PCI (percutaneous coronary intervention) is used in cardiology to resume blood flow through the arteries of the heart. It can prevent myocardial infarction or reduce its spread. Prescribed on an emergency or planned basis. Absolute contraindications are bleeding and the inability to insert a catheter through the vascular network.
The operation takes the form of balloon expansion of the site of narrowing and removal of the plaque, installation of a metal frame (stenting), or laser revascularization is used. The PCI method is low-traumatic, since only a puncture of the femoral artery is needed, it reduces the frequency of angina attacks and increases exercise tolerance.
The downside is the risk of re-occlusion, so it is important to take medications for life to reduce blood viscosity, adhere to a diet, moderate physical activity, and give up smoking and alcohol abuse.
PCI in cardiology - what is it?
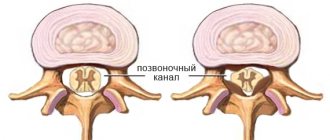
Explanation PCI is a percutaneous coronary intervention, it is used in cardiology to restore the patency of the heart artery. Recommended for atherosclerosis of the heart vessels - angina pectoris, myocardial infarction. It is called percutaneous because a catheter inserted through the skin penetrates the vessel. For this purpose, the femoral artery is usually used, and the progress of the instrumentation is monitored using radiography.
There are 3 methods of PCI: balloon angioplasty, stenting and laser revascularization. In the first case, the lumen is expanded with the help of an inflating balloon, it crushes the plaque, in the second, a stent (metal frame) is additionally placed in this area, and in the third, laser beams destroy cholesterol accumulations.
We recommend reading the article about TEE of the heart. From it you will learn about the advantages and disadvantages of the method, indications for cardiac TEE, as well as how transesophageal electrophysiological examination is performed. And here is more information about myocardial rupture.
Indications for PCI
Indications for PCI surgery include:
- myocardial infarction;
- angina pectoris with an unstable course or pre-infarction conditions (attacks become more frequent and stronger, there are rhythm disturbances, typical changes in ECG, blood enzymes, heart failure);
- stable angina with resistance to medications or contraindications for their constant use;
- unstable atherosclerotic plaque (dangerous for a heart attack), discovered during examination;
- narrowing of the lumen of the vessel after coronary artery bypass surgery or previously performed stenting.
Contraindications for carrying out
It is impossible to perform PCI only in cases of extensive bleeding (anticoagulants cannot be taken afterwards) and widespread damage to the vascular network, when it is difficult to insert the catheter into the site of narrowing. The doctor evaluates all other contraindications to angioplasty only on an individual basis, comparing the risk of the operation and its absence:
- the lumen of the artery is up to 3 mm, and the narrowing area is more than 20 mm;
- multiple changes in the coronary vessels;
- low blood clotting activity, anemia;
- damage to the vessels in the extremities (especially the femoral) through which the catheter will be inserted;
- inability to perform coronary angiography due to intolerance to contrast agents;
- arterial hypertension that cannot be controlled with medications;
- high body temperature, infection, exacerbation of inflammation;
- decompensated diabetes mellitus;
- contraindications for the use of blood thinners after surgery (other than bleeding);
- insufficiency of kidney and liver function;
- circulatory disorders in the cerebral arteries;
- mental illnesses;
- neoplasms;
- heart valve damage;
- bacterial endocarditis;
- rheumatism, myocarditis.
Performing primary percutaneous coronary intervention (PCI) is the main modern method of treating patients with ST-segment elevation myocardial infarction (MI) [10]. The main problem after PCI in such patients is severe microvascular obstruction or the no-reflow phenomenon [5]. The results of a number of studies have demonstrated that early complications of MI (arrhythmias, pericardial effusion, cardiac tamponade, early congestive heart failure) are more common in patients with the no-reflow phenomenon; unfavorable left ventricular remodeling; repeated hospitalizations for heart failure and increased mortality [1, 2, 6, 7, 12]. Therefore, detection, prevention and treatment of the no-reflow phenomenon are of utmost importance for the results of primary PCI.
The occurrence of the no-reflow phenomenon is the cause of a changing combination of four pathogenetic components: 1) distal atherothrombotic embolism; 2) ischemic damage; 3) reperfusion injury; 4) sensitivity of myocardial microcirculation to damage [14].
