Why does myocardial infarction develop?
Our heart is a tireless worker. In one minute it pumps more than five liters of blood and makes about one hundred thousand beats. The heart performs the most important functions for the human body:
- due to rhythmic contractions, it ensures blood flow through the blood vessels;
- saturates organs and tissues with oxygen;
- removes carbon dioxide and other harmful substances from the body.
With the development of myocardial infarction, the heart loses its ability to function normally, which often leads to disability and death.
The main cause of myocardial infarction is atherosclerosis, a chronic vascular pathology caused by impaired lipid and protein metabolism. During the disease, atherosclerotic plaques form in the lumen of blood vessels - dense formations of cholesterol, covered with fibrous tissue on top.
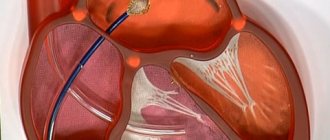
With certain changes in the body (stress, increased blood pressure), vascular spasm occurs, which often leads to rupture of an atherosclerotic plaque with the formation of blood clots. If this occurs in the heart muscle, then acute myocardial infarction develops. If in the intestines, then intestinal infarction, etc.
People with chronic diseases have an increased likelihood of developing myocardial infarction:
- diabetes mellitus;
- hypertension;
- coronary heart disease;
- varicose veins of the lower extremities.
What could cause it to appear?
The main cause of the pathology is damage to the inner lining of the coronary artery. This is a vessel that nourishes the tissues of the heart. As long as its diameter does not narrow and the walls remain elastic, no negative changes occur. Reducing the lumen limits blood flow. A similar picture emerges when:
- atherosclerosis;
- spasm of the coronary arteries;
- increased blood viscosity;
- formation of blood clots - thrombi.
The disease can be triggered by the influence of negative factors, which include:
- hormonal disorders;
- long-term treatment with corticosteroids;
- hypertonic disease;
- obesity;
- smoking;
- alcohol consumption;
- sedentary lifestyle;
- emotional overload.
In rare cases, myocardial infarction can be triggered by other internal pathologies: rheumatism, cancer, severe allergic reactions.
Clinical options for the development of myocardial infarction
The classic form of myocardial infarction is accompanied by a severe pain syndrome of a compressive, tearing, burning nature. The pain is most often localized behind the sternum, but can also radiate to the left arm, left shoulder, lower jaw, and interscapular area. As a rule, the pain lasts more than 20 minutes and is not relieved by nitroglycerin within 5 minutes.
Other symptoms of classic myocardial infarction:
- increased sweating;
- psychomotor agitation;
- feeling of fear of death.
There are also atypical options for the development of myocardial infarction:
- abdominal form. In this case, the patient experiences heartburn, nausea, vomiting, pain in the upper abdomen;
- arrhythmic form. Characteristic signs are heart rhythm disturbances, a feeling of interruptions in the heart;
- asthmatic form. The main symptoms are shortness of breath, suffocation;
- painless form. It is characterized by the absence of pain or the presence of mild pain that occurs at varying frequencies. This form especially often develops in patients with diabetes mellitus and in people who have already suffered a myocardial infarction in the past.
Why is the painless form dangerous? First of all, the development of sudden cardiac death. In addition, if in the acute period a myocardial infarction occurs without clear clinical symptoms, then in the future this can lead to the development of chronic heart failure.
The painless form of myocardial infarction can be recognized by other signs. For example, a person may experience shortness of breath, increased fatigue, and exercise intolerance.
Modern diagnostic methods
If there is a suspicion of a heart attack, there is anamnestic data about coronary heart disease and characteristic clinical signs, the doctor prescribes a diagnostic program. It consists of the following methods:
- electrocardiogram;
- laboratory diagnostics.
Let's take a closer look at these research methods.
An electrocardiogram is a graphic representation of the conduction of an impulse along the myocardial fibers. If conductivity is impaired due to necrosis, this will be reflected in the recording. Based on changes in the ECG, the localization of the necrosis zone can be distinguished. Also, on the graph you can see the phase of the infarction - acute or subacute.
General blood analysis
There are no specific changes observed in a general blood test and therefore a diagnosis cannot be made on its basis. During a heart attack, leukocytosis develops, which occurs several hours after the start of the process and reaches a maximum by the end of the day. The elevated level lasts for several days and gradually returns to normal. Leukocytes do not increase significantly, as, for example, with infectious pathology, which allows for differential diagnosis. This is important in case of an atypical clinical picture of myocardial infarction, when the doctor may suspect several pathologies. In a general blood test, you can also see an increased ESR, which remains this way for several weeks. Eosinophils also increase and remain elevated for about a week.
Blood chemistry
Alanine aminotransferase (ALT)
Indicator of destruction of hepatocytes and cardiomyocytes. It increases with hepatitis of various etiologies, heart attack, toxic damage to internal organs. ALT is an active component of liver metabolism, an enzyme that accelerates the metabolism of amino acids. The highest concentration of the substance is found in the cells of the liver, kidneys, heart, as well as in skeletal muscle tissue. Since its localization is the cytoplasm, it is released into the blood when the cell membrane is destroyed. The more massive the area of destruction, the higher the concentration of the enzyme in the blood. The peak activity of the enzyme during a heart attack is 12 hours.
