Description of drugs in Lesson No. 15
Description of drugs in Pathological Anatomy in Lesson No. 15
(This is an indicative description, not a cathedral one, some drugs may be missing, as is the description of previous years)
- LESSON No. 1 5
coronary heart disease
ELECTROGRAM Acute ischemic myocardial dystrophy (demonstration).
Mitochondria are swollen, their cristae are destroyed. Glycogen granules are not detected.
MICROPREPARATION No. 110 Atherosclerosis and thrombosis of the coronary artery of the heart.
The lumen of the coronary artery is narrowed due to an atherosclerotic plaque, in the center of which fatty protein masses, cholesterol crystals and lime deposits are visible (stage of atherocalcinosis). The plaque cover is represented by hyalinized connective tissue. The lumen is obstructed by thrombotic masses consisting of fibrin, leukocytes, and erythrocytes.
MICROPREPARATION No. 111 Myocardial infarction (necrotic stage). Demonstration, see earlier
MICROPREPARATION No. 111A Myocardial infarction. Organization stage.
A zone of necrosis surrounded by a demarcation shaft (granulation tissue with a large number of vessels). An area of necrosis with lysis of nuclei and clumpy disintegration of the cytoplasm of cardiomyocytes, surrounded by a zone of demarcation inflammation, in which full-blooded vessels, hemorrhages, and accumulations of leukocytes are identified.
MICROPREPARATION No. 215 Disappearance of glycogen from the ischemic zone of cardiomyocytes.
The absence of glycogen in the focus of necrosis is expressed by the pale color of the stained preparation. Cardiomyocyte nuclei are lysed. Thick red fibers are the remains of necrotic tissue. Around them is bluish tissue with many nuclei - granulation tissue in the form of a mesh (PMN, fibroblasts, vessels, connective fibers, BM fragments).
MICROPREPARATION No. 45 Large focal cardiosclerosis.
Heme-Eoz staining (demonstration). Staining with picrofuchsin according to Van Gieson: an irregularly shaped area of cardiosclerosis is red. The focus of sclerosis is irregular in shape, with pronounced hypertrophy of cardiomyocytes along the periphery. When stained for connective tissue (according to Van Gieson), the scar is stained red, cardiomyocytes - yellow.
MACROPROOF Transmural myocardial infarction with cardiac rupture.
In the anterior wall of the left ventricle, a focus of necrosis is visible, irregular in shape, whitish-yellowish in color, flabby consistency, with a hemorrhagic rim. On the endocardial side – thrombotic masses attached to the endocardium, on the pericardial side – fibrous deposits. In the area of necrosis there is a slit-like hole whose walls are saturated with blood. In the pericardial cavity there is blood and thrombotic masses.
MACROPROOF
Subendocardial myocardial infarction with mural thrombus.
A focus of necrosis with a dark red rim is visible in the left ventricle. In the area of projection of necrosis on the endocardium, dense, dry, crumbling masses of gray-red color (thrombotic masses) are visible.
MACROPROOF Large focal cardiosclerosis.
- the heart is enlarged in size and weight
- in the area of the left ventricle, an irregularly shaped focus is determined, represented by dense whitish connective tissue.
MACRO PREPARATION
Chronic cardiac aneurysm
- the heart is enlarged in size
— the wall of the left ventricle in the apical region is thinned, whitish, represented by scar connective tissue, and bulges.
— the myocardium around the bulge is hypertrophied
- the aneurysm cavity is filled with crumbling, dense, dry gray-red masses (thrombotic masses) associated with the aneurysm wall
I — 1 — 05 Circulatory disorders-2
2
LESSON I – 05
Circulatory disorders: stasis, thrombosis, embolism, ischemia, infarction.
Stasis
– a sharp slowdown or cessation of blood flow in the vessels of the microvasculature (capillaries, venules). In the mechanism of development of stasis, aggregation of erythrocytes (sludge phenomenon) is important.
Microslide
No. 82
-
“Staz in the capillaries of the brain during malaria”, (G-E) - demonstration.
The capillaries and venules are sharply dilated, filled with sticky red blood cells, in which a large amount of black-brown pigment is visible - hemomelanin, which gives the brain a slate-gray color. The substance of the brain is swollen. Prolonged stasis in the brain can lead to severe hypoxia and the development of focal necrosis of the brain substance. Clinically, it manifests itself as cerebral coma.
