Author: Sozinova A.V., obstetrician-gynecologist, has been in continuous practice since 2001. January, 2021.
Synonyms: platelets, platelet count, PC, plt.
Platelets are blood cells, and their concentration is determined during a general blood test. On the CBC form, platelets are designated as platelet count or PC. Blood for studying its composition, including counting the number of platelets, is taken from a finger (capillary) or from a vein. The unit of measurement for platelets is the number (N) of cells multiplied by 109 per liter.
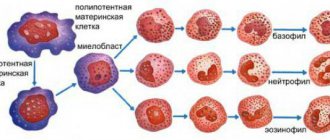
Platelets, like other formed elements, are formed in the red bone marrow. Their lifespan in the bloodstream is about 7–12 days. Destruction and breakdown of cells occurs in the spleen and liver tissues.
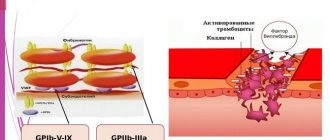
The main function of platelets is to carry out hemostasis, that is, to stop bleeding. Contact with damaged tissues causes transformation of cells, up to 10 processes are formed in them, and when they spread, the wound is closed with a platelet mass (thrombus). Thus, platelets prevent large amounts of blood from leaking out of damaged soft tissues.
Another equally important function of platelets is to protect the injured area from the penetration of pathogenic microorganisms (they secrete lysozyme and B-lysine).
Platelets also participate in the processes of hemostasis (maintaining the internal environment of the body), nutrition of the capillary endothelium (the inner layer of the walls of blood vessels) and regenerative processes of damaged tissues due to the release of growth factors that stimulate cell division.
A 2021 scientific paper provides evidence showing that in addition to the above functions, platelets also play an important role in the human immune system.
Indications
Prescription of an OAC with a study of platelet concentration is indicated for all patients who visit the clinic, undergo a routine medical examination, or receive a referral for inpatient treatment. Also, platelet determination is prescribed to all patients requiring surgery (emergency or planned). The main indications for platelet testing include:
- suspicion of disturbances in the hemostatic system (bleeding, formation of subcutaneous hematomas);
- suspicion of a malignant process;
- immunity disorders;
- bronchopulmonary pathology;
- diseases of the digestive tract and urinary system (stomach ulcer, glomerulonephritis);
- cardiovascular pathology;
- endocrine disorders (obesity, diabetes).
Symptoms that should alert you
- red, purple bruises on the skin
- frequent nosebleeds, bleeding gums
- prolonged bleeding of even small wounds or cuts
- heavy menstrual bleeding in women
Treatment and severity
Treatment of thrombocytopenia most often comes down to identifying the primary disease and its treatment, as well as eliminating various unpleasant symptoms. In the process, it is also important to take into account that the severity of thrombocytopenia varies:
Mild degree. It assumes that the platelet concentration is from 50 to 150 thousand units per microliter. The condition of the capillaries is usually normal, bleeding does not develop. Usually, treatment is not necessary at this stage - doctors recommend waiting and monitoring the development of the patient’s condition.
Average degree. In this case, the concentration is 20-50 thousand platelet units per microliter. Under this condition, bleeding gums and nosebleeds are observed. If injuries and bruises occur, serious hemorrhages form in the skin. At this stage, drug therapy may be prescribed.
Severe degree. The platelet concentration is below 20 thousand, hemorrhages are spontaneous and severe. At the same time, the patient himself may feel quite comfortable, does not complain of feeling unwell, but tests show that he needs help.
Since the treatment of thrombocytopenia requires the most thorough and detailed diagnosis, it is important to choose a modern clinic that will help you. JSC "Medicine" in Moscow is just the place where you can get qualified help from the best specialists. The clinic has everything necessary for both examination and treatment of each patient.
Preparing for the study
Before taking the OAC, you should stop drinking alcoholic beverages, fatty, spicy, excessively salty and fried foods the day before the procedure. Blood is donated on an empty stomach, the patient is advised to maintain physical and emotional peace (refrain from sudden movements, climbing stairs, avoid stressful situations) for half an hour before the test. Also, platelet testing is not recommended immediately after recovery from a long-term illness, which may distort the results due to weakened immunity.
Detailed instructions for preparing for a general blood test are here.
What does a blood test show?
