Forms of angina pectoris
IHD exertional angina is divided into forms:
- First appeared. The diagnosis is made if no more than one month has passed since the attack. The course of the disease occurs in two variants - angina regresses (disappears) or becomes stable angina. The first signs of pathology may be harbingers of a heart attack.
- IHD stable angina pectoris. A persistent form of the disease with attacks lasting more than one month. It is characterized by the appearance of stereotypical symptoms in the patient under the load of one force.
- Progressive angina pectoris. Its development is indicated by an increase in severity and an increase in the duration and frequency of pain attacks when the body is exposed to normal stress.
Angina pectoris stage or otherwise functional classes (FC):
- 1 (first) FC. The usual load does not cause changes in well-being. Painful attacks occur against the background of excessive stress - after climbing several flights of stairs, while walking quickly.
- Second FC. The patient's physical activity is limited. An attack can be triggered by walking 500 meters or more, climbing 1-2 flights of stairs, walking in windy weather or frost, or psycho-emotional agitation.
- Third FC. The patient's physical activity is kept to a minimum. The attack appears after walking a distance of 100 meters, or when climbing one flight of stairs.
- Fourth FC. Physical activity is limited. A painful attack also occurs at rest.
Angina pectoris FC (functional classes) allows the doctor to correctly determine the amount of physical activity and select medications.
The essence and typology of forms of the disease
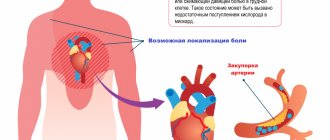
The heart, the main muscle of the body, receives nutrition through the supply of oxygen and nutrients through the arteries.
The daily requirement may increase if a person performs a certain physical activity. Accordingly, blood flow to the main organ increases. The coronary and coronary arteries, which “serve” the heart, come from the aorta. If they are not normal, blood flow is disrupted. This means that a certain part of the heart muscle will not receive enough oxygen and the necessary substances for normal functioning.
This failure is called ischemia. If this condition lasts more than 30 minutes, cardiomyocytes in the heart begin to die, which leads to myocardial infarction. The pathology can become more active when the permissible level of physical activity is exceeded and is accompanied by pain.
There are 4 functional classes of the disease (FC). The main criterion for differentiation is the severity of the form and the permissibility of physical activity:
- FC 1 is a relatively mild degree of the disease, in which moderate exercise is allowed. An attack is possible only in case of extreme physical stress.
- FC 2 involves restrictions on physical activity. This class includes patients whose angina attack begins after walking 500 m or when climbing stairs to the second floor. In addition, patients are not recommended to walk in cold and windy weather, to be active immediately after waking up from sleep, or to experience emotional stress. All this can also provoke a deterioration in well-being.
- FC 3 significantly limits a person’s physical activity. An attack can be triggered by walking at an average speed for 100-500 m and climbing a flight of stairs.
- FC 4 is the most severe form. This is a disability in which seizures can occur even when at rest.
The most common form among heart patients is FC 3, which is regarded by doctors as a disability. In combination with other diseases, for example, tachycardia or arrhythmia, ischemic heart disease (IHD) angina pectoris can provoke attacks for no apparent reason when the patient is at rest.
It is also worth noting that patients with FC 3 disease can usually control their abilities well. They are also able to sense upcoming attacks. This helps to neutralize them in advance and reduce the intensity to nothing.
Causes of angina pectoris
One of the main reasons for the development of angina pectoris is atherosclerosis. There are a number of risk factors under the influence of which the disease not only begins, but also progresses.
Unavoidable factors for exertional angina are genetic predisposition, the person’s gender and age. Until approximately 50-55 years of age, men are more susceptible to angina pectoris. After menopause in women, that is, after 50 years, the percentage of patients of different sexes equalizes.
Avoidable risk factors:
- Smoking.
- Physical inactivity.
- Diabetes. The disease cannot be completely defeated, but following the doctor’s recommendations reduces its severity and, accordingly, reduces the likelihood of changes in the blood vessels.
- Arterial hypertension. Just like with diabetes, controlling the course of the disease reduces the risk of complications.
- Obesity.
- Psycho-emotional stress.
- High cholesterol levels.
Stable angina pectoris: assessment of prognosis and treatment
The most commonly diagnosed form of coronary artery disease is stable angina. Stable angina is a clinical syndrome characterized by chest discomfort that occurs during physical exertion or emotional stress. The attack occurs at the same level of load and passes within 1–5 minutes. after its termination.
Patients with stable angina are considered to have a relatively good prognosis. In clinical trials of antianginal and prophylactic therapy and/or revascularization, the annual mortality rate is 1.2–2.4% per year [1–6], with an annual rate of cardiac death of 0.6–1.4% and nonfatal myocardial infarction (MI) between 0.6% in the RITA-2 (Second Randomized Intervention Treatment of Angina) trial [4] and 2.7% in the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial [1].
