Budd-Chiari syndrome is a blockage of the hepatic veins that leads to impaired blood flow. It is provoked by changes in the structure of blood vessels or secondary diseases of the cardiovascular system. This rare pathology occurs in acute or chronic form. Budd-Chiari disease is manifested by nausea, enlarged liver (hepatomegaly), pain in the right side, weakness, abdominal dropsy, lethargy, yellowing of the skin and eyeballs. The prognosis for recovery depends on how quickly the surgery is performed.
Causes of the disease
Budd-Chiari syndrome or disease is a pathological condition characterized by venous stagnation due to a decrease in the lumen of the hepatic vessels. The pathology is diagnosed in 1 person per 100 thousand population. Women aged 40-50 years are more susceptible to it than others. In 18% of cases, the syndrome is provoked by pathologies of the hepatobiliary system - liver, gallbladder and ducts. In 1/3 of patients, the cause of thrombosis of the mesenteric (mesenteric) vessels cannot be identified.
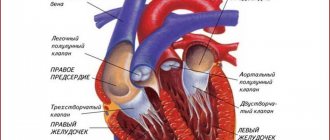
The portal system of the liver collects blood from the unpaired organs of the peritoneum:
- pancreas;
- stomach;
- spleen.
Congenital and acquired vascular diseases lead to a slowdown in venous blood flow, which affects the functioning of many internal organs.
Depending on the origin, the syndrome is:
- Primary – a consequence of congenital pathologies of the cardiovascular system. Occurs when there is stenosis or damage to the hepatic vessels. Most often found in people living in Japan and African countries.
- Secondary is the result of structural changes in the vessels of the portal system of the liver against the background of acquired pathologies. Budd-Chiari syndrome complicates the course of pericarditis, cancer of the peritoneal organs, peritonitis, and cirrhosis of the liver.
Disruption of venous blood flow is the main cause of the clinical syndrome.
Due to the increase in hydrostatic pressure in the portal vein basin, portal hypertension is diagnosed. Depending on the rate of progression, there are 2 forms of Budd-Chiari syndrome:
- Acute – accompanied by vivid symptoms. The liver increases in volume and acquires a bluish tint. Due to stagnation of blood, the central lobes of the organ are affected, which leads to thrombosis of the central vein, congestive cirrhosis.
- Chronic – the clinical picture is erased. The walls of the liver vessels thicken. Gradually they become clogged with blood clots. If left untreated, the vessels become overgrown, transforming into fibrous cords.
Phlebologists and hepatologists identify a number of factors that provoke the syndrome:
- injuries of the peritoneal organs;
- malignant tumors;
- chronic inflammation of the liver;
- infectious diseases;
- pregnancy;
- cardiovascular pathologies;
- abuse of certain drugs.
Concomitant pathologies provoke obstruction (blockage) of the liver veins, which leads to damage to its tissue (parenchyma). Due to venous stagnation, intrahepatic pressure increases, which causes necrosis (death) of hepatocytes.
When the vessels in the portal vein are blocked, the outflow of blood is provided by the paravertebral and intercostal veins. But they cannot cope with excessive loads, resulting in serious complications.
In the last stages of the syndrome, the parenchyma in the peripheral areas of the liver becomes thinner, and in the central area it thickens. Due to the increase in its volume, the inferior vena cava is compressed, which aggravates the course of the disease.
1.General information
As you know, inflammatory processes can develop in almost any organ and any tissue. Inflammation of the inner walls of blood vessels is called endovasculitis; A special case is endophlebitis, if the walls of a vein or several veins become inflamed. The diagnosis of “obliterating endophlebitis” implies a tendency to narrowing of the lumen against the background (and as a result) of inflammation, which, in turn, entails disturbances in venous outflow, possible thrombosis and other serious complications.
Obliterating endophlebitis, affecting the hepatic veins (in the area of their confluence with the inferior vena cava), received the name “Budd-Chiari disease”. This is a primary, independent disease, usually caused by congenital anomalies in the structure of blood vessels. Separately, we consider the secondary symptom complex, which also occurs when there are disturbances in the venous outflow of blood from the liver and is clinically similar to Budd-Chiari disease, but is not associated with organic changes in the veins. This condition is called Budd-Chiari syndrome.