An increase or normalization of ALT levels is a marker of the condition of patients of various profiles with diseases of internal organs and soft tissues. Depending on the disease, ALT can increase moderately or acutely, for example, the highest degree of concentration is observed in hepatitis.
In case of a heart attack, the de Ritis coefficient is used, which consists of comparing the activity of AST and ALT. If the value exceeds the norm, this indicates a heart attack, and if it is below its value, necrosis of the renal tissue or the active phase of hepatitis may have developed. Naturally, a diagnosis is not made based on the ALT indicator. For this, more specific markers are used. The level of transaminases is checked in a general biochemical analysis for differential diagnosis and monitoring of the patient’s general condition.
Aspartate aminotransferase (AST)
Marker of the condition of heart and liver tissues. Increases in viral hepatitis, toxic damage to heart tissue and hepatocytes. It is also used for preventive examination, if necessary, to confirm or exclude a heart attack. This substance is responsible for the exchange of amino acids in cells, so the largest amount is found in the cells of the liver, heart, skeletal muscles and red blood cells. If the cells of these organs are damaged, transaminase is released into the blood, where its increase can be detected. There is an acceptable level of the enzyme in the blood, because organ cells are periodically destroyed, but in pathological conditions this indicator increases several times or tens of times. The peak concentration in the blood is 12 hours after the onset of a heart attack. A comparison of ALT and AST indicators is also used. Each of these enzymes increases in certain pathologies, and during a heart attack their ratio is assessed. AST is not a specific indicator for a heart attack; it complements the overall picture of laboratory testing.
Creatine kinase MB
This substance is an isoenzyme, a marker of the condition of the heart muscle. Takes part in the metabolism of creatine and creatine phosphate. This substance is contained only in the myocardium, and therefore increases in its diseases - myocarditis, heart attack, rhabdomyolysis, pericarditis. The level of the substance is a marker during the acute and subacute phases of the process. A short-term increase in the indicator is observed during cardiac surgery, which reflects the reaction of the myocardium to treatment. The maximum concentration during a heart attack is observed 12 hours after the onset. High activity indicates a significant size of the affected area. The increase in this CPK fraction is compared with the general indicator of the substance in the body. In principle, assessment of the level of CPK MB is used for early diagnosis of myocardial damage, as well as for differentiating the condition from other diseases. An increase in the marker can indicate, in addition to a heart attack, conditions such as shock, poisoning and intoxication, infectious lesions of heart tissue.
Troponin I
A protein that is found in high quantities in skeletal muscles and myocardium. There are varieties of this protein that are responsible for different phases of muscle contraction. All these proteins are cardiac-specific and indicate the state of the myocardium. Damage to cardiac myocytes leads to the release of the substance into the blood, where it can be detected using laboratory testing. The area of necrosis affects the level of increase in troponin levels in the blood. Troponin I is the most sensitive and specific for infarction. Elevated troponin persists for 5-6 days after the onset of the pathological process.
Myoglobin
This is a protein that is found in muscle cells and contains iron molecules. Similar in structure to hemoglobin, an iron-containing blood protein. The function of myoglobin is also similar - it transports oxygen to myocytes, muscle cells. With necrosis, muscle cells are destroyed, myoglobin is released and enters the bloodstream, where it can be detected. Protein is excreted from the blood along with the kidneys. It can be detected in the blood within a few hours after the onset of the pathological process; within 2-3 days it can still be detected. This marker is one of the first to react, which increases its diagnostic value. With necrotic changes, it increases 7-10 times, depending on the area of necrosis. For comparison, the period of peak increase in other markers is 12 hours, while for myoglobin it is 6 hours. Normalization of analyzes occurs just as quickly. They can remain elevated for longer than a day if complications occur, for example, expansion of the area of necrosis. Sometimes new foci occur, then myoglobin increases again, which requires dynamic monitoring of the indicator. A negative test result is also important, which, in comparison with the clinical picture, allows one to exclude pathology. In addition to a heart attack, myoglobin may indicate long-term compartment syndrome. muscle pathologies, inflammatory processes.
First aid for myocardial infarction
In providing first aid, the principle of the “golden hour” is very important, from the moment the symptoms of the disease appear until the patient is admitted to the hospital. In critical situations, even more rapid action is required. The severity of the condition during a heart attack depends on how much the lumen of the vessel is blocked by a thrombus. If occlusion (complete obstruction) of a vessel occurs, a critical condition develops. The patient has 20–40 minutes left, after which necrosis of the cardiac tissue occurs.
It is very important not to wait for the pain to subside or for the work day to end. If symptoms characteristic of a heart attack appear, you should immediately take the necessary medications and call an ambulance.