A logical prerequisite for the prevention of distal embolism during PCI is the use of thrombus aspiration devices, since they can reduce the volume of thrombus in the arterial lumen, better visualize the true lesion, and perform direct stenting without prior balloon angioplasty. Currently, several models for thrombectomy are available, which can be divided into catheters for manual thrombus aspiration and devices for rheolytic destruction and aspiration of thrombi due to the Venturi effect [13, 16].
Strategies aimed at reducing the time from onset of chest pain to balloon angioplasty have been extensively studied and may reduce the incidence of no-reflow by reducing total ischemic time. In addition, known drugs that reduce myocardial oxygen demand and therefore the severity of ischemia may improve outcomes, at least in part, by improving myocardial perfusion [14].
The results of a number of studies that included patients at high risk for the no-reflow phenomenon and with risk factors for reperfusion injury have demonstrated conflicting results on the effectiveness of the use of platelet glycoprotein receptor blockers IIb/IIIa. It should be noted that, according to other studies, the use of IIb/IIIa glycoprotein receptor blockers is associated with an increase in the number of bleedings during PCI [10].
Although genetically determined sensitivity to microcirculatory injury is difficult to correct, acquired sensitivity may be treatable. Indeed, optimal and rapid treatment of hyperglycemia is probably the most important goal in the prevention of no-reflow. According to the DIGAMI study, lower blood glucose levels are associated with a reduction in infarct size. Moreover, statins also have the potential to reduce the size of reperfusion injury [11]. K. Iwakura et al. [9] demonstrated that chronic statin therapy in patients with or without hypercholesterolemia is associated with lower no-reflow rates and better functional recovery.
The purpose of the study was to determine the effectiveness and safety of using thrombus aspiration devices in combination with intravenous eptifibatide in the prevention of severe microvascular obstruction (no-reflow phenomenon) during primary PCI in patients with STEMI.
Material and methods
From October 2009 to February 2011, 92 patients with acute MI were treated at the Department of X-ray Surgical Methods of Diagnostics and Treatment of City Clinical Hospital No. 12. The criteria for inclusion in the study were the duration of STEMI no more than 12 hours, angiographic signs of a thrombus in the lumen of the epicardial coronary artery. Exclusion criteria: history of MI, cardiogenic shock, previous coronary artery bypass grafting, left or right bundle branch block, pacemaker rhythm.
All patients were divided into two groups: group 1 consisted of 45, group 2 - 47. Patients of groups 1 and 2 were comparable in terms of initial clinical characteristics (Table 1).
Before the intervention, all patients received 600 mg of clopidogrel and 300 mg of acetylsalicylic acid orally. After this, patients underwent coronary angiography, the results of which, in comparison with ECG data, determined the localization of the lesion in the infarct-related artery (Table 2).
All patients in the 1st and 2nd observation groups had angiographic signs of a thrombus in the lumen of the infarct-related artery.
During PCI, all patients of groups 1 and 2 were intravenously administered 70 units/kg of unfractionated heparin. The first stage of PCI was mechanical recanalization with a guidewire. Then, in the 1st group of patients, the thrombus was aspirated using an Export catheter (Medtronic, USA) and the IIb/IIIa glycoprotein platelet receptor blocker eptifibatide was administered intravenously in a bolus of 180 mcg/kg, followed by a constant infusion of 2.0 mcg/kg/min. during PCI and 12 hours after the operation. In group 2, balloon angioplasty was performed. PCI in both groups 1 and 2 was completed with stenting.
The adequacy of reperfusion after the intervention was assessed by the degree of blood flow according to the TIMI scale and myocardial contrast according to the results of coronary angiography and ST segment reduction according to the results of electrocardiography. Reperfusion was considered adequate when blood flow grade TIMI 3 in combination with myocardial contrast grade 2 or 3 and a reduction in ST segment elevation by more than 70% 1 hour after completion of the intervention. Inadequate reperfusion (no-reflow phenomenon) was determined when blood flow on the TIMI scale <3 or 3 with a degree of myocardial contrast from 0 to 1 and a decrease in ST segment elevation by 70% or less 1 hour after completion of the intervention.
At the hospital follow-up stage, the following indicators were assessed: recurrent MI, re-PCI, clinically significant bleeding and death. Clinically significant bleeding included intracranial bleeding; bleeding causing hemodynamic instability or requiring intervention; bleeding requiring blood transfusion, but not leading to hemodynamic disturbances.
In the long-term follow-up period (after 12 months), the following indicators were assessed: recurrent MI, return of clinical manifestations of angina, functional class (FC) of heart failure (HF) according to the New York Heart Association (NYHA) classification, and mortality.