Thrombosis
- intravital blood coagulation in the lumen of blood vessels or cavities of the heart. The resulting blood clot is called a thrombus.
The mechanism of thrombosis involves both local (changes in the vascular wall, slowdown and disruption of blood flow) and general (disruption of the relationship between the coagulation and anticoagulation systems in the regulation of the fluid state of the blood, changes in blood quality) factors.
Thrombosis
consists of
4 stages
:
1. platelet agglutination; 2. fibrinogen coagulation and fibrin formation; 3. agglutination of erythrocytes 4. precipitation of plasma proteins.
Depending on the structure and appearance, white, red, mixed (layered) and hyaline blood clots are distinguished. In relation to the lumen of the vessel, the thrombus can be parietal or obstructive (obstructive thrombus). When the blood clot grows, they speak of progressive thrombosis.
Electron diffraction pattern
“Second stage of thrombus formation” - demonstration.
In the area of destroyed endothelium, accumulations of degranulated platelets and fibrin are visible.
In a mixed (layered) thrombus, a head, body and tail are distinguished.
Macro-drug
“Parietal thrombus in the aorta” - description.
The intima of the aorta is uneven, rough, with ulcerations. A gray-red, dryish formation with a corrugated, dull surface is located near the wall, fixed to the intima in the region of the head. The body and tail of the thrombus lie freely in the lumen of the vessel.
Macroscopic specimen
“Thrombi in the deep veins of the lower extremities” (cross section) - description
. Dark red dryish masses obstruct the lumen of the veins; they are intimately connected with the inner lining of the vessels. Red blood clots usually form in the veins. This is the most common location of blood clots, especially in patients with cardiovascular insufficiency, when venous congestion develops.
Microslide
No. 5 “Mixed thrombus in a vessel”, (G-E) - draw
. The lumen of the vein is obstructed by a mixed thrombus. It consists of fibrin threads, between which red blood cells, platelets, and leukocytes are visible.
Blood clot outcomes
may be favorable or unfavorable.
Favorable
- aseptic autolysis (in small vessels), organization, canalization and vascularization of the thrombus;
unfavorable -
septic autolysis (purulent fusion of a blood clot), thromboembolism.
Microslide
No. 32 “Organizing thrombus”, (G-E) - demonstration
. Most of the thrombotic masses in the lumen of the artery are replaced by connective tissue growing from the intimal side. In it, cracks lined with endothelium are visible (thrombus canalization).
Embolism
- circulation in the blood (or lymph) of particles not found under normal conditions and blockage of blood vessels by them. Emboli can move along the blood flow (orthograde embolism), against the blood flow (retrograde embolism), through defects in the septa of the heart from the systemic circulation to the small circulation (paradoxical embolism). Depending on the type of embolus, there are: thromboembolism, fatty, air, gas, tissue (cellular), microbial, foreign body embolism.
Thromboembolism
is
the most common type of embolism. Pulmonary embolism is of greatest clinical importance.
Macrodrug
“Pulmonary artery thromboembolism” - description.
In the common trunk of the pulmonary artery, loose gray-red worm-like masses with a corrugated surface are visible.
With thromboembolism of the common trunk and large branches of the pulmonary artery, sudden death occurs due to the pulmonary-coronary reflex. The most common source of pulmonary embolism are thrombi of the veins of the lower extremities, pelvic tissue, and hemorrhoidal plexus.
Microslide
No. 92 “Fat embolism of the lung”
,
(Sudan III ) - description
. The capillaries of the interalveolar septa of the lung are filled with droplets of fat, colored yellow-red.
Fat embolism of the lung develops with traumatic crushing of subcutaneous fat, with a fracture or gunshot wound of long tubular bones (bone marrow damage), after childbirth (crushing pelvic tissue).
An example of a bacterial embolism is embolic purulent nephritis.
Macrodrug
“Embolic purulent nephritis” - demonstration.
The kidney is enlarged in size; in the cortex and medulla, multiple small yellowish foci (foci of purulent inflammation) are visible, some of them are surrounded by a red rim (area of hemorrhages).
Cellular embolism underlies tumor metastasis.