Some blood test results provide clear information about the risk of occurrence and presence of a particular disease, and also allow you to track the dynamics of the disease, both as it progresses and during the recovery process. Some important blood parameters, such as vitamin D and homocysteine, are unfortunately not included in most panels, despite the fact that they are quite informative.
It is important to remember that most blood biomarkers do not signal any one disease. Most often, a blood test means an increased risk of disease. During the diagnostic process, it is always necessary to take into account changes in several biomarkers (series, panel of analytes) in order to correctly interpret the latter. Testing all biomarkers is quite expensive (about 70,000 rubles on average), however, there are about 40 biomarkers that are the most informative, and the price here is relatively low (about 8,000 rubles).
Another important condition for the correct interpretation of blood biomarkers is the need for repeated studies. The indicators of one analysis are difficult to interpret, because we do not know its basic level, the nature of the influence of various factors, from dietary habits to the effects of drugs. It makes sense to take certain blood tests regularly, some should be done once a year, others - 3-4 times.
Biomarkers of complete blood count
Red blood cell count
Red blood cells are produced in the bone marrow and destroyed in the spleen and liver. The number of red blood cells may be increased due to dehydration and high testosterone levels. May be reduced due to nutritional deficiencies (iron, vitamin B6, vitamin B12, folate), renal dysfunction, chronic inflammation, anemia, blood loss.
Hemoglobin.
Hemoglobin carries oxygen to tissues and can be elevated due to dehydration, elevated testosterone levels, poor oxygen delivery, thiamine deficiency, and insulin resistance. May decrease due to anemia, liver disease, hypothyroidism, exercise, arginine deficiency, protein deficiency, lack of nutrients due to inflammation (vitamin E, magnesium, zinc, copper, selenium, vitamin B6, vitamin A).
Hematocrit
Hematocrit reflects the percentage of blood volume that is made up of red blood cells. May also be elevated due to dehydration, elevated testosterone levels, poor oxygen delivery, thiamine deficiency, insulin resistance. May decrease due to anemia, liver disease, hypothyroidism, exercise, arginine deficiency, protein deficiency, lack of nutrients due to inflammation (vitamin E, magnesium, zinc, copper, selenium, vitamin B6, vitamin A).
Average corpuscular volume
Mean corpuscular volume is an estimate of the average size of red blood cells. May be elevated (“macrocytic”) due to nutrient deficiencies (vitamin B12, folate, vitamin C), alcohol consumption, thiamine deficiency. May be reduced (“microcytic”) due to iron deficiency, lack of nutrients (vitamin B6, copper, zinc, vitamin A, vitamin C).
Average corpuscular hemoglobin
Average corpuscular hemoglobin is a measure of the average weight of hemoglobin per red blood cell. May be elevated (“macrocytic”) due to nutritional deficiencies (vitamin B12, folate, vitamin C), alcohol consumption, thiamine deficiency, and (falsely elevated) due to hyperlipidemia. May be reduced (“microcytic”) due to iron deficiency, lack of nutrients (vitamin B6, copper, zinc, vitamin A, vitamin C).
Average corpuscular hemoglobin concentration
Mean corpuscular hemoglobin concentration measures the average concentration of hemoglobin in red blood cells. May be elevated (“macrocytic”) due to nutritional deficiencies (vitamin B12, folate, vitamin C), alcohol consumption, thiamine deficiency, and (falsely elevated) due to hyperlipidemia. May be reduced (“microcytic”) due to iron deficiency, lack of nutrients (vitamin B6, copper, zinc, vitamin A, vitamin C).
Platelets
Platelets are involved in the clotting process and are important for vascular integrity. May increase due to iron deficiency anemia, collagen diseases, hemolytic anemia, blood loss, stress, infection, inflammation. May decrease due to alcoholism, liver dysfunction, viral/bacterial infections, pernicious anemia, bleeding.
Average platelet volume
Mean platelet volume measures the average size of platelets and reflects their function. May be elevated due to increased platelet production, which is often caused by the loss or destruction of existing platelets. Elevated mean platelet volume levels may be associated with vascular disease, some cancers, type 2 diabetes, and Hashimoto's thyroiditis. The mean platelet volume may be reduced due to conditions associated with insufficient platelet production, such as aplastic anemia or cytotoxic drug therapy.
Red blood cell distribution width
Red blood cell distribution width measures changes in red blood cell size. Usually increases due to anemia associated with nutritional deficiencies (iron, vitamin A, copper, zinc, vitamin B6).