Statistical analysis was performed using the Statistica 7.0 program (StatSoft Inc., USA). Comparisons of quantitative variables were made using the Mann-Whitney test, qualitative variables - using the two-tailed Fisher test and the Pearson χ2 test. Differences were considered statistically significant at p<0.05.
results
When performing PCI in group 1 using a device for thrombus aspiration, macroscopic thrombus fragments were obtained in 34 (75.6%) patients. Angiographic criteria for epicardial blood flow and tissue perfusion after stenting in groups 1 and 2 are presented in Table. 3.
According to angiographic criteria, adequate reperfusion was determined statistically significantly more often in group 1 of patients.
1 hour after completion of the intervention in the intensive care unit, an ECG was taken and the dynamics of the ST segment were assessed (Table 4).
Statistically significant differences were found in the reduction of the ST segment 1 hour after PCI in favor of the group where thromboextraction was performed with simultaneous administration of eptifibatide.
Cardiac complications and bleeding were assessed over 30 days (Table 5).
Statistically significantly more often deaths were recorded in the group where standard PCI was performed. When analyzing fatal outcomes in patients of group 2, it was found that in these observations after PCI the criteria for adequate reperfusion were not achieved.
After 12 months, long-term results were studied in 40 patients of group 1 and 38 patients of group 2 (Table 6).
There were no statistically significant differences between the 1st and 2nd groups of patients in terms of the incidence of recurrent MI, recurrence of angina pectoris and mortality.
In patients without repeated MI and recurrence of angina after 12 months of observation, the FC of HF was determined according to the NYHA classification (Table 7).
Statistically significantly more often in group 2 patients, HF class III was determined according to NYHA after 12 months of observation. When analyzing patients of group 2 with HF class III, it was found that after PCI they did not achieve the criteria for adequate reperfusion.
Discussion
Currently, a number of studies have been conducted in Europe and the USA in patients with STEMI, which used various systems for thrombus aspiration and microvascular protection.
The prospective randomized TAPAS trial included 1071 patients with STEMI. The results of the study demonstrated that in patients with STEMI, the strategy of coronary thrombus aspiration before primary PCI with stenting not only leads to improved myocardial perfusion immediately after surgery, but is also accompanied by better long-term clinical results compared with standard intervention [16]. Results from the DEAR-MI and REMEDIA trials also demonstrated better myocardial reperfusion immediately after intervention when using clot aspiration catheters [4, 15]. Indicative are the results of a meta-analysis of 11 studies, which included 2686 patients. Based on these findings, it was concluded that the use of thrombus aspiration devices significantly improves clinical outcomes in patients with STEMI undergoing mechanical reperfusion [3].
In our study, in the group of patients in whom thrombus aspiration devices were used in combination with intravenous eptifibatide, the results of restoration of epicardial blood flow and myocardial perfusion after PCI were statistically significantly better than in the control group.
In this group of patients, a decrease in the ST segment of more than 70% was also more often detected 1 hour after PCI. During the in-hospital follow-up period, statistically significant differences in mortality were obtained in favor of the group where thrombus aspiration devices were used in combination with intravenous eptifibatide. It should be noted that the use of eptifibatide in group 1 of patients did not increase the number of bleedings. During 12 months of follow-up, the patient groups did not differ in the incidence of recurrent myocardial infarction, repeat PCI, and mortality. However, statistically significantly less often in the group of patients where prevention of microvascular obstruction was used, NYHA HF class III was determined in the long-term follow-up period.
conclusions
1. When performing primary PCI using devices for thrombus aspiration in combination with intravenous administration of eptifibatide, severe microvascular obstruction (no-reflow phenomenon), assessed by angiographic and ECG criteria, is detected statistically significantly less frequently.
2. When performing primary PCI using devices for thrombus aspiration in combination with intravenous administration of eptifibatide, mortality during the hospital observation period and the number of patients with HF class III according to the NYHA classification in the long-term observation period are statistically significantly reduced.
3. The use of eptifibatide in combination with dual-component antiplatelet therapy and heparin therapy during primary PCI is not associated with an increase in the number of clinically significant bleedings.
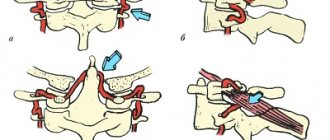
Techniques for performing PCI
PCI is performed in several ways, with many of the approaches being the same:
- preparation - coronary angiography, blood tests: general, biochemistry with kidney and liver tests, sugar, cholesterol, coagulation, for infections (viral hepatitis, HIV, syphilis), ECG, ultrasound of the heart and blood vessels of the extremities;
- local anesthesia in the area of the projection of the femoral artery, incision 2-3 mm;
- introduction of a conductor and contrast agent;
- identification of the narrowing area;
- approaching the catheter to the location of the plaque.