Both Budd-Chiari disease and the syndrome of the same name are rare. Some sources report a predominance of women among those affected. It has long been proposed that the syndrome and Budd-Chiari disease be considered as a single disease; in ICD-10, in particular, only the syndrome is mentioned, and the term “Budd-Chiari disease” is absent. However, there are also those specialists who continue to separate these concepts who have their own reasons (see above).
A must read! Help with treatment and hospitalization!
Symptoms
Signs of the syndrome depend on the number of pathologically altered hepatic vessels. In some, obstruction occurs in the area of the inferior vena cava, in others - at the level of the large or small veins of the liver.
The severity of the clinical picture depends on the form of the pathology. The most dangerous is acute, which progresses quickly and causes serious complications.
When one small vessel is affected, the syndrome is asymptomatic. In the case of stenosis of two or more veins, hydrostatic pressure in the bloodstream increases, which affects the functioning of the liver and peritoneal organs.
Symptoms of Budd-Chiari syndrome:
- nausea;
- gagging;
- liver enlargement;
- fast saturation;
- pain in the right side;
- yellowness and itching of the skin.
When the vena cava is obstructed, the limbs swell and subcutaneous vessels appear. After a few days, kidney failure occurs, which is characterized by:
- decrease in daily diuresis;
- lethargy;
- lack of appetite;
- drowsiness;
- smell of ammonia from the mouth.
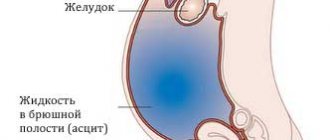
In the subacute course of the syndrome, blood clotting increases, which increases the risk of thrombus formation in the liver vessels. Due to stagnation of blood, the spleen enlarges, ascites appears, that is, intercellular fluid accumulates in the abdominal cavity.
People with indolent syndrome have almost no clinical manifestations. In rare cases, the following are noted:
- increased fatigue;
- liver enlargement;
- decreased performance.
When two liver veins are obstructed, the symptoms gradually increase. There are complaints of pain in the right hypochondrium and vomiting. At the height of the disease, cirrhotic changes in the liver and digestive disorders are detected.
In hepatology, isolated cases of the fulminant course of the syndrome are described, in which patients developed jaundice, abdominal dropsy, liver and kidney failure in a matter of days.
How is it diagnosed?
Budd-Chiari syndrome is indicated by a triad of signs - abdominal pain, abdominal hydrops, liver enlargement. To make an accurate diagnosis, a number of additional studies are prescribed:
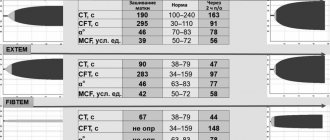
- Blood chemistry. The pathological syndrome is indicated by increased activity of liver enzymes - AST and ALT.
- Clinical blood test. Stagnation of venous blood is indicated by an increased ESR, and inflammation of the liver is indicated by an excess of leukocytes.
- Coagulogram. Against the background of changes in the rheological properties of blood, an increase in prothrombin time is noted.
- Ultrasound of the liver. Using echo signs, the degree of damage to the liver parenchyma, the size of the organ and the severity of vascular disorders are assessed.
To identify stenosis of the liver veins, MRI and portography are performed. Based on the data obtained, the doctor distinguishes Budd-Chiari syndrome from myocardial insufficiency and veno-occlusive pathology.
Diagnosis of Budd-Chiari disease
Diagnosis of Budd-Chiari syndrome is based on ultrasound data, revealing the characteristic nodular structure of the liver and congestion. A Doppler study (ultrasound examination of blood flow velocity) is also necessary to confirm disturbances in venous outflow from the liver.
Since nodules in the liver can be a manifestation of a malignant neoplasm, additional studies are carried out to exclude oncological pathology (analysis for the level of alpha-fetoprotein, liver biopsy). To accurately determine the anatomy of the lesion in the venous system, venography may be recommended - an examination in which contrast is injected directly into the hepatic vein system. Next, a series of x-rays are taken or a computed tomography scan is performed.