However, the individual prognosis of a particular patient with stable angina can vary significantly depending on his basic clinical, functional and anatomical characteristics.
This is illustrated by data from the REACH (Reduction of Atherothrombosis for Continued Health) registry [7]: in high-risk patients with peripheral arterial disease, post-infarction cardiosclerosis, and diabetes mellitus (DM), the annual mortality rate was 3.8%, while in low-risk patients it was 3.8%. 0.63%.
Prognostic assessment is an important part of the diagnosis of stable angina. On the one hand, there is a need to identify patients with more severe forms of disease whose outcome may be improved by more aggressive management, including revascularization. On the other hand, it is also important to identify patients with less severe disease and good prognosis, thereby avoiding unnecessary aggressive tests and revascularization procedures.
The forecast is determined by several factors:
1. coronary reserve, i.e. the possibility of an adequate increase in coronary blood flow with increasing work of the left ventricle and the amount of myocardium receiving insufficient blood supply. Under conditions of energy starvation, the contractility of the myocardium can be significantly reduced, leading to heart failure with ischemia of a large part of the left ventricle or not very large, but which is sufficient to reduce the pumping function, exacerbating existing contractility disorders due to previous myocardial damage.
2. risk factors that accelerate the progression of atherosclerosis and the formation of unstable plaques, responsible for the development of unstable angina and acute coronary events caused by sudden rupture of atheromatous plaque and not related to the severity of pre-existing stenosis.
According to the 2013 ESC guidelines for the diagnosis and treatment of stable angina, once a diagnosis of stable CAD has been made and optimal medical therapy (OMT) has been initiated, coronary risk stratification is performed, usually based on available non-invasive tests, to select patients who may benefit from revascularization. Depending on the severity of symptoms, early coronary angiography may be performed with appropriate confirmation of the significance of stenoses and subsequent revascularization, bypassing noninvasive testing. Revascularization provides a clear prognostic benefit only to high-risk patients and little or no improvement in prognosis in those who already have a good prognosis.
Previously, in the ESC recommendations [8], an annual risk of cardiac death of more than 2% was considered the threshold beyond which revascularization was recommended. The 2013 guidelines [9] reassessed the severity of angina pectoris, in which surgical treatment improves the prognosis to a greater extent than medical treatment, and suggested that high-risk patients be considered those with a probability of cardiac death > 3% per year.
Additional studies have shown that both ischemia- and anatomically-based indices lead to similar conclusions in identifying patients at “high risk of excesses” with medical treatment alone in whom revascularization procedures lead to an improved prognosis.
There are several approaches to noninvasively assess the prognosis of patients with probable or established CAD, the most widely used of which is the scoring proposed by DB Mark et al., called the Duke tredmil score (Table 1). The authors analyzed the outcomes of 2842 individuals with probable or previously established coronary artery disease who underwent a treadmill test before diagnostic coronary angiography. Points are calculated as follows:
Duke treadmill index = exercise time in minutes – 5 × ST deviation in mm – 4 × angina index (angina index: 0 – there was no angina, 1 – angina appeared, 2 – angina was the reason for stopping the test).
An approximate assessment of the risk of developing myocardial infarction and death using the Duke treadmill index (Table 2) helps to choose further tactics for patient management:
- For patients at low risk, subsequent stress imaging and coronary angiography are considered inappropriate and drug treatment is recommended;
- Revascularization is indicated for high-risk patients;
- For patients with average risk, it is advisable to undergo stress imaging techniques (Table 2), while normal or close to normal myocardial perfusion during exercise in combination with normal heart sizes is considered a sign of a favorable prognosis and drug treatment is recommended for these patients, and in the presence of left ventricular dysfunction – revascularization [10, 11].
The EOC recommendations propose some changes in the tactics of drug treatment of stable angina:
- It is recommended to begin the prevention of attacks with the prescription of b-blockers and/or calcium channel blockers;
- as second-line drugs, it is recommended to add long-acting nitrates, ivabradine, nicorandil or ranolazine, in accordance with heart rate, blood pressure and drug tolerance;
- Trimetazidine may also be considered as a second-stage treatment;
- depending on comorbidity/tolerance in certain patients, second-line drugs may be used as first-line drugs;
- in asymptomatic patients with a large ischemic area (>10%), the use of b-blockers should be considered first.
β-blockers (BABs) are effective antianginal agents that eliminate symptoms, increase exercise tolerance and reduce the consumption of short-acting nitrates [12]. They reduce the need for oxygen by reducing heart rate, blood pressure and myocardial contractility. Perfusion of ischemic areas is improved by prolonging diastole (i.e., perfusion time) and eliminating coronary steal due to increased vascular resistance in non-ischemic areas.