Absolute neutrophils
Neurotrophils are the most common type of leukocytes that neutralize pathogenic microorganisms. May be elevated due to bacterial infection or inflammation. May be decreased due to nutrient deficiencies (copper, B12, folate), increased other white blood cells.
Absolute lymphocytes
Absolute white blood cells are a type of white blood cell including B cells, T cells, and natural killer cells. May be elevated due to viral infections, Crohn's disease and other autoimmune diseases, hypoadrenalism. May be reduced due to zinc deficiency, increase in other white blood cells.
Absolute monocytes
Absolute monocytes are white blood cells that leave the circulation to become macrophages. May be elevated due to inflammation, collagen diseases (i.e. rheumatoid arthritis), ulcerative colitis, recovery from infection or injury.
Absolute eosinophils
Absolute eosinophils are immune cells that become active in the late stages of inflammation. May be elevated due to allergies, asthma, parasitic infections, hypoadrenalism, skin diseases such as eczema, ulcerative colitis, Crohn's disease, aspirin sensitivity. May be reduced due to increased cortisol levels.
Absolute basophils
Absolute basophils are white blood cells associated with inflammation and hypersensitivity. May be elevated due to inflammation, allergies, hemolytic anemia, hypothyroidism.
Comprehensive Metabolic Panels
Glucose
Glucose is the concentration of sugar in the blood; may be elevated due to type 1 and type 2 diabetes, insulin resistance, increased levels of stress hormones or inability to inhibit liver glucose production, or (if not fasting) eating high carbohydrate foods.
Urea and nitrogen
Urea and nitrogen are markers of kidney function. May be elevated due to dehydration, poor kidney function, high protein intake, fatty liver, catabolic stress. May be reduced due to insufficient protein intake or protein malabsorption, liver disease, excessive eating and B6 deficiency.
Creatinine
Creatinine is a byproduct of the breakdown of creatine. May be increased due to kidney dysfunction, dehydration, excessive muscle breakdown or increased muscle mass, hyperthyroidism, high meat intake, ketones. May be reduced due to low muscle mass, poor protein intake.
Sodium
Sodium is a positively charged electrolyte, essential for muscle contraction, nutrient absorption, nervous system function, and pH balance. May be elevated due to dehydration, hyperaldosterone (sodium reabsorption), excess sodium intake. May be decreased due to elevated serum glucose, low cortisol levels, glycosuria, ketonuria, hypothyroidism, and fluid loss due to sweat.
Potassium
Potassium is a positively charged electrolyte essential for muscle contraction, pH balance, nerve signal conduction, and action potentials. May be elevated due to renal failure, hypoaldosterone, acidosis, hemolysis, low insulin levels, hyperglycemia, exercise. May be reduced due to poor potassium intake, alkalosis, hyperaldosterone, excessive fluid loss, elevated insulin levels, low magnesium levels, elevated estrogen levels, elevated catecholamines.
Uric acid
Uric acid is the end product of the metabolism and excretion of purine DNA in the kidneys; may indicate oxidative stress, and elevated levels are associated with cardiovascular disease and diabetes. May be elevated due to gout, kidney dysfunction, excessive alcohol consumption, fasting, excessive calorie restriction, liver dysfunction, hemolytic anemia, excess fructose intake, fungal infection, ketogenic diet, supplemental niacin, high protein diet, prolonged fasting, supplemental vitamin B3, excess acidity. May be reduced due to nutritional deficiencies (molybdenum, zinc, iron), oxidative stress, low purine intake (vegetarian or vegan), excess alkalinity.
Chloride
Chloride is a negatively charged electrolyte; important for maintaining cellular balance through cell membranes and for stomach acid production. May be elevated due to renal dysfunction, diarrhea, dehydration, hyperparathyroidism, hyperventilation. May be reduced due to vomiting, respiratory acidosis (hypoventilation), metabolic alkalosis, hypoaldosterone.
Calcium
Calcium plays important roles in the body including dental and bone health, blood clotting, neurotransmitter function, muscle contraction, and enzyme activity. May be increased due to alkalosis, renal dysfunction, hyperparathyroidism, cancer, excess vitamin D intake, adrenal insufficiency, excess vitamin A intake. May be decreased due to poor intake or absorption, hypoparathyroidism, vitamin D deficiency, magnesium deficiency.