Macrodrug
“Metastases of stomach cancer to the liver” - description.
The liver tissue is almost completely replaced by tumor nodes of a rounded yellowish color with retraction in the center of individual nodes.
DIC syndrome
– widespread blood coagulation in the vessels of the MCR. It manifests itself as hypercoagulation and the simultaneous development of hemorrhagic syndrome (consumptive coagulopathy). The main reason is autoinfusion of tissue thromboplastins in extreme conditions of the body: embolism, severe acute hypoxia, burns, infectious-septic conditions, intoxication, paraneoplastic syndrome, transfusions of incompatible blood, plasma, shock.
Shock –
circulatory collapse, accompanied by tissue hypoperfusion and decreased oxygenation.
Types of shock –
hypovolemic, cardiogenic, septic, vascular.
Stages of shock
:
1.
Non-progressive (early) stage;
2.
– progressive stage;
3.
– irreversible stage.
Morphological changes in internal organs during shock:
kidneys - necrotizing nephrosis, lungs - edema, atelectasis, adult respiratory distress syndrome, liver - centrilobular necrosis, brain, gastrointestinal tract - hemorrhages.
Anemia
called reduced blood supply or bleeding of tissue, organ, part of the body as a result of insufficient blood flow.
It can be general and local. General ( anemia) anemia
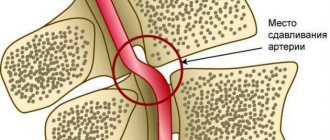
Local (ischemia)
- develops as a result of spasm, compression of the artery or obstruction of its lumen, morphological changes - parenchymal atrophy and sclerosis.
An example of severe anemia
may be a kidney (kidney) drug for anemia.
Macrodrug
“Anemia of the kidney in anemia” - demonstration.
The kidney tissue is pale, almost white, somewhat reduced in volume, with a flabby consistency.
Heart attack –
tissue necrosis caused by cessation or significant reduction of arterial blood flow in an organ or part of the body.
Types of heart attacks (by color): white
– myocardium, brain, kidneys, spleen;
red
– lungs, small intestine, ovaries. The shape of infarctions can be wedge-shaped (triangular), or have an irregular shape, depending on the characteristics of the angioarchetectonics of the organ.
Macropreparation
“Splenic infarction” - demonstration .
Under the capsule of the spleen, a wedge-shaped area is visible, white in color, dense in consistency, clearly demarcated from the surrounding tissues; on the capsule - fibrin overlays.
Macrodrug
“Myocardial infarction” - description.
In the myocardium (in the anterior wall of the left ventricle - the most common location of myocardial infarction) a yellow-white focus of necrosis of irregular shape is visible, surrounded by a hemorrhagic rim.
Microslide No. 111
“Myocardial infarction”, (G-E) – drawing.
An area of necrosis with lysis of nuclei and clumpy disintegration of myoplasm, delimited by a demarcation zone with full-blooded vessels, areas of hemorrhage, and an accumulation of inflammatory infiltrate cells (mainly polymorphonuclear leukocytes).
Macrodrug
“Hemorrhagic pulmonary infarction” - description.
In the lung, an airless area of triangular shape, dark red color, dense consistency, with its base facing the pleura, is revealed. Fibrin is deposited on the pleura at the site of the infarction.
Microslide
No. 3 “Hemorrhagic pulmonary infarction” (H-E) - description.
In the zone of necrosis, a rupture of the interalveolar septa and the absence of nuclei in the septal cells and alveolar epithelium are determined; the area of necrosis is saturated with blood; in the zone of demarcation inflammation there is an accumulation of leukocytes; along the periphery - lung tissue with increased airiness - emphysema.
Types of rehabilitation
Improvement of health is promoted by:
- drug therapy for circulatory disorders;
- physical therapy and physiotherapy;
- working with a psychologist, gaining knowledge at a health school;
- treatment in a specialized sanatorium.
The attending physician develops the program individually, taking into account:
- the nature of the heart attack and the severity of the condition;
- age;
- severity of heart failure;
- the presence of complications and concomitant diseases;
- physical training.
Drug rehabilitation
Medicines are prescribed during the acute period. After improvement in indicators, you also need to take medications prescribed by your doctor.
