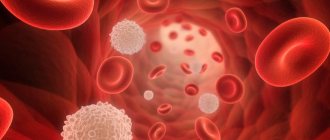
A blood test is the most common and accessible method for general health assessment. Changes in the composition of the blood determine the development of pathology. During the study, such an indicator as the level of neutrophil granulocytes is of great importance. These cells are the largest group of leukocytes that perform an important protective function.
If neutrophils are elevated, most often this means that an inflammatory process is occurring in the body. This condition is called “neutrophilosis”. It should be said that in an adult healthy person, mature cells (segmented cells) predominate in the bloodstream. Their maturation occurs in the bone marrow, after which they enter the blood. If an infectious agent has entered the body or inflammation has developed, then young forms begin to quickly be released from the brain, which include myeloblasts, promyelocytes, metamyelocytes and band cells. As a rule, with an increased content of neutrophil granulocytes, immature cells are found in the blood. In this case, they say that there has been a shift in the leukocyte formula to the left.
An increase in neutrophils in the blood is called neutrophelosis
Functions and types of cells
Neutrophils are a type of leukocyte - white blood cells that are vital to the immune system. These cells are heterogeneous; in total there are 4 types of neutrophils, which differ in their narrow purpose:
- myelocytes are preneutrophils, maximally immature cells without differentiation, which can eventually turn not only into a neutrophil, but into any blood element: from a platelet to an eosinophil;
- young neutrophils are an immature version of neutrophils, a conditional reserve of cells that begin to work in conditions of the body’s increased need for immune cells; in critical situations, a minimum number of such cells can be recorded in the bloodstream (no more than 1%);
- band neutrophils - make up no more than 5% of the total number of neutrophils, this is already a partially specialized cell of the immune system, it works in the bloodstream if the remaining neutrophils cannot cope with their functions;
- segmented neutrophils are the basis of neutrophil cells; up to 70% of the total number of structures constantly work in the bloodstream; they manifest themselves to the maximum during the infectious and inflammatory process in the body.
Thus, there are only two types of active, that is, capable of acting, neutrophils: segmented and band. They solve the main tasks that the body sets for neutrophils:
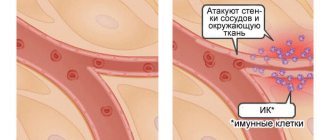
- lyse the cell membrane of the pathogen, killing viruses, bacteria, fungi, and other pathogenic microflora;
- enter into an antigen-antibody reaction with microbes, binding pathogenic flora, accelerating the relief of inflammation;
- absorb microbes and digest them (phagocytosis): one cell can destroy up to 30 “strangers”;
- inactivate viruses, reducing the rate of replication of pathogens, helping to stop inflammation of a viral nature.
Diagnostics
Detection of neutrophilia requires differential diagnosis. To do this, you need to consult a general practitioner. In order to obtain primary information, anamnesis is collected - how long ago the symptoms appeared, whether there was recent contact with infectious patients, whether there was an increase in body temperature, pain, skin rashes.
If there is a suspicion of acute surgical abdominal pathology, the abdomen must be palpated for tension in the muscles of the anterior abdominal wall and the presence of a positive Shchetkin-Blumberg sign. However, it must be taken into account that these signs are difficult to identify in a child under 9 years of age. To confirm the diagnosis, additional examination is prescribed, including:
- Blood tests
. The total number and percentage of all types of leukocytes are calculated. The concentration of red blood cells, platelets, and inflammatory markers (ESR, CRP) is measured. The morphology of granulocytes (toxic granularity, karyopyknosis) is studied. In a septic condition, the level of presepsin and procalcitonin is determined. The presence of autoantibodies (anti-DNA, topoisomerase, antineutrophil antibodies) is checked. - Identification of the pathogen
. To identify the pathogenic microorganism, bacteriological culture, microscopy of sputum, urine, smear from the throat and tonsils are performed. To diagnose helminthiases, a stool test is performed for worm eggs, a blood test for specific immunoglobulins, and a scraping is taken from the child’s perianal folds. - Ultrasound
. A sign of pyelonephritis on an ultrasound of the abdominal cavity is expansion, thickening of the renal collecting system, pancreatitis - enlargement, diffuse changes in the pancreatic parenchyma, cholecystitis - thickening of the walls of the gallbladder, often the presence of stones. - X-ray
. On chest x-rays with pneumonia, foci of infiltration and darkening are visible. When the ulcer is perforated, the images reveal the presence of free gas in the abdominal cavity (“sickle symptom”). In case of inflammatory diseases of the joints, x-rays show a narrowing of the joint space and marginal osteoporosis. - ECG.