Phosphorus
Phosphorus is a mineral involved in the synthesis of DNA and RNA, part of ATP, and helps activate enzymes. May be elevated due to vitamin D toxicity, hypoparathyroidism, renal dysfunction. May be reduced by poor absorption, vitamin D deficiency, elevated insulin levels, high carbohydrate diet, diarrhea, poor protein absorption.
CO2
Carbon dioxide (CO2) measures blood bicarbonate and is a surrogate marker for CO2 gas. May be increased due to vomiting, metabolic alkalosis, respiratory acidosis (hypoventilation). May be reduced due to metabolic acidosis, respiratory alkalosis (hyperventilation).
Total cholesterol
Total cholesterol is a fat-like substance that travels in the blood with carrier lipoproteins (HDL, LDL and VLDL); precursor of steroid hormones and bile salts. May be elevated due to poor thyroid function, insulin resistance, dysregulation of blood glucose, magnesium deficiency, dehydration, kidney disease, familial hypercholesterolemia. May be reduced due to liver dysfunction, oxidative stress, inflammation, malabsorption, anemia.
Triglycerides
Triglycerides: This test measures the level of fat in the body; usually done on an empty stomach. The indicator is related to cardiovascular diseases. May be elevated due to impaired blood glucose regulation, diabetes, hypercaloric diets, poor thyroid function, kidney disease, and alcohol consumption. May be reduced by fat malabsorption, low carbohydrate diets, calorie restriction, and potentially autoimmune disorders.
LDL-X
LDL-C is the amount of cholesterol bound to low-density lipoprotein (LDL) particles in the blood. May be elevated due to insulin resistance, impaired blood glucose regulation, poor thyroid function, kidney disease, familial hypercholesterolemia. May be reduced due to liver dysfunction, oxidative stress, malabsorption, anemia.
HDL-C
HDL is the amount of cholesterol bound to high-density lipoprotein particles in the blood. May be increased due to inflammation, oxidative stress, and excessive exercise. Low HDL levels are associated with metabolic syndrome and can be reduced due to insulin resistance, sedentary lifestyle, and poor diet.
Albumen
Albumin, the most abundant plasma protein synthesized in the liver, binds to other compounds in the blood and contributes to the plasma osmotic gradient. May be elevated due to dehydration. May be reduced due to infection, inflammation, liver disease, kidney disease.
Globulin
Globulin is a plasma protein with various subtypes. May be elevated due to cancer, autoimmune disease, increased estrogen. May be reduced due to hemolytic anemia, nephrosis, or impaired immune system.
Total bilirubin
Total bilirubin is a byproduct of the breakdown of red blood cells and an important component of bile; acts as an antioxidant. May be elevated due to excessive hemolysis, liver dysfunction, bile duct obstruction, Gilbert's syndrome. May be reduced due to oxidative stress, zinc deficiency.
Iron
Iron bound to transferrin is typically measured and represents ~⅓ of the total iron binding capacity to transferrin. By itself, it is a relatively poor marker of iron status. May be increased due to hemochromatosis and other genetic diseases, hemolytic anemia, liver damage, vitamin B6 deficiency. May be reduced due to poor iron intake, poor absorption, chronic blood loss, chronic disease or infection, or taking progesterone birth control pills.
Alanine aminotransferase
Alanine aminotransferase (ALT) is an enzyme found in highest concentrations in the liver and in smaller amounts in the heart, muscle, and kidneys. May be elevated due to hepatocellular diseases, gall bladder problems, pancreatitis.
Aspartate aminotransferase
Aspartate aminotransferase (AST) is an intracellular enzyme that usually increases due to the destruction of active tissue and cells. May be elevated due to hepatitis, liver cirrhosis or alcoholism, hypothyroidism. May be reduced due to vitamin B6 deficiency, increased serum nitrogen.
GGT
GGT is an enzyme found primarily in the liver, kidneys, and pancreas. May be elevated due to gallbladder dysfunction, alcoholism, pancreatitis, oxidative stress. May be reduced due to hypothyroidism, magnesium deficiency.
Lactate dehydrogenase
Lactate dehydrogenase may be elevated due to liver disease, hypothyroidism, skeletal muscle damage, anemia (hemolytic), and fractures. May be reduced due to reactive hypoglycemia, insulin resistance, ketosis.
