 anomaly is not accompanied by spinal cord damage and is made mainly in adults using CT and MRI. According to the pathoanatomical autopsy, in children with spinal canal hernia, Chiari disease of the second type is detected in most cases (96–100%). Using ultrasound, you can determine disturbances in the circulation of cerebrospinal fluid. Normally, cerebrospinal fluid circulates easily in the subarachnoid space.
Downward displacement of the tonsils impedes circulation. Due to impaired fluid dynamics, hydrocephalus occurs.
Lateral X-ray and MR picture of the skull shows the expansion of the spinal canal at the level of C1 and C2. On angiography of the carotid arteries, the cerebellar artery bends around the tonsil. X-rays show concomitant changes in the craniovertebral region, such as underdevelopment of the atlas, odontoid process of the epistrophe, and shortening of the atlanto-occipital distance.
With syringomyelia, a lateral X-ray image shows underdevelopment of the posterior arch of the atlas, underdevelopment of the second cervical vertebra, deformation of the foramen magnum, hypoplasia of the lateral parts of the atlas, enlargement of the spinal canal at the C1-C2 level. Additionally, MRI and invasive x-ray examination should be performed.
MRI is the most preferred diagnostic method
The manifestation of symptoms of the disease in adults and the elderly often becomes the reason for identifying tumors of the posterior cranial fossa or craniospinal region. In some cases, the patient’s external manifestations help to make a correct diagnosis: low hairline, shortened neck, etc., as well as the presence of craniospinal signs of bone changes on X-rays, CT and MRI.
Today, the “gold standard” for diagnosing the disorder is MRI of the brain and cervicothoracic region. It is possible to perform intrauterine ultrasound diagnostics. Possible ECHO signs of abnormality include internal dropsy, a lemon-shaped head, and a banana-shaped cerebellum. At the same time, some experts do not consider such manifestations to be specific.
To clarify the diagnosis, different scanning planes are used, thanks to which several informative symptoms in the fetus can be detected regarding the disease. Obtaining an image during pregnancy is quite easy. In view of this, ultrasound remains one of the main scanning options to exclude pathology in the fetus in the second and third trimesters.
Identification of signs of the disease in the fetus can be an indication to exclude malformations of the spinal column, however, even the absolute absence of ultrasound data indicates spina bifida in 95% of cases.