Subsequently, depending on the method of restoring blood flow, the balloon expands and crushes the cholesterol plaque, a stent is installed, or atheromatous deposits are destroyed by laser beams.
After coronary blood flow has been restored, the instruments are removed and a pressure bandage is applied to the thigh.
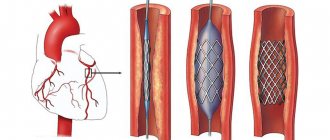
How is PCI with stenting performed?
If PCI is performed with stenting, then after inflation with a balloon, a metal structure – a stent – is installed into the lumen of the vessel. It first passes in a curled form, and then straightens out at the point of narrowing. Its installation prevents the walls of the arteries from collapsing, and the medicinal coating also prevents re-clogging.
PCI with a stent can be a method of treating myocardial infarction, then it is performed urgently in the first 6 hours, less often during 12. If the goal is to prevent a vascular accident, then the operation will be planned, after an in-depth examination, which helps to avoid many complications.
Coronary angiography of the heart vessels
Stenting takes about 2 hours. During PCI, there is pain or discomfort in the heart, a burning sensation in the chest. Upon completion of all manipulations, the patient is admitted to the postoperative ward for constant monitoring - monitoring of ECG, blood pressure, pulse, he is given blood and urine tests to exclude coronary circulatory disorders.
After a day for a planned operation and after 2-3 days for an emergency operation, you can be in a regular ward; if there are no complications, the patient is discharged for rehabilitation at the place of residence.
Stenting
Stenting is one of the most effective methods of relieving a patient from the risk of heart attack, stroke, and constant attacks of angina. It helps supply the myocardium with the necessary amount of oxygen through the installation of a vascular implant - a stent.
Restoration of blood flow patency occurs under x-ray control throughout the entire operation. Surgeons, constantly monitoring the patient's heart rate, inject a contrast agent through a catheter into the hip artery.
When mixed with blood, it fills the vessels, helping doctors visualize the area of work. Anesthesia is not required for stenting. Due to the simplicity and short duration of the operation, local anesthesia is sufficient, allowing doctors to maintain contact with the patient during the installation of coronary stents.
On the other hand, through the brachial artery, another catheter with a special “balloon” is inserted, expanding the previously implanted implant to the size of the vessel. Depending on the condition of the vascular system and the blockage of a particular artery, not one, but 2 or even 3 stents may be installed.
At the final stage, surgeons check the result of their work, assessing how freely blood now flows through the previously injured coronary vessel.
Advantages of primary percutaneous coronary intervention over conventional surgery
The advantages of percutaneous coronary intervention (compared to bypass surgery) include:
- there is no need for general anesthesia, ventilation, switching to artificial circulation, or opening the sternum;
- no long recovery required;
- the effectiveness in normalizing blood flow is comparable - pain in the heart stops or appears less frequently;
- lower risk of cerebral blood flow disorders and postoperative pneumonia.
But with PCI, it is more common for the stent to become blocked or the site of expansion to narrow again, which requires another operation. This complication occurs in every fifth patient after 6-9 months.
Expert opinion
Alena Ariko
Expert in Cardiology
The disadvantages of any method of surgical improvement of coronary circulation include a symptomatic effect. This means that in this way it is possible to remove an obstacle to the movement of blood and relieve pain in the heart, but it cannot cure atherosclerosis. Therefore, patients require long-term drug prevention of re-clogging of the arteries, drugs that reduce blood viscosity, and lifestyle changes.
Contraindications
PCI in cardiology is a non-hazardous surgical intervention, which nevertheless requires a careful examination of the patient’s general health condition. Among the main contraindications to percutaneous coronary intervention, cardiologists note:
- body resistance to antiplatelet therapy;
- renal failure (its acute or chronic form);
- dysfunction of the gastrointestinal tract, including prolonged bleeding;
- febrile conditions (especially if it is impossible to determine the reasons that provoked their occurrence);
- recent stroke;
- anemia (moderate and high);
- hypertension (uncontrollable and uncontrollable by medication);
- electrolyte disturbances (not only pronounced, but also in a latent form);
- inability to maintain contact with the person being operated on, for example, due to his being in an unconscious or inadequate state;
- the presence of a serious disease that may be negatively affected by PCI;
- the patient’s refusal to receive postoperative medical support (under such circumstances it is impossible to control potentially dangerous consequences for the patient’s body);
- intoxication;
- individual intolerance to a number of medications. Including anesthetic type;
- severe heart failure.