Alkaline phosphatase
Alkaline phosphatase is an enzyme found in the liver, bone, kidney, small intestine and placenta. May be increased due to liver obstruction, liver cirrhosis, gastrointestinal tract, hyperphosphatemia, hyperparathyroidism. May be reduced due to lack of nutrients (zinc, magnesium and/or vitamin C).
Additional biomarkers
- C-reactive protein
- Cortisol
- Sulfate-DHEA
- Estimated glomerular filtration rate (eGFR)
- Estradiol
- Ferritin is an iron-binding protein in the body. May be elevated due to hemochromatosis and other genetic conditions, inflammation, liver damage, hemolytic or sideroblastic anemia. May be reduced due to poor intake, poor absorption, chronic blood loss, chronic disease or infection, progesterone birth control pills.
- folate
- Glycated hemoglobin
- homocysteine
- progesterone
- Testosterone
- Thyroid-stimulating hormone
- Vitamin D, 25-hydroxy
- Antinuclear antibody (ANA) - a common test for autoimmune disease
Platelet norms
Important! Standards may vary depending on the reagents and equipment used in each particular laboratory. That is why, when interpreting the results, it is necessary to use the standards adopted in the laboratory where the analysis was carried out. You also need to pay attention to the units of measurement.
The list shows the reference values of platelet cells adopted in the Invitro laboratory:
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| Children | boys | girls |
| less than 2 weeks | 218 — 419 | 144 — 449 |
| 2 weeks — 1 month | 248 — 586 | 279 — 571 |
| 1 - 2 months | 229 — 562 | 331 — 597 |
| 2 — 6 | 244 — 529 | 247 — 580 |
| 6 months - 2 years | 206 — 445 | 214 — 459 |
| 2 years - 6 years | 202 — 403 | 189 — 394 |
| Adults | men and women | |
| over 6 years old | 150 — 400 | |
In the Helix laboratory there is a slightly different gradation of values:
| Age | Reference values 109/l |
| Less than 10 days | 99 — 421 |
| 10 days – 1 month | 150 — 400 |
| 1-6 months | 180 — 400 |
| 6 months – 1 year | 160 — 390 |
| 1-5 years | 150 — 400 |
| 5-10 years | 180 — 450 |
| 10-15 years | 150 — 450 |
| More than 15 years | 150 — 400 |
It should be noted that the platelet count decreases slightly in women during the menstrual period, but returns to normal after bleeding stops. A slight decrease (up to 150) in platelet concentration during the gestational period is also possible, which is explained by blood dilution due to an increase in BCC (circulating blood volume) and due to insufficient nutrition of the expectant mother.
Important! The interpretation of the results is always carried out comprehensively. It is impossible to make an accurate diagnosis based on only one analysis.
Deviation from the norm is not always a disease
If the level of red blood cells during the first analysis is slightly outside the normal range, do not panic.
Your doctor will help you interpret the results correctly, taking into account your individual characteristics and medical history. A single slightly elevated or slightly decreased result may have no medical significance. There are several factors that can cause a test result to fall outside the established reference range without pathological reasons:
- Under the influence of external factors (stress, previous infections, physical activity), the results of the analysis of the same person may differ slightly. In this case, a person can be healthy. If the analysis shows a slight deviation, retake the test on another day.
- Individual characteristics. For some people, the boundaries of the norm may differ slightly from generally accepted ones. Reference values are valid for the vast majority of people, but we are all different, and in some rare cases, a healthy person may have their own norms, slightly different from the usual values.
Only a doctor can accurately determine this after conducting additional research.
Drugs that affect platelet levels
Long-term use of these drugs may change platelet levels:
- aspirin
- pain relievers such as ibuprofen and naproxen
- antihistamines
- asthma medicine
- sildenafil (Viagra)
- drugs used to prevent blood clots, such as clopidogrel
- antibiotics
- antidepressants and antipsychotic drugs
- Cholesterol-lowering drugs (statins)
- calcium channel blockers (verapamil).
Increase P-LCR
An increased number of large platelets means that there is a pathology in the body. Only in isolated cases is a high P-LCR value an individual characteristic of a person and does not require treatment.
Etiology
The reasons for an increase in P-LCR can be completely different diseases - inflammatory, oncological, hematological, infectious.
But most often, the formation of a large number of large platelets occurs in autoimmune disorders.