Before doctors arrive, a person with coronary syndrome should be provided with first aid.
Correct algorithm of actions:
- Place the person in a semi-sitting position. For example, you can put the patient in bed and place pillows under his back. A semi-sitting position reduces the load on the heart.
- Provide the patient with complete physical and mental rest, try to calm him down. Physical and emotional stress increases myocardial ischemia and increases the need for oxygen in the heart muscle.
- Free your body from constrictive elements of clothing - remove your tie, belt, unbutton your shirt collar.
- Create an influx of fresh air - open a window or vent.
- Give the patient half a tablet of aspirin to chew. This will reduce the area of the heart attack and reduce the risk of death.
- If possible, you need to measure the person's blood pressure.
- If you have high blood pressure, be sure to give a drug for hypertension, as well as nitroglycerin. Nitroglycerin capsules are placed under the tongue and sprayed under the root of the tongue as a spray.
Therapy
The patient is taken to intensive care, where complex therapy is carried out. When treating a heart attack, the speed of reaction is very important: the faster the patient gets to the hospital and receives proper care, the higher the chances of a positive outcome and the absence or minimum number of complications.
Doctors use drugs that help dissolve a blood clot, painkillers, and medications to lower blood pressure and reduce blood circulation. Also, as part of treatment, it is necessary to achieve a decrease in heart rate, which is achieved by taking beta-blockers.
The rehabilitation period after inpatient treatment is no less important than the therapy itself. The recovery period lasts up to 6 months. The patient may be prescribed medications that must be taken constantly. Also, to maintain normal condition, it is necessary to follow a diet, in particular, eliminating fatty and fried foods from the diet, as well as stopping smoking and drinking alcohol.
If the doctor's recommendations are followed, the patient can count on a long and fulfilling life.
Anaprilin
- Has a hypotensive effect, reduces heart rate;
- Increases the resistance of the heart muscle to oxygen starvation;
- Prevents the development of arrhythmia.
More details
THERE ARE CONTRAINDICATIONS. BEFORE USE, READ THE INSTRUCTIONS CAREFULLY OR CONSULT A DOCTOR
Complications
Complications of myocardial infarction are early and late. As a rule, early complications develop in the first hours of a heart attack during hospitalization or for several days after the attack. The occurrence of complications is significantly influenced by the timeliness of first aid and hospitalization.
The most common early complications include:
- disturbances in the rhythm and conduction of the heart, which in most cases are fatal;
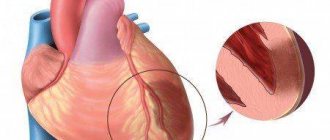
- rupture of the heart muscle;
- development of acute left ventricular failure, which is accompanied by pulmonary edema.
The last stage of left ventricular failure is cardiogenic shock, in which myocardial contractility sharply decreases and the blood supply to all organs is disrupted. The condition is accompanied by a strong drop in blood pressure, a decrease in body temperature, pale skin, difficulty breathing, oliguria, and loss of consciousness. The probability of death with cardiogenic shock is 90%.
Late complications of myocardial infarction:
- early post-infarction angina. A person who has such a complication does not tolerate even the slightest physical activity. Any activity causes squeezing pain behind the sternum. Even simple self-care activities lead to pain. The pain is less severe than during a heart attack itself, but quite painful;
- chronic heart failure, which is accompanied by shortness of breath, edema of the lower extremities, enlarged liver, and the development of chronic left ventricular aneurysm.
What it is
Myocardial infarction, or heart attack, most often occurs in older patients. The risk group includes women over 55 years of age and men over 45 years of age.
Doctors classify pathology according to the time of its occurrence:
- primary infarction – occurring for the first time;
- recurrent infarction – diagnosed within 1.5 months after the first attack;
- repeated heart attack – occurring after 6 weeks from the date of the first incident.
Several departments can be affected at once. In this case, we are talking about an extensive heart attack. Pathology can only affect the left ventricle - its septum or walls. The tissue of the right ventricle dies less often.
Rehabilitation
a cardiologist twice a month . During the second year after the attack, it is necessary to visit a general practitioner once every four months. If necessary, each of these specialists can refer the patient to a rehabilitation center or sanatorium.
For successful rehabilitation, it is important for the patient to strictly follow all the doctors’ recommendations:
- take necessary medications. These may be statins, anticoagulants, antihypertensive drugs;
- maintain a balance between sleep, work and rest;
- walk in the fresh air more often;
- avoid stress. After a heart attack, a person should receive only positive emotions.
What symptoms of a microinfarction do women experience?
The disease is very “insidious”, since the symptoms of a microinfarction in women are not always noticeable. Because of this, the diagnosis is made after the fact when other diseases occur.
One of the first symptoms is sudden chest pain. Pain may be present in the left side of the shoulder girdle, shoulder blade and jaw.
According to statistics, women are less likely to pay attention to the symptoms of a heart attack, as they are less sensitive to pain. Also, microinfarction often goes unnoticed by patients over 55-60 years of age and diabetics.