Depending on the number and type of contraindication, the doctor makes a decision on the advisability of PCI in a particular case. Refusal from coronary plastic surgery may be temporary, since some of the above circumstances can be corrected and partially or completely eliminated.
Devices used
The operation of stenting heart vessels is performed using the following equipment:
- X-ray machine;
- monitors to display the movement of instruments through vessels;
- a conductor with a catheter and an expanding balloon or laser beam emitter;
- stents – metal frames, conventional or drug-eluting, inert materials.
Watch the video about stenting heart vessels:
Types of stents
PCI in cardiology is a process that involves the use of advanced inventions. One of these is a stent. It is a thin metal tube formed from small cells. After being introduced into the body, the stent is inflated to the size of the vessel with a special balloon inserted through the artery.
The differences between its types are due to many factors: the material used in manufacture, the coating applied to the surface, the type of opening after installation in the vessel, and so on.
The main classification involves dividing implants into:
- Wire (1 type of wire is used in production).
- Tubular (their design is based on a cylinder-shaped tube).
- Ring (the design implies the presence of several rings fastened together).
- Mesh (outwardly they look like a mesh).
- Self-expanding (after installation in a vessel, they increase in it to the required size without the use of additional equipment).
- Expandable using a “balloon” (they acquire the required size after “inflating” with a device inserted through an artery).
The type of stent chosen by the surgeon for a particular person depends on the location of the implant, as well as the presence of contraindications for the person being operated on (for example, allergic reactions to a metal alloy).
Types of stents
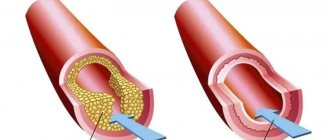
There are several types of stents:
- ordinary metal ones without coating - cheaper than others, made of steel or cobalt, nickel alloys, tantalum, widely used, and many cardiac surgeons recognize them as having exactly the same final effect as the more expensive ones;
- coated with medications – medications prevent inflammation, blood clots and tissue growth on the stent;
- inert - coated with gold, titanium or silicon carbide, do not react with blood and artery walls;
- with double coating – at the same time they prevent blockage and proliferation of the muscle layer;
- self-absorbing - after 36 months they dissolve and gradually release drugs into the blood that prevent blockage of the vessel.
Types of stents
Risks of intervention
PCI, despite its simplicity, like any surgical intervention in cardiology, involves a number of risks.
This is not only the body’s rejection of the stent installed during the operation, but also a potentially dangerous possibility:
- damage to the vascular wall;
- the occurrence of causeless bleeding (not only external, but also internal);
- death;
- formation of stent thrombosis;
- the onset or progression of a pre-existing acute coronary syndrome;
- development of restenosis;
- soft tissue infection;
- formation of false aneurysms;
- the occurrence of hematomas (including pulsating ones);
- rupture of the coronary arteries (despite the fact that the risk of such a consequence of PCI is minimal, in such circumstances the patient’s death is inevitable).
Despite the risks, it is important to understand that the vast majority of them are due to inappropriate examination of the general condition of the body before percutaneous coronary intervention.
If you follow the cardiologist's recommendations (the doctor must be selected taking into account his experience, qualifications, and patient reviews), the risk of unforeseen situations on the operating table is minimal.
Anticoagulant therapy
All patients without exception after PCI must take drugs to reduce blood clotting - anticoagulants (Warfarin), inhibiting platelet adhesion - antiplatelet agents (Plavix, Cardiomagnyl). They are usually prescribed for 1 month, and then the patient undergoes an examination, including an ECG with stress tests, blood tests, urine tests, examination by a gastroenterologist and other specialists if necessary.
Based on the results obtained, the dose and dosage regimen are changed. In the future, it is necessary to monitor the coagulogram monthly, and other diagnostic methods are recommended once every 3-6 months. Blood thinners should be taken at a maintenance dose for at least 1 year.
Drug therapy also includes tablets for:
- lowering cholesterol levels – Crestor, Vasilip;
- normalization of vascular tone and blood pressure - Prestarium, Diroton;
- improving metabolic processes in the heart muscle - Mildronate, Preductal.
How do PCIs differ from open heart surgeries?