Systemic diseases that can cause thrombocytosis include: collagenosis (scleroderma, systemic lupus erythematosus, rheumatic diseases, periarteritis nodosa), sarcoidosis, polyarthritis, ankylosing spondylitis, enteropathy. These processes are accompanied by the release of interleukin and other inflammatory mediators into the blood, which stimulate the biosynthesis of thrombopoietin and the formation of a large number of platelets.
Along with this, the P-LCR index increases if the patient has:
- infectious pathology - bacterial, viral, fungal, parasitic,
- post-traumatic and postoperative syndrome,
- oncological and hematological diseases - lymphoma, neuroblastoma and hepatoblastoma, anemia,
- spleen diseases,
- cirrhosis or polycystic liver disease,
- damage or inflammation of the spinal cord,
- alcoholism,
- intoxication with chemicals that disrupt bone marrow function,
- atherosclerosis,
- diabetes mellitus
Some scientists believe that the increase in P-LCR is due to a congenital stem cell defect. In patients, the process of platelet formation is disrupted. The large cellular elements produced are defective and inactive. They are unable to adequately interact with other structures and function fully.
A high P-LCR index leads to the fact that the patient has a tendency to thrombosis. Due to the adhesive properties of platelets, they stick together and form a blood clot, which disrupts blood circulation and prevents the free movement of blood. As the thrombus grows, it narrows the lumen of the vessel, disrupts the blood supply to the organ, and causes hypoxia and ischemia of the tissue. When the coronary arteries are damaged, this leads to myocardial infarction. With thrombosis of cerebral vessels, an ischemic stroke develops. The result of the process is often varicose veins or atherosclerotic changes in the arteries. These pathologies are deadly and often result in the death of patients.
Symptoms
When the P-LCR increases, the patient develops corresponding clinical signs. They may go unnoticed behind the obvious symptoms of the causative disease. Such patients are not treated for thrombocytosis, which further aggravates the situation.
An increase in P-LCR is manifested by the following symptoms:
- hypersensitivity and pain in the fingertips,
- causeless appearance of hematomas,
- irritation and itching of the skin,
- cyanosis,
- asthenia of the body,
- rapid heartbeat,
- shortness of breath at rest,
- visual dysfunction.
These signs are optional. They can appear individually or in various combinations. But despite this, the patient needs to visit a health care facility and undergo certain tests, based on the results of which doctors will determine the cause of the P-LCR deviation and prescribe appropriate treatment.
Treatment and diagnostic procedures
To determine the cause of the disorder and make a correct diagnosis, in serious cases, a bone marrow biopsy is examined and blood is taken again. Additionally, general clinical and molecular tests and ultrasound of internal organs are performed.
To normalize the P-LCR value, the causative disease
. If the pathology is not treated, the patient risks dying from thrombosis, or more precisely from its consequences - acute coronary or cerebral failure. These phenomena are very dangerous. They are often fatal. That is why this deviation needs to be corrected. Hematologists carry out diagnostic and treatment measures. Restoration of normal P-LCR levels in a blood test is a sign of adequate and effective therapy.
- Patients are prescribed a diet rich in vegetables and fruits, vegetable oils, freshly squeezed juices and other products that make the blood less viscous. For the same purpose, experts recommend optimizing your drinking regime - drinking up to 2-3 liters of water per day.
- To prevent thrombosis and its consequences, the use of antiplatelet agents and anticoagulants is indicated - Aspirin, Cardiomagnyl, Trental, Cavinton, as well as drugs that improve microcirculation - Dipyridamole, Piracetam, Vinpocetine.
- If the cause of a high level of large platelets is an infectious disease, then after intensive antibiotic therapy, the P-LCR index value returns to normal almost immediately.
- In severe cases, the use of corticosteroids - Prednisolone, Dexamethasone and cytostatics - Anagrelide, Hydroxyurea, Radioactive phosphorus 32P is indicated.
- To stimulate the immune system, Interferon and its derivatives are prescribed.
- There are folk remedies that allow you to correct (but not eliminate) existing violations. These include: mulberry poison, sweet clover infusion, ginger tea, celery juice. These plants have a beneficial effect on the condition and activity of platelets.