Commonly used β1-blockers that have proven high antianginal effectiveness are metoprolol, atenolol and bisoprolol. To achieve a round-the-clock antianginal effect, β1-blockers with a long period of circulation in plasma (for example, bisoprolol) or dosage forms that maintain the concentration of the drug in plasma (for example, metoprolol CR) are prescribed. To maintain a uniform plasma concentration of atenolol (half-life 6–9 hours), twice daily dosing is optimal, but it should be borne in mind that as the dose of the drug increases, the duration of the β-blocking effect also increases. The effect of beta blockers in stable angina can be counted on only if their use achieves a clear effect of beta-adrenergic receptor blockade. To do this, it is necessary to maintain a resting heart rate within the range of 55–60 beats/min. More accurately, the degree of blockade of β-adrenergic receptors achieved can be assessed by exercise testing [8].
A meta-analysis examining the effect of various beta blockers on mortality showed a significant reduction in mortality with long-term use after myocardial infarction. Based on these data, it was suggested that beta blockers may also have a cardioprotective effect in patients with stable coronary disease. However, this was not proven in a placebo-controlled trial [13].
Large studies of the effectiveness of beta blockers for stable angina - APIS [14] and TIBET [15] - did not show a significant difference in results between patients treated with beta blockers or calcium channel blockers, nifedipine or verapamil. These studies confirmed the beneficial antianginal properties of β-blockers, but did not answer whether treatment changes the prognosis of patients with stable angina.
The recommendations of the European Society of Cardiology recommend beta blockers (if there are no contraindications) as a first-line treatment for stable angina [8, 9].
Calcium channel blockers (CCBs) are a heterogeneous class of drugs that dilate coronary and other arteries by blocking the influx of calcium through L-type channels. The antianginal effect of CCBs is associated with a decrease in cardiac function due to systemic vasodilation, as well as coronary vasodilation and counteracting vasospasm [12].
When comparing the antianginal efficacy of verapamil and metoprolol in stable angina, similar results were obtained [14]. Their comparison in patients with arterial hypertension (AH) and coronary artery disease showed that those receiving verapamil had a lower incidence of new cases of diabetes, angina attacks [16] and mental depression [17].
Non-selective or pulse-lowering CCBs (verapamil and diltiazem) reduce myocardial contractility and atrioventricular conduction to some extent. Even the vasoselective dihydropyridine CCBs (nifedipine, amlodipine, and felodipine) can cause some cardiac depression, but this is counteracted by reflexogenic sympathetic activation of the heart with a slight increase in heart rate that subsides over time.
Long-acting CCBs (eg, amlodipine) or sustained-release forms of short-acting CCBs (nifedipine, felodipine, verapamil, and diltiazem) are preferred to minimize fluctuations in plasma concentrations and cardiovascular effects.
The ACTION trial, a large placebo-controlled trial of long-acting nifedipine for stable angina, demonstrated its safety and ability to reduce the need for coronary angiography and cardiovascular interventions [18].
In the CAMELOT study in patients with coronary artery disease and normal blood pressure, a comparison of amlodipine with placebo revealed a significant reduction in the incidence of hospitalization due to angina, as well as the need for coronary revascularization during 2 years of follow-up [19].
In the CAPE trial [20], treatment with amlodipine compared with placebo resulted in a modest but significantly greater reduction in ischemia on Holter monitoring after 7 weeks. treatment. Patients reported a greater reduction in anginal attacks (70 vs. 44%) and a greater reduction in nitroglycerin consumption (67 vs. 22%) over 10 weeks. treatment with amlodipine compared with placebo. The side effect profile of amlodipine was favorable in both CAMELOT and CAPE.
Some researchers report a more effective reduction in the severity of exercise-induced ischemia during therapy with amlodipine than with the β-blocker atenolol, and an increase in the anti-ischemic effect when used in combination [21].
Nitrates are the oldest of all antianginal drugs, used in clinical practice for more than 100 years. They reduce myocardial oxygen demand through systemic dilation of veins and arteries, which reduces pre- and afterload of the left ventricle and thus reduces myocardial work. Nitrates also act directly on the coronary circulation.
EDRF (or NO) is an important vasodilator produced by the endothelium. Nitrates are metabolized to NO in endothelial cells, and they supply NO directly to vascular smooth muscle cells. Despite the impairment of endothelium-dependent vasodilation in coronary artery disease, nitrates are effective in atherosclerotic coronary arteries and increase blood flow to ischemic areas of the myocardium.
Almost all patients with angina require short-acting nitrates. Nitroglycerin tablets (0.5–1 mg) are usually used for sublingual administration. Aerosol forms of nitrates (nitroglycerin and isosorbide dinitrate) have a good stopping effect. The solution is sprayed into the mouth. The antianginal effect occurs faster than when taking tablets under the tongue. Isosorbide dinitrate has a longer action (up to 90 minutes) than nitroglycerin (up to 15 minutes). These same drugs can be used to prevent angina pectoris during expected short-term physical or emotional stress. The development of tolerance is not a problem for short-acting nitrates [22].