When preparing drug therapy, the following are taken into account:
- presence of concomitant diseases;
- causes of thrombosis;
- characteristics of the body.
The condition is kept under control, and the treatment program is adjusted if necessary.
Thanks to regular medication use:
- blood pressure levels stabilize;
- it is possible to prevent the development of arrhythmia and angina pectoris;
- lipid metabolism and blood clotting are normalized;
- the condition of chronic heart failure improves.
Physical rehabilitation
Physical rehabilitation after a heart attack begins during the hospital stay. From the second day, the simplest exercises are shown - you can bend and straighten your toes and fingers, lower your bent legs to the left and right. Between approaches there is a rest - 10-30 seconds are allotted for it.
After transfer to the cardiology department, physical activity increases. Most of the movements are performed in a sitting position. Head turns, raising arms forward and up, and other simple exercises are added. The patient gets up and begins to walk around the room. Then he goes for walks in the corridor. Later he is allowed to go up and down the steps.
After discharge, a gradual increase in activity is indicated:
- A complex of exercise therapy is performed taking into account the physical capabilities of the person. It is selected individually, the loads should be dosed and moderate.
- Simple work around the house and in the garden brings benefits (heavy lifting and other hard work is prohibited).
Shown:
- walks in the open air;
- going up/down stairs;
- cardio exercises;
- Nordic walking;
- jogging and other aerobic exercise.
During classes, indicators are monitored. The initial loads should not be long - a quarter of an hour is enough. Gradually, the duration of classes is increased by five minutes a day and stopped at an hour.
Refusal of physical activity and prolonged bed rest increase the risk of thromboembolic complications and congestive pneumonia. As a result of physical inactivity, the functioning of the gastrointestinal tract is disrupted, muscles weaken, and the quality of life deteriorates.
Psychological rehabilitation
After a heart attack, the psychological state seriously deteriorates. The patient feels helpless and fears the next attack and death. Increased nervousness and irritability are common symptoms after illness. If you ignore them, there is a risk of developing neurosis and depression. A psychologist will help improve your psychological mood and form positive thinking. The environment plays an important role - loved ones should provide psychological support.
Features of acute myocardial infarction and its symptoms
Acute myocardial infarction is the death of a section of the heart muscle caused by a circulatory disorder. Heart attack is one of the main causes of disability and mortality among adults.
Causes and mechanisms of vascular incompetence of the heart
A heart attack can be considered an acute form of coronary heart disease or its complication.
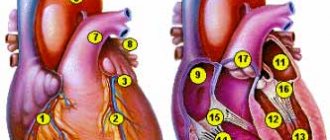
The peculiarities of the heart - constant contractions of the myocardium - determine a very high level of metabolic processes in its cells, high consumption of oxygen and nutrients. This mode of activity requires an uninterrupted flow of highly oxygenated (oxygen-rich) blood, which is provided by an extensive network of cardiac vessels starting from the aorta in the form of coronary (coronary) arteries.
The downside to the effectiveness of the heart muscle is its high sensitivity to oxygen starvation. If there is a malnutrition in the myocardium, pathological phenomena develop that very quickly become irreversible.
If the lack of blood flow is not critical, reversible ischemia (anemia) of the heart muscle occurs, which is manifested by anginal pain in the chest. When the flow of blood to a certain area is completely stopped, a cascade of pathological processes develops - the accumulation of toxic metabolic products that are not excreted, the transition to an anaerobic (oxygen-free) mode of operation using the internal energy reserves of cells.
The body's own reserves of energy carriers (glucose and ATP) are very quickly (in about 20 minutes) depleted, and the bloodless section of the heart muscle dies. This is myocardial infarction - necrosis, the size of which depends on the level of vessel occlusion (large or small branch), the rate of onset of ischemia (with gradual cessation of blood supply, partial adaptation is possible), the patient’s age and many other factors. For example, acute transmural myocardial infarction (with necrosis of the entire thickness of the heart muscle), which has a very severe course, develops when a large branch of a coronary vessel is occluded (blocked).