Platelets are reduced (thrombocytopenia)
When the concentration of platelets in the CBC decreases, they speak of the development of thrombocytopenia, which is accompanied by a blood clotting disorder and a tendency to bleed (gums bleed, nosebleeds or intestinal bleeding often occur, menstruation becomes long and heavy). Thrombocytopenia develops in a number of serious diseases due to the loss of elasticity of the vascular wall, their fragility and fragility and the risk of internal bleeding.
Reasons that provoke a decrease in platelet levels include:
- hemolytic-uremic syndrome or Gasser's disease (a combination of hemolytic anemia, thrombocytopenia and acute kidney failure);
- thrombocytopenic purpura or Werlhof's disease (one of the widows of hemorrhagic diathesis);
- allergic thrombocytopenia (taking a number of medications: procainamide, heparin, co-trimoxazole);
- DIC syndrome (second stage);
- severe liver damage (hepatitis, cirrhosis);
- alcoholism;
- malaria;
- enlarged spleen;
- bone marrow diseases, some leukemias;
- megaloblastic anemia;
- pathology of the thyroid gland (hypothyroidism, thyrotoxicosis).
It is important to note that a decrease in platelet concentration (75 – 150) is observed in pregnant women, which is not regarded as a pathology.
How does a blood clot form? Why is a test for induced platelet aggregation prescribed?
Normally, platelets in the blood are in an inactive state; the cells have a discoid, slightly elongated shape, which is why in old textbooks they are called “blood plates.” When bleeding begins, platelets are activated: they acquire a spherical shape and form special outgrowths - pseudopodia. With their help, they can connect with each other (aggregate) and stick to the site of damage to the vascular wall (adhere). These two processes provide the basis for thrombus formation.
To assess the quality of platelet aggregation and find out whether it is reduced or, conversely, does not occur too intensely, an analysis for induced platelet aggregation is prescribed. To do this, they take blood from a vein, add special substances (activation inducers) to it and evaluate the process.
When preparing for the study, it is important to comply with certain conditions - for 3 days, follow a special diet prepared by a doctor, 24 hours before, avoid taking stimulants (coffee, alcohol, nicotine, garlic) and immunostimulant drugs, 8 hours before, stop taking medications and fatty foods.
Low platelet activity occurs in diseases of the hematopoietic system, constant use of antiplatelet drugs, in this case the duration of bleeding increases. Increased aggregation, on the contrary, increases the risk of thrombosis: venous thrombosis, heart attack, stroke. You may ask, why order an induced activation test if the risk of bleeding/thrombosis can be assessed by the total platelet count? Alas. Even with normal numbers, most of the cells may turn out to be “defective”, so we are talking about severe platelet deficiency with their normal concentration in the blood.
Platelets are increased (thrombocytosis)
An increase in platelet count (thrombocytosis) is observed when:
- excessive physical stress
- chronic inflammatory processes (rheumatoid arthritis, tuberculosis, sarcoidosis);
- myeloproliferative diseases (primary erythrosis, chronic myeloid leukemia, myelofibrosis, myelosclerosis);
- some hemolytic anemias;
- hemolysis or severe blood loss;
- carcinoma, lymphoma;
- after removal of the spleen.
Sources:
- Eugenio D. Hottz. Platelets in Immune Response to Virus and Immunopathology of Viral Infections. — Front Med (Lausanne). Apr 2018.
- Data from the independent laboratory Invitro.
- Data from Helix laboratory.
- Steven Kim, MD. Acquired Platelet Function Disorder. — Healthline, Jan 2021
- Douglas B. Cines. Thrombocytopenia in pregnancy. - Blood. 2017 Nov 23; 130(21): 2271–2277
- Danilova L.A., Doctor of Medical Sciences, Prof. Analyzes of human blood, urine and other biological fluids at different age periods, SpetsLit, 2014.