In the 2013 ESC recommendations, long-acting nitrates are classified as second-line antianginal drugs [9].
The most widely used long-acting oral nitrates contain either isosorbide dinitrate (ISDN) or isosorbide-5-mononitrate (ISMN), the main active metabolite of ISDN.
Dosage forms of ISDN can be in the form of regular tablets with natural release of the drug and tablets with delayed release, providing approximately 30% longer duration of action. The minimum effective single dose of ISDN when taken orally is 20 mg. Treatment is usually started with this dose. If the therapeutic effect is insufficient, it is advisable to increase the single dose of ISDN to 30–40 and even 60 mg [23].
It is well known that patients can respond differently to equal doses of the same drug. However, individual sensitivity is ignored, and drugs are usually prescribed routinely - 1 tablet 3-4 times a day. To determine the possibility of increasing the dose of nitrates in a particular patient, it is recommended to measure the initial systolic blood pressure, give the drug and repeat the measurement at the peak of the hemodynamic effect of the drug (usually after 1–2 hours). If systolic blood pressure decreases by 15–20 mmHg. Art., then a further increase in a single dose usually does not provide a significant increase in the antianginal effect, and the likelihood of side effects becomes high [24]. The frequency of taking the drug is determined by the duration of its action and the duration of the time interval during which it is necessary to ensure an increase in stress tolerance. With an increase in the dose of ISDN, there is an increase not only in the severity, but also in the duration of the antianginal effect. The antianginal effect after a single dose of 20 mg of ISDN is 5 hours, 40 mg – 6–7 hours, 60 mg – 8–9 hours.
Isosorbide-5-mononitrate, contained in a tablet with natural release of the drug (20 mg and 40 mg), after oral administration, is quickly and completely absorbed from the gastrointestinal tract. The maximum concentration of the drug in the blood plasma is achieved 1 hour after administration. The duration of the antianginal effect - up to 8 hours - is ensured by the properties of the active substance itself.
Slow-release tablets and capsules, usually containing 50 mg of isosorbide-5-mononitrate, provide a two-phase release of the drug into the bloodstream: 30% of the dose is released quickly, and 70% is released gradually, ensuring long-term maintenance of therapeutic concentrations of the drug in the blood. In terms of antianginal effectiveness, these drugs are the same as naturally released forms containing 20 mg of isosorbide-5-mononitrate, and the duration of the antianginal effect increases to 16–24 hours [23, 24].
All long-acting preparations of isosorbide dinitrate and isosorbide-5-mononitrate are equally effective when used in equivalent doses.
The prophylactic use of nitrates in adequate doses significantly improves the quality of life in patients with significantly limited exercise tolerance due to angina pectoris. It is these patients who most highly rate the benefits of using the drug. Correct determination of indications for prescribing nitrates and selection of a sufficiently effective dose ensure high effectiveness of treatment. The duration of action of nitrates should correspond to the needs of a particular patient, i.e., the time of physical activity that can cause an attack of angina. Patients taking long-acting nitrates should have a daily nitrate-free interval to avoid the potential development of tolerance and to maintain their therapeutic effectiveness over long-term use [8, 9].
Molsidomin. This NO group donor has the same anti-ischemic effect as isosorbide dinitrate [25]. Taking a prolonged form containing 16 mg of the drug is as effective as taking 8 mg 2 times a day.
Ivabradine. Ivabradine selectively and specifically inhibits sinus node If channels, which control spontaneous diastolic depolarization in the sinus node and regulate heart rate. It does not affect the timing of impulses along the intraatrial, atrioventricular and intraventricular pathways, the processes of ventricular repolarization, as well as myocardial contractility. Dose-dependently reduces heart rate, which reduces the risk of developing severe bradycardia (heart rate less than 40 beats/min). Reduces myocardial oxygen demand without affecting its contractility and blood pressure levels [26]. Approved by the European Medicines Agency (EMA) for the treatment of stable angina in patients intolerant of beta-blockers or when their effectiveness is insufficient, when the heart rate in sinus rhythm exceeds 60 beats/min. [26].
Ivabradine is as effective for stable exertional angina as atenolol or amlodipine. Adding 7.5 mg of ivabradine 2 times a day to atenolol therapy allows for significantly better control of heart rate and the severity of angina [26, 27]. A study of the antianginal efficacy of ivabradine - BEAUTIFUL, which included 1507 patients, showed a reduction in cardiovascular mortality and the frequency of hospitalizations due to the development of myocardial infarction or heart failure. The effect was most pronounced in patients with heart rate ≥70 beats/min.