Percutaneous coronary intervention differs from open heart surgery not only in its greater safety, but also in its technique.
In addition, among the characteristic features we can also highlight:
- no need to place a person under general anesthesia for a long time (with age, as well as due to the presence of a number of circumstances, it can be difficult for patients to get out of “medication sleep”);
- shorter rehabilitation process (the integrity of the skin after percutaneous coronary intervention is restored within a few weeks after the operation);
- a large number of contraindications that are “temporary” (for example, feverish conditions, the patient’s refusal to be accompanied further or the inability to maintain contact with the person being operated on);
- there is no need for lengthy preparation for the operation (usually the cardiologist observing the patient recommends taking blood tests to identify pathologies, as well as undergoing an ultrasound examination of individual body systems and obtaining an opinion from specialized specialists).
The equipment used during emergency surgery is less expensive than the “working tools” of surgeons performing open heart surgery. This makes it possible to carry out medical procedures of this type in most hospitals with a cardiology department.
Possible risks
The main risk after PCI is restenosis. This is called repeated blockage of a coronary vessel. It can cause renewed heart pain and even a heart attack. Categories of patients in whom the likelihood of restenosis is high have been established:
- smokers;
- suffering from alcoholism;
- women;
- with diabetes mellitus;
- violating recommendations for diet and physical activity;
- over 65 years of age;
- with excess body weight;
- have had a previous heart attack.
Complications after
After stenting surgery, the following complications are possible (in addition to restenosis):
- increase in temperature - it is considered normal to rise to 37.3 degrees in the first 2-3 days, then this is a sign of infection;
- bleeding from the femoral artery where the catheter was inserted;
- impaired renal function due to the administration of contrast - lower back pain, frequent urination;
- injury to a vessel by a catheter;
- arrhythmia, cardiac arrest, heart attack (frequency below 1%).
They usually appear in the early postoperative period while the patient is in the hospital. After discharge, dangerous symptoms that require urgent medical attention are:
- fever,
- chills,
- severe chest pain,
- burning behind the sternum,
- feeling of interruptions in rhythm,
- sudden weakness
- sweating
Results
As a result of stent installation:
- the spread of an already existing infarction is stopped or its occurrence is prevented in a pre-infarction state;
- the course of angina pectoris becomes easier - attacks occur with higher physical activity, they are shorter in time, and can be relieved with a smaller dose of medication;
- the patient’s quality of life increases, as activity increases and there is a chance to fully restore ability to work;
- the risk of death from heart attack, arrhythmia and heart failure is reduced.
Life after
After the operation, restrictions are set for the first time:
- Excessive physical activity and driving are not recommended for the first day;
- for 7-10 days, bathing, lifting weights from 3 kg, quickly climbing stairs, playing sports (measured walking is useful, but without the appearance of fatigue), sexual intercourse is prohibited;
- For 30-45 days, sunbathing, staying in a sauna, hypothermia, and sudden climate change are contraindicated.
In the first month, the body recovers; a gradual increase in physical activity is necessary. Dosed walking and therapeutic breathing exercises for 30-45 minutes a day are recommended.
Pulse and blood pressure must be monitored daily; they should not be allowed to rise above 90 beats per minute and 130/85 mm Hg. Art. Smoking and alcohol abuse are prohibited. Patients require weight loss if they are obese.
Nutrition after PCI
Diet is one of the mandatory conditions of the rehabilitation period; the following should be excluded from the diet:
- fatty meat (pork, lamb, duck), offal;
- all sausages;
- semi-finished products;
- canned food;
- smoking, pickling, marinades;
- store-bought sauces;
- margarine, sour cream and cheese products;
- heavy cream, sour cream and cottage cheese above 9% fat, butter (up to 20 g);
- nectars, sweet soda;
- cakes, pastries.
Allowed:
- first courses of vegetables and cereals (without meat and fish);
- boiled, steamed, baked vegetables;
- lean chicken and fish (cannot be fried or stewed with oil);
- vegetable salad with a dressing of herbs and lemon juice, a teaspoon of vegetable oil;
- fruits, berries;
- whole grain and bran bread, porridge, crispbread;
- freshly prepared fermented milk drinks without sugar, cottage cheese 2-5%, 1-2 tablespoons of sour cream 10% per day;
- eggs for omelettes, poached, boiled - 3 yolks per week, whites can be used every day;
- legumes – beans, lentils, peas;
- seeds and nuts, honey - 1-2 tablespoons.