Electrocardiography during myocardial infarction reveals ST segment elevation, left bundle branch block, ventricular tachycardia, and other heart rhythm disturbances. With pulmonary embolism leading to pulmonary infarction, signs of overload of the right parts of the heart are detected - a deep Q wave in III, an S wave in lead I, a high pointed P wave (P-pulmonale) in leads II, III, aVF. - Histological studies
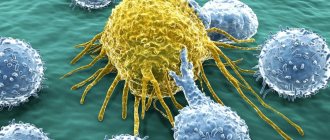
. A definitive diagnosis of cancer can only be made on the basis of a biopsy. The main feature of solid tumors is a large number of atypical cells. In case of leukemia, in the bone marrow biopsy, hyperplasia of the granulocytic lineage and the predominance of blast cells are noted; in the tissues of the lymph node in case of lymphomas, diffuse proliferation of cells with blast morphology is noted.
Norms of neutrophils in the blood in adults and children
Neutrophils are abbreviated Neut and are counted as a percentage or absolute neutrophil count in units per liter of blood. The choice depends on the laboratory in which the analysis is performed. The norms of neutrophils in men, women, and children are presented in the tables.
In women, the variability of indicators is quite high, correlates with age, depends on hormonal fluctuations: puberty (especially delayed), menstruation, pregnancy. The data may decrease slightly depending on the patient’s condition when the test is taken, but never increase.
On average, the norm of neutrophils in the blood of women is up to 60%. This is slightly higher than that of men, which is explained by the physiological and immune characteristics of the female body.
| Woman's age | Norm in % (according to segmented form) |
| Up to 18 and from 45 to 60 | 50-55 |
| Until 21 | 51,5-56,5 |
| Before 35 and after 60 | 52-60 |
| Up to 45 | 50-58,5 |
In men, normal levels of neutrophils in the bloodstream are not significantly lower: up to 57%, and are correlated with the age and condition of the patient when the test was taken.
| Man's age | Norm in % (according to segmented form) |
| Up to 18 and from 35 to 45 | 50-54 |
| Under 21 and over 60 | 50-56 |
| Up to 35 | 51,5-57 |
| 45-60 | 49-53 |
In children, the calculation of the norm of neutrophils in the blood is carried out by day, month, year, since fluctuations are the most variable. A sharp increase in the first days of life is associated with the active formation of immunity and adaptation to the external environment.
| Child's age | Norm in % (according to segmented form) |
| Newborn | 59-60 |
| 12 hours | 65,1-68,1 |
| 1st day | 60,1-61,1 |
| 7 days | 39,9-42,9 |
| 14 days | 39,1-40,5 |
| 30 days | 35,5-38,2 |
| 6 months | 30,1-32,1 |
| 1 year | 30,5-31,5 |
| 2 years | 30,3-33,5 |
| 4 years | 40,1-42,5 |
| 6 years | 49,1-51,1 |
| 8 years | 50,5-53,1 |
| 10 years | 50,1-54,1 |
| 11-18 years old | 52,5-55,5 |
Forecast
It is impossible to predict prognosis based on neutrophilia alone. It all depends on the disease that served as the background for the occurrence of neutrophilia. For example, a transient increase in the number of neutrophils after stress, food intake, or in a child on the first day of life is absolutely benign and transient. Conversely, severe purulent-septic pathologies and oncological diseases have a fairly high incidence of deaths. Therefore, any excess of the reference values of neutrophils (especially high and persistent ones) requires contacting a doctor.