Nicorandil. Nicorandil opens ATP-dependent potassium channels of smooth muscle cells of the vascular wall, which is accompanied by dilatation of small vascular branches. The released nitric oxide causes the large coronary vessels to dilate. The hemodynamic effect of nicorandil occurs within 1–2 minutes. after intravenous administration of the drug and 30–60 minutes later. – after oral administration, persisting for 12 hours (at a dosage of 40–60 mg). Oral nicorandil is recommended for all types of angina. In reducing the symptoms of angina pectoris, increasing exercise tolerance and improving the quality of life of patients, oral nicorandil is comparable to β-blockers, nitrates and calcium antagonists. In a prospective study of nicorandil in stable angina (IONA) over 1.6 years in 5126 patients, a 14% reduction in the incidence of cardiovascular events was noted [28]. The safety profile of nicorandil turned out to be higher than that of the drugs of the mentioned groups (no effect on blood pressure, heart rate).
According to the updated NICE Guidelines for the treatment of stable angina 2011 (National Institute for Health and Clinical Excellence, UK), nicorandil is recommended for use as monotherapy in cases of intolerance to β-blockers and calcium antagonists, the presence of contraindications to their use, or as an additional drug for their lack of effectiveness.
Ranolazine. Ranolazine is a selective late sodium channel inhibitor that reduces disturbances in ventricular repolarization and contractility associated with myocardial ischemia. Doses of 500–2000 mg/day reduce the severity of angina and increase exercise tolerance without changing heart rate or blood pressure. Administration of ranolazine to patients with stable angina in doses of 400 mg 3 times a day had an anti-ischemic effect comparable to the effect of atenolol in a daily dose of 100 mg [29, 30].
The EMA approved the use of ranolazine in 2009 as an additional treatment for stable angina in patients with inadequate control or intolerance to first-line drugs (β-blockers and/or calcium antagonists) [31].
The TERISA study showed a reduction in the frequency of angina attacks when treated with ranolazine in 949 patients with diabetes who were already receiving one or two antianginal drugs. The effect was more pronounced in patients with higher levels of glycated hemoglobin (HbA1c). These results allow us to recommend supplementing insufficiently effective antianginal therapy with this drug, especially in patients with high HbA1c levels [32].
The level of ranolazine in the blood plasma increases with simultaneous administration of cytochrome P3A (CYP3A) blockers, such as diltiazem, verapamil, macrolide antibiotics, grapefruit juice. The clearance of ranolazine is reduced with impaired renal and hepatic function [29]. Ranolazine increases QT length, so caution is required when used in patients with QT prolongation or when used with other drugs known to cause QT prolongation [29].
Trimetazidine. Trimetazidine is an anti-ischemic metabolic modulator [33] with antianginal efficacy at a dose of 20 mg 3 times/day, similar to propranolol. Heart rate and double product at rest and peak exercise remained unchanged in the trimetazidine group, thus showing a non-mechanical anti-ischemic effect [34, 35]. The combined use of trimetazidine at a dose of 35 mg 2 times a day with a β-blocker (atenolol) reduced the severity of exercise-induced myocardial ischemia compared to taking atenolol alone [36].
In patients with diabetes, trimetazidine reduces the level of glycemia and HbA1c [37]. Trimetazidine is contraindicated in Parkinson's disease and movement disorders: tremor (shaking), muscle rigidity, walking disorders and restless legs syndrome. Trimetazidine has not yet been evaluated in large studies in patients with stable angina.
The optimal treatment option includes at least one drug to eliminate angina/ischemia plus drugs to prevent coronary events.
In order to reduce the risk of developing coronary events and progression of atherosclerosis, it is recommended to prescribe:
- Low-dose acetylsalicylic acid (ASA) for daily use in all patients with stable angina.
- Clopidogrel is indicated as an alternative in case of ASA intolerance.
- Statins for all patients with stable angina. The goal of treatment is to achieve an LDL-C level <1.8 mmol/L and/or a 50% reduction if the target level cannot be achieved.
- Prescribing ACE inhibitors (or ARBs) if there is heart failure, hypertension or diabetes.
ACE inhibitors (ACEIs) reduce overall mortality, MI, and stroke in patients with heart failure, vascular disease alone, or at high risk of diabetes. Therefore, it is reasonable to consider the use of ACE inhibitors for the treatment of patients with stable angina, especially those with concomitant hypertension, FI ≤40%, diabetes or chronic kidney disease (CKD), unless contraindicated.
However, not all clinical trials have shown that ACEIs reduce mortality, nonfatal myocardial infarction, stroke, and heart failure in patients with atherosclerosis and intact LV function.