Treatment
Budd-Chiari disease is treated exclusively in a hospital using medication and surgical techniques. Complex therapy has several goals:
- eliminating blockage of veins;
- maintaining liver function;
- prevention of complications;
- normalization of blood pressure in the portal vein basin.
To restore venous blood flow and relieve symptoms, the following are used:
- anticoagulants (Novoparin, Fragmin) - reduce blood clotting, prevent the formation of blood clots in the hepatic veins;
- diuretics (Lasix, Furosemide) – remove excess fluid from the body, lower blood pressure, reducing the severity of portal hypertension;
- thrombolytics (Streptase, Actilyse) - dissolve blood clots in the systemic circulation, prevent thrombus formation.
Medicines only make you feel better, but do not lead to a complete recovery.
Mortality rates with drugs alone reach 85%. To restore blood circulation in the portal vein basin, surgery is needed. The extent of intervention depends on the location of the stenosis and the extent of the blood clots:
- Angioplasty is an operation to install a stent in a narrowed area of the inferior vena cava. At the preparation stage, balloon dilatation is performed to expand the vessel, after which an elastic metal-plastic cylinder is installed into it. It prevents re-narrowing and fusion of the vein.
- Bypass surgery is an operation to create artificial pathways for blood outflow. To reduce the pressure in the portal vein basin, portosystemic shunting is performed.
- Liver transplant – transplantation of a donor organ. The operation is performed for irreversible changes in the hepatic vessels or parenchyma. Patient survival rates range from 50% to 95%.
Additional therapeutic techniques are used depending on complications. To prevent internal bleeding, beta-blockers are prescribed. When the veins of the esophagus are dilated, their ligation with elastic rings is indicated. Patients with abdominal dropsy follow a salt-free diet.
4.Treatment
Conservative therapy includes the prescription of hepatoprotectors, anticoagulants, diuretics, and hormonal anti-inflammatory drugs. However, all these measures are usually ineffective; The mortality rate with drug treatment alone reaches 90%. Thus, the method of choice is vascular surgery (bypass surgery, angioplasty), but in this case the prognosis and surgical plan vary widely depending on the etiopathogenetic and clinical features of a particular case.
Possible complications and prognosis
In most cases, the prognosis is unfavorable. The effectiveness of treatment depends on:
- severity of liver dysfunction;
- age;
- causes of the syndrome;
- localization of stenosis;
- course of the pathology.
In the absence of adequate therapy, patients die within 3 to 36 months from the onset of symptoms. In all patients without exception, Budd-Chiari syndrome causes portal hypertension. Stagnation of venous blood provokes:
- liver failure;
- jaundice;
- dilation of the veins of the esophagus;
- bleeding from the gastrointestinal tract;
- ascites;
- hepatic encephalopathy;
- congestive cirrhosis;
- hepatocellular carcinoma.
The ten-year survival rate does not exceed 55%.
Prognosis worsens with cancer pathologies and myocardial failure. Budd-Chiari syndrome or disease is a rare pathology characterized by venous stasis. With inadequate or absent treatment, it is complicated by portal hypertension and cirrhosis. With a sluggish form of the syndrome, timely diagnosis and surgical intervention, it is possible to significantly prolong life.
2. Reasons
Idiopathic Budd-Chiari disease is caused by purely individual characteristics and abnormalities in the development of the vascular system. Risk factors include abdominal trauma, hematological diseases, gestation and childbirth, previous surgical operations, vasculitis, long-term use of certain medications (eg, hormone-containing contraceptives).
Secondary Budd-Chiari syndrome develops, by definition, against the background of more general severe diseases - with oncological processes, peritonitis, liver cirrhosis, coagulopathies and other blood diseases, systemic infections, pathology of the inferior vena cava, etc.
In approximately 25-30% of cases, the cause of obliterating endophlebitis cannot be established.
Visit our Gastroenterology page