Among the causes of impaired blood supply to the myocardium, the most common is a block of the lumen of the vessel by an atherosclerotic plaque or thrombus (these phenomena can be combined) . In addition, a sharp spasm of the coronary arteries is possible under the influence of physical (cold) or chemical (poisons, drugs) factors. Severe anemia, in which there is a sharp decrease in the content of hemoglobin in the blood, and, consequently, its ability to transport oxygen, can also cause myocardial ischemia. Inconsistency of blood supply with increased needs occurs with sudden hypertrophy of the heart muscle - cardiomyopathy.
Predisposing factors for the development of heart attack
Some diseases and pathological conditions are increased risk factors for the development of acute myocardial ischemia. These include:
- Diabetes.
- Hypertonic disease.
- Coronary heart disease (CHD), manifested by attacks of angina (especially its unstable forms).
- Increased levels of cholesterol and some fractions of lipoproteins in the blood.
- Excessive body weight.
- Smoking.
- Alcohol abuse.
- Errors in diet (high consumption of salt, animal fats).
- Cardiac arrhythmia.
- Prolonged stressful situations.
- Age over 60 years (although in recent years there has been a “rejuvenation” of heart attacks).
- Male gender (after 70 years, the number of men and women suffering from a heart attack equalizes).
Classification of ischemic myocardial injury
There are different criteria for classifying a heart attack. Some of them:
- The size of the damage zone is large-focal and small-focal.
- According to the depth of damage to the heart muscle - transmural (throughout the entire thickness of the heart wall), intramural (necrosis in the thickness of the wall), subendocardial (damage to the inner layer), subepicardial (outer layer).
- According to topography - left ventricular (anterior wall, posterior and lateral walls, interventricular septum), right ventricular.
Symptoms of a heart attack
In the development of the pathological process, several periods are distinguished, each of which has its own duration and symptoms.
The pre-infarction period can last from several minutes to months. It is characterized by an increase in the frequency of angina attacks and an increase in their intensity.
The most acute period , in which ischemia and necrosis of the heart muscle develops, lasts up to several hours. It may have a typical or atypical course.
The painful, or anginal, variant is typical (about 90% of all cases). It is characterized by high-intensity pain behind the sternum of a burning or pressing nature, which can radiate (give) to the left limbs, jaw, and neck. There may be fear of death, sweating, pale or reddened facial skin, and shortness of breath. The severity of pain depends on the size of the affected area - large-focal infarction causes more severe symptoms than small-focal infarction. The pain is not relieved by taking nitroglycerin.
Atypical variants can occur in the asthmatic type (have symptoms of an attack of bronchial asthma), abdominal (with symptoms of an acute abdomen), arrhythmic (in the form of an attack of cardiac arrhythmia), cerebral (with impaired consciousness, dizziness, paralysis, visual impairment).
The acute period lasts about 10 days. The necrosis zone is finally formed and delimited, absorption of decay products and scar formation begins. The pain syndrome disappears or decreases. Possible increase in temperature, hypotension and heart failure.
The subacute period (about two months) is the stage of scar formation and thickening. There is no pain syndrome, the condition is gradually improving. Well-being in this period is largely determined by the nature and extent of changes that have occurred in the heart muscle.
The post-infarction period , or rehabilitation (up to six months), is characterized by the absence of clinical and laboratory signs of a heart attack (changes on the ECG remain - they will remain for life), however, in this phase, the development of heart failure, angina pectoris and recurrent heart attack is possible.
Complications of myocardial infarction
Acute myocardial ischemia, being a serious condition in itself, can be further aggravated by the addition of complications.
The most common complications:
- Heart rhythm disturbances (paroxysmal tachycardia, extrasystole, atrial fibrillation). A situation such as the appearance of ventricular fibrillation with the transition to fibrillation can cause the death of the patient.
- Heart failure is associated with a disruption in the activity of the left ventricle in pumping blood through the vessels. It can lead to pulmonary edema, cardiogenic shock and death due to a sharp drop in pressure and cessation of renal filtration.
- Pulmonary embolism can lead to pneumonia, pulmonary infarction, and death.
- Cardiac tamponade can occur when the heart muscle ruptures in the area of the infarction and blood leaks into the pericardial cavity. The condition is life-threatening and requires immediate attention.
- Acute cardiac aneurysm is a bulging area of scar tissue with extensive damage to the myocardium. In the future, it can cause the development of heart failure.