Treatment with angiotensin receptor antagonists (ARBs) may be an alternative therapy for patients with stable angina when ACE inhibitors are indicated but not tolerated. However, there are no clinical trial results showing a beneficial effect of ARB in stable angina.
Aldosterone blockade with spironolactone or eplerenone is recommended for use in post-myocardial infarction patients without significant renal impairment or hyperkalemia who are already on a therapeutic dose of an ACE inhibitor and beta-blocker, have an FI ≤40%, diabetes, or heart failure.
Thus, a doctor’s recommendations to a patient with coronary artery disease with stable angina should be based on the following points:
- Smoking cessation, daily exercise training, antiplatelet agents, and treatment of dyslipidemia and high blood pressure are the main interventions aimed at reducing the incidence of death and myocardial infarction and are indicated for most patients with stable angina.
- Short-acting nitrate therapy should be prescribed to all patients for immediate relief of acute symptoms.
- If angina pectoris, limiting the tolerance of habitual exercise, worsens the quality of life, it is necessary to prescribe systematic antianginal therapy. β-blockers and calcium channel antagonists remain the mainstays of pharmacological treatment of chronic stable angina. Both classes of antianginal agents are effective in preventing angina, and studies have not shown benefit over either one.
- Second-line drugs can be used as additional to the main therapy or as its replacement when the main drugs cannot be used.
- Treatment should begin with monotherapy, resorting to a combination of drugs only in the absence of the required effect. The dosage of one drug should be optimized before adding another.
- Patients whose symptoms are not well controlled with two antianginal drugs should be evaluated as candidates for revascularization, if available.
When determining indications for surgical treatment, patients should be subdivided according to their risk of MI and death. Patients with a risk of cardiovascular death of more than 3% per year are classified as high risk; the risk of cardiovascular death of less than 1% per year is considered low and 1–3% is considered intermediate.
Revascularization provides a clear prognostic benefit only in high-risk subgroups, with little or no improvement in prognosis in those who already have a good prognosis [38].
Literature
- 1. Boden WE, O'Rourke RA, Teo KK, Hartigan PM et al. Optimal medical therapy with or without PCI for stable coronary disease // N. Eng. J. Med. 2007. Vol. 356. P.1503–1516.
- 2. Chung SC, Hlatky MA, Faxon D, Ramanathan K et al. The effect of age on clinical outcomes and health status BARI 2D (Bypass Angioplasty Revascularization Investigation in Type 2 Diabetes) // J. Am. Coll. Cardiol. 2011. Vol. 58. P. 810–819.
- 3. Frye RL, August P., Brooks MM, Hardison RM et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease // N. Eng. J. Med. 2009. Vol. 360. P. 2503–2515.
- 4. Henderson RA, Pocock SJ, Clayton TC, Knight R. et al. Seven-year outcome in the RITA-2 trial: coronary angioplasty versus medical therapy // J. Am. Coll. Cardiol. 2003. Vol. 42. P. 1161–1170.
- 5. Poole-Wilson PA, Lubsen J, Kirwan BA, van Dalen FJ et al. Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with stable angina requiring treatment (ACTION trial): randomized controlled trial // Lancet. 2004. Vol. 364. P. 849–857.
- 6. Steg PG, Greenlaw N, Tardif JC, Tendera M et al. Women and men with stable coronary artery disease have similar clinical outcomes: insights from the international prospective CLARIFY registry // Eur. Heart J. 2012. Vol. 33. P. 2831–2840.
- 7. Steg PG, Bhatt DL, Wilson PW, D'Agostino R. Sr. et al. One-year cardiovascular event rates in outpatients with atherothrombosis // JAMA. 2007. Vol. 297. P. 1197–1206.
- 8. Guidelines on the management of stable angina pectoris: executive summary // Eur. Heart J. 2006. Vol. 27, No. 11. P.1341–1373.
- 9. 2013 ESC guidelines on the management of stable coronary artery disease. https://www.escardio. org/guidelines-surveys/esc-guidelines/Pages/GuidelinesList.
- 10. Ong P., Athanasiadis A., Borgulya G. et al. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study (Abnormal Coronary Vasomotion in patients with stable angina and unobstructed coronary arteries) // J. Am. Coll. Cardiol. 2012. Vol. 59. P. 655–662.
- 11. Kitta Y., Obata J.E., Nakamura T., Hirano M. et al. Persistent impairment of endothelial vasomotor function has a negative impact on outcome in patients with coronary artery disease // J. Am. Coll. Cardiol. 2009. Vol. 53. P. 323–330.
- 12. Thadani U. Selection of optimal therapy for chronic stable angina // Curr. Treat. Options Cardiovasc. Med. 2006. Vol. 8(1). P. 23–35.
- 13. Yusuf S., Wittes J., Friedman L. Overview of results of randomized clinical trials in heart disease. I. Treatments following myocardial infarction // JAMA. 1988. Vol. 260. P. 2088–2093.