Diagnostics
Thrombocytosis is detected in a clinical blood test. Although very high platelet counts are more common in hematologic diseases, platelet levels alone cannot determine the cause of thrombocytosis. Therefore, if it is detected, you should visit a therapist. The doctor carefully asks about the patient’s complaints, how long ago the symptoms occurred, and conducts a general examination of the patient. Then, based on the data obtained, an additional examination is prescribed, including:
- Blood tests
. In a general blood test, the content of other formed elements (erythrocytes, leukocytes) is determined, and the leukocyte formula is calculated. The concentration of inflammatory markers (ESR, CRP) is measured. The indicators of serum iron, TBC, ferritin are assessed. The presence of autoantibodies (RF, ACCP, antibodies to the cytoplasm of neutrophils) is checked. In case of endocarditis and sepsis, an analysis for procalcitonin and presepsin is performed. - Pathogen identification
. To identify the pathogen, microscopy, bacterial culture of urine and sputum are performed. If tuberculosis is suspected, an intradermal test with tuberculin is prescribed. Using an enzyme immunoassay, antibodies to viruses, parasites, and fungi are detected, and using the polymerase chain reaction method, their DNA and RNA are detected. To diagnose meningitis, a cerebrospinal fluid analysis is informative. - Genetic research
. In patients with myeloproliferative pathologies, mutations of Janus kinase (JAK2V617F), thrombopoietin receptors (MPL), and erythropoietin are determined using fluorescent hybridization (FISH) and PCR. Sometimes chromosomal abnormalities are detected - trisomies, deletions. In chronic myeloid leukemia, cytogenetic analysis reveals the Philadelphia chromosome (Ph). - X-ray
. On an X-ray of the lungs, in case of pneumonia, foci of darkening and infiltrates are noted, in case of tuberculosis - enlargement of the mediastinal lymph nodes, expansion of the roots of the lungs, rounded shadows (cavities) of the upper lobes of the lungs. In patients with arthritis, x-rays of the joints show a narrowing of the joint space, areas of erosion, and marginal osteoporosis. - Ultrasound
. Ultrasound of the abdominal organs in case of pyelonephritis determines compaction and expansion of the pyelocaliceal system, and in case of blood diseases - splenomegaly. In bacterial endocarditis, cardiac echocardiography reveals vegetations of the valves and sometimes effusion into the pericardial cavity. - Endoscopy
. In patients with inflammatory bowel pathologies, fibrocolonoscopy is performed, which reveals hyperemia of the mucous membrane, lack of vascular pattern, erosion, and ulcerative defects. Crohn's disease is characterized by the "cobblestone pavement" symptom - alternating deep ulcers with unchanged mucous membrane. - Histological studies
. In bone marrow aspirate for malignant hematological pathologies, hyperplasia of the megakaryocyte lineage of hematopoiesis is noted (in polycythemia vera - all three lineages), a large number of blast cells (in myeloid leukemia), proliferation of reticulin and collagen fibers (fibrosis). In case of vasculitis, a biopsy of a vessel reveals pronounced perivascular infiltration with lymphocytes and plasma cells.
Platelet count according to Fonio
Drug therapy
With the correct selection of medications, it is possible to stably and quickly reduce the platelet count and prevent complications.
The earlier treatment for thrombocytosis is started, the faster it can be dealt with.
For this purpose the following medications are prescribed:
- Anti-inflammatory, based on acetylsalicylic acid.
- Antitumor - "Hydroxyurea" .
- To eliminate thrombosis, with the effect of slowing blood clotting.
- Immunostimulator "Interferon" .
- Blood-thinning drugs - “Curantil”, “Trental” .
Trental Curantyl Interferon Hydroxyurea
The dosage depends on the stage of the disease, as well as on the age of the patient. The doctor will check your platelet count regularly. If there is no decrease in their levels, medications will need to be replaced.
Symptoms and manifestations of thrombocytosis
At the very beginning of the disease, there may be no signs. The secondary form of the disease has more pronounced manifestations, since they begin against the background of the appearance of chronic inflammation. The presence of thrombocytosis in the blood can be assumed by the following symptoms:
- Fast fatiguability.
- Deterioration in general health.
- Edema.
- Bleeding.
- Problem with the functioning of blood vessels.
- The appearance of hematomas not associated with bruises.
- Hypertension, migraine.
- Painful shortness of breath.
- Feeling of heaviness in the right hypochondrium.
Many patients find out that they are sick after a clinical blood test. The primary form can develop into a chronic stage in a short time. When thrombocytosis of the second type appears, patients often complain of unpleasant conditions associated with their main illness. If you quickly diagnose and determine the cause of deterioration in health, treatment will be prescribed in a timely manner. In this case, blood clotting is unlikely.
Traditional recipes for thrombocytosis
Treatment of the disease is sometimes carried out using traditional methods. Natural ginger, garlic tincture, berry infusions and Gingko Biloba are used. Cocoa, which should be drunk in the morning, before breakfast, without sugar and milk, also helps. Experts may recommend hirudotherapy.