- Thromboendocarditis is the deposition of fibrin on the inner surface of the heart. Its separation can cause a stroke, mesenteric thrombosis (closure of a branch of the vessel feeding the intestine) with subsequent necrosis of a section of the intestine, and kidney damage.
- Post-infarction syndrome is the general name for long-term complications (pericarditis, pleurisy, arthralgia).
Diagnosis of heart attack
In the diagnosis of a heart attack, data from anamnesis (circumstances of the course of the disease and previous life, ascertained by interviewing the patient and his relatives), laboratory and instrumental research methods are important.
Anamnesis
Past attacks of chest pain of varying frequency and intensity, as well as risk factors (smoking, stress, chronic diseases) are identified. During examination, it is possible to identify excess weight, indirect signs of high blood pressure (capillary network on the face), etc. Substernal pain lasting more than 20 minutes is considered one of the diagnostic criteria for a heart attack.
Laboratory methods
Laboratory research methods for a heart attack reveal the following changes:
- Blood clinic. Leukocytosis (increased number of leukocytes), increased ESR.
- Biochemistry of blood. Increased activity of the enzymes AlT, AST, LDH, creatine kinase, myoglobin, which is an indicator of damage to the heart muscle. Changes in the level of electrolytes and iron are possible.
Instrumental research methods
- ECG – characteristic signs of a heart attack (negative T wave, pathological QRS complex, etc.). Taking a cardiogram in different leads helps determine the location of the necrotic focus (for example, the anterior or posterior wall of the left ventricle, etc.).
- EchoCG – local (limited) violation of contractility of the affected ventricle.
- Coronary angiography reveals narrowing or blockage of the vessel supplying the myocardium. It should be noted that when carrying out this research method, it can also be used to provide assistance (after supplying a contrast agent through the same catheter, a drug is injected into the vessel or an expander stent is installed).
Treatment of myocardial infarction
Emergency care (performed directly during a painful attack and then in a specialized clinic):
- Providing the patient with complete rest.
- Give sublingual (under the tongue) nitroglycerin and Corvalol orally.
- Immediate transportation for further treatment to the cardiac intensive care unit (preferably on specialized resuscitation transport).
Specialized treatment
- Relief of pain syndrome (narcotic analgesics and antipsychotics are used).
- Dissolution of a blood clot located in a coronary vessel by introducing special thrombolytic agents (streptase, cabinase). The method is very effective, but has a time limit - assistance must be provided within the first hour after the attack; subsequently, the percentage of saved myocardial mass rapidly decreases.
- Antiarrhythmic drugs.
- Improving metabolic processes in the heart muscle.
- Reducing the volume of circulating blood to reduce the load on the heart.
- Surgical methods of treatment - balloon angioplasty of the coronary vessels, insertion of a stent (tubular spacer), coronary artery bypass grafting (providing bypass blood flow by placing a shunt on the damaged vessel).
- Anticoagulants (heparin, aspirin) to reduce blood clotting and prevent thrombosis.
The prognosis for a heart attack is always serious and depends on the volume of the affected myocardium, the localization of the necrotic focus (for example, if the conduction system of the heart is involved in the area of damage, the prognosis worsens), the patient’s age, concomitant diseases, timeliness of treatment, the presence of complications, etc. The percentage of residual effects and occurrence is high. disability.
After passing the acute period, patients are shown rehabilitation with a gradual increase in the level of stress. In the future, medical supervision and prophylactic use of antianginal drugs are necessary.
Prevention of a heart attack is the cessation of bad habits, the fight against excess weight, a balanced diet, work and rest, and timely treatment in case of angina pain.
Objectives and principles of rehabilitation after a heart attack
Due to the limited functionality of tissues healed after necrosis, circulatory failure occurs.
The main goals of rehabilitation of a patient who has suffered a myocardial infarction:
- recovery from a serious condition;
- normalization and stabilization of the cardiovascular system;
- adaptation of the body to changed conditions.
Other tasks:
- formation of the correct psychological attitude of the patient - he must be ready for long-term rehabilitation with strict adherence to medical recommendations;
- prevention of complications and relapses;
- preparing the body for stress.
If rehabilitation after a heart attack is carried out correctly, then a speedy return to a full life and work becomes possible. An optimistic forecast for life expectancy is given.