- 14. Rehnqvist N., Hjemdahl P., Billing E. et al. Effects of metoprolol vs verapamil in patients with stable angina pectoris. The Agina Pectoris Study in Stockholm (APIS) // Eur. Heart J. 1996. Vol. 17. P. 76–81
- 15. Dargie HJ, Ford I., Fox KM Total Ischemic Burden European Trial (TIBET). Effects of ischemia and treatment with atenolol, nifedipine SR and their combination on outcome in patients with chronic stable angina. The TIBET Study Group // Eur. Heart J. 1996. Vol. 17. P. 104–112.
- 16. Pepine CJ, Handberg EM, Cooper-DeHoff RM et al. A calcium antagonist vs a noncalcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial // JAMA. 2003. Vol. 290. P. 2805–2816.
- 17. Ried LD, Tueth MJ, Handberg E. et al. A Study of Antihypertensive Drugs and Depressive Symptoms (SADD-Sx) in patients treated with a calcium antagonist versus an atenolol hypertension Treatment Strategy in the International Verapamil SR-Trandolapril Study (INVEST) // Psychosom. Med. 2005. Vol. 67. P. 398–406.
- 18. Poole-Wilson PA, Lubsen J, Kirwan BA, van Dalen FJ et al. Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with stable angina requiring treatment (ACTION trial): randomized controlled trial // Lancet. 2004. Vol. 364. P. 849–857.
- 19. Nissen SE, Tuzcu EM, Libby P, Thompson PD et al. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT study: a randomized controlled trial // JAMA. 2004. Vol. 292. P. 2217–2225.
- 20. Deanfield JE, Detry JM, Lihtlen PR et al. Amlodipine reduces transient myocardial ishemia in patients with coronary artery disease: doubl-blind Circadian Anti-Ishemia Program in Europe (CAPE Trial) // J.Am. Coll. Cardiol. 1994. Vol. 24. P. 1460–1467.
- 21. Haasenritter J., Bosner S., Vaucher P., Herzig L. et al. Ruling out coronary heart disease in primary care: external validation of a clinical prediction rule // Br. J.Gen. Pract. 2012. Vol. 62. P. e415–e421.
- 22. Henderson RA, O'Flynn N. Management of stable angina: summary of NICE guidance // Heart. 2012. Vol. 98. P. 500–507.
- 23. Kirichenko A.A. Stable angina and acute coronary syndrome. M., 2001.
- 24. Martsevich S.Yu. The role of nitrates in modern therapy of coronary heart disease // Russian Medical Journal. 2002. No. 21. T. 10. P. 955–957.
- 25. Wagner F., Gohlke-Barwolf C., Trenk D. et al. Differences in the antiischaemic effects of molsidomine and isosorbide dinitrate (ISDN) during acute and short-term administration in stable angina pectoris // Eur. Heart J. 1991. Vol.12. P. 994–999.
- 26. Tardif JC, Ford I, Tendera M et al. Efficacy of ivabradine, a new selective I(f) inhibitor, compared with atenolol in patients with chronic stable angina // Eur. Heart J. 2005. Vol. 26. P. 2529–2536.
- 27. Tardif JC, Ponikowski P., Kahan T. Efficacy of the I(f) current inhibitor ivabradine in patients with chronic stable angina receiving beta-blocker therapy: a 4-month, randomized, placebo-controlled trial // Eur. Heart J. 2009. Vol. 30. P. 540–548.
- 28. Effect of nicorandil on coronary events in patients with stable angina: the Impact Of Nicorandil in Angina (IONA) randomized trial // Lancet. 2002. Vol. 359. P. 1269–1275.
- 29. Jerling M. Clinical pharmacokinetics of ranolazine // Clin. Pharmacokinet. 2006. Vol. 45. P. 469–491.
- 30. Timmis AD, Chaitman BR, Crager M. Effects of ranolazine on exercise tolerance andHbA1c in patients with chronic angina and diabetes // Eur. Heart J. 2006. Vol. 27. P. 42–48.
- 31. Ranexa (Ranolazine). https://www.ema.europa.eu/docs/en_GB/document_ library/EPAR_-_Summary_for_the_public/human/000805/WC500045940. pdf (23 August 2013).
- 32. Kosiborod M, Arnold SV, Spertus JA, McGuire DK et al. Evaluation of Ranolazine in Patients with Type 2 Diabetes Mellitus and Chronic Stable Angina. Results from the TERISA randomized clinical trial // J. Am. Coll. Cardiol. 2013. Vol. 61(20). P. 2038–2045.
- 33. Tuunanen H., Engblom E., Naum A., Nagren K. et al. Trimetazidine, a metabolic modulator, has cardiac and extracardiac benefits in idiopathic dilated cardiomyopathy // Circulation. 2008. Vol. 118. P. 1250–1258.
- 34. Detry JM, Sellier P, Pennaforte S et al. Trimetazidine: a new concept in the treatment of angina. Comparison with propranolol in patients with stable angina. Trimetazidine European Multicenter Study Group // Br. J. Clin. Pharmacol. 1994. Vol. 37. P. 279–288.
- 35. El-Kady T., El-Sabban K., Gabaly M. et al. Effects of trimetazidine on myocardial perfusion and the contractile response of chronically dysfunctional myocardium in ischemic cardiomyopathy: a 24-month study // Am. J. Cardiovasc. Drugs. 2005. Vol. 5. P. 271–278.
- 36. Questions and answers on the review of medicines containing trimetazidine (20 mg tablets, 35 mg modified release tablet and 20 mg/ml oral solution). .https://www. ema.europa.eu/docs/en_GB/document_library/Referrals_document/Trimetazidine_31/WC500129195.pdf (9 March 2012).
- 37. Fragasso G., Piatti Md PM, Monti L. et al. Short- and long-term beneficial effects of trimetazidine in patients with diabetes and ischemic cardiomyopathy // Am. Heart J. 2003. Vol. 146. P. e18.
- 38. Demosthenes G., Katritsis John PA Ioannidis, MD Percutaneous Coronary Intervention Versus Conservative Therapy in Nonacute Coronary Artery Disease. A Meta-Analysis.//Circulation. 2005. Vol. lll. P. 2906–2912.
Signs of exertional angina
The degree of angina pectoris determines the clinical picture of the disease. But the main manifestation for all stages of the disease is an attack of pain. Typical course of a pain attack:
- The pain begins during physical work, at a time of stress. It is typical for an attack to occur in cold or windy weather.
- The pain is most often concentrated behind the sternum with irradiation to the scapula, neck, and lower jaw. Patients describe the pain as squeezing, burning, cutting.
- The duration of pain is from 2 to 15 minutes. With a prolonged attack, the possibility of developing a heart attack cannot be ruled out.
- The intensity of the attack decreases after taking nitroglycerin and when physical work stops.
Symptoms of angina pectoris include weakness, shortness of breath, interruptions in heart function, a decrease or increase in blood pressure, and cold sweat. Some patients experience pale skin, increased urination, and dry mouth.
Attacks can recur from several times a day to two or three episodes a month. Unstable angina pectoris manifests itself more clearly, its symptoms intensify over time.
Predictions and prevention
The consequences of primary angina pectoris are unpredictable, and in the case of stable angina, it can be myocardial infarction, multi-vessel damage to the coronary arteries, cardiosclerosis, persistent narrowing of the main trunk of the coronary artery. Three percent of patients experience death.
The main methods of prevention:
- weight loss;
- to give up smoking;
- balanced diet;
- relief from arterial hypertension;
- preventive use of prescribed medications.
People suffering from exertional angina should definitely contact a cardiac surgeon, who will decide on the need for surgical intervention.
Treatment of angina pectoris
The patient's treatment plan is drawn up individually. First of all, standard therapy for coronary artery disease is prescribed using beta-blockers, antiplatelet agents, and drugs that reduce blood cholesterol.
During an attack, nitroglycerin helps relieve pain. For frequent episodes of exacerbation, prolonged (long-term) action nitrates are prescribed - Isosorbide mononitrate, Isosorbide dinitrate, nitroglycerin ointment or patch.
Complex therapy includes the elimination of all risk factors for the disease, diet therapy, and the choice of optimal physical activity.
Why does angina pectoris FC 3 develop?
The main reason for the progression of cardiac diseases associated with a lack of oxygen in the myocardium is atherosclerotic plaques that appear due to elevated cholesterol levels in the blood. They clog blood vessels, preventing blood from circulating normally. Several factors can provoke atherosclerosis:
- Increased blood pressure - the walls of blood vessels become thinner and more susceptible to damage, which simplifies the formation of plaques;
- Male gender is another risk factor. If women have the hormone estrogen in their blood, which helps eliminate cholesterol, then in men this harmful substance accumulates in the body;
- Poor nutrition is the main reason. Patients whose heart condition requires diagnosis and treatment usually abuse fatty, smoked, and fried foods. They do not watch what they eat, may be overweight, and constantly overeat;
- Cardiovascular diseases are one of the provocateurs of attacks and are often hereditary;
- Insufficient level of physical activity;
- Increased heart rate – when the heart rate increases, the body requires more oxygen. An attack can be triggered by playing sports, emotional shock, and even a regular walk at a slow pace.
However, it is not enough for the patient to remove physical stress - the pain will continue despite the reduction in stress. In the most severe cases, when an attack occurs at rest, and functional class 3 changes to FC 4, surgical intervention is required.