Pathological causes of growth
The norm of neutrophils in the blood changes in most cases due to pathological reasons, the main of which are:
- inflammation of infectious or autoimmune origin;
- endocrine pathologies;
- tumor growth, metastasis;
- physician error during surgery (iatrogenic factor).
There is an exception to the rule: neutrophils can remain normal against the background of a manifest pathological process, which indicates depletion of the immune system and requires immediate adequate treatment.
Reasons for the downgrade
A decrease in the number of neutrophils in the blood compared to the norm is called a shift in the leukocyte formula to the left. There are several reasons for this condition:
- HIV;
- aplastic anemia;
- severe infections;
- the period after a serious illness, prolonged fasting, cachexia;
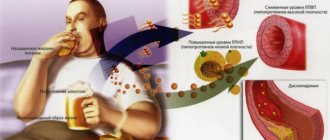
- alcoholism;
- hepatitis;
- sepsis;
- radiation sickness;
- intoxication of various etiologies, taking medications (antibiotics, antiviral anti-inflammatory drugs, drugs for the treatment of hyperthyroidism, for chemotherapy);
- deficiency of minerals, B vitamins;
- bone marrow damage;
- enlarged spleen;
- metastasis of cancer of any location to the bone marrow or myeloproliferative processes;
- genetic predisposition;
- hyperglycemia;
- idiosyncrasy, when the reason for the decrease in the concentration of neutrophils in the bloodstream is unclear.
Correction
Conservative therapy
There are no direct ways to normalize the number of neutrophil granulocytes. To combat neutrophilia, it is necessary to treat the underlying disease against which it developed. Short-term neutrophilia after eating, stress or physical work does not require any intervention, as it is not a sign of disease or pathological condition. Neutrophilia resulting from surgery also does not need to be treated. In the case of persistent neutrophilia, you should consult a doctor to find out the cause and prescribe differentiated treatment:
- Antimicrobial (antiparasitic) therapy
. For bacterial infections, antibiotics (amoxicillin, cefixime) are used. For generalized infections (sepsis, bacterial endocarditis), it is necessary to use a combination of 2 antibacterial drugs. In case of helminthic infestation in a child, anthelmintic drugs (mebendazole) are prescribed. - Hemorheological therapy
. For heart attacks of any location caused by thrombosis or thromboembolism, antiplatelet drugs (acetylsalicylic acid), anticoagulant drugs (low molecular weight, unfractionated heparin), and sometimes thrombolytic drugs (alteplase) are used. - Antisecretory and antienzyme therapy
. In order to reduce the secretion of hydrochloric acid in peptic ulcers, proton pump inhibitors (omeprazole, pantoprazole), H2-blockers (famotidine, ranitidine) are used. To suppress the destructive action of proteolytic enzymes of the pancreas in acute pancreatitis and pancreatic necrosis, enzyme inhibitors (aprotinin) are effective. - Anti-inflammatory treatment
. To achieve remission of rheumatological diseases, medications are prescribed that stop the inflammatory process. These include glucocorticosteroids (prednisolone), 5-aminosalicylic acid derivatives (sulfasalazine), immunosuppressants (cyclophosphamide, methotrexate). - Chemotherapy.
For the treatment of malignant tumors, chemotherapeutic drugs (cytostatics, antimetabolites, hormone antagonists) are used in combination with radiotherapy. For oncohematological diseases, a combination of several antitumor agents is necessary.
Surgery
Many diseases accompanied by neutrophilia (mainly acute abdominal pathologies) require emergency surgical intervention - laparoscopic appendectomy, laparotomy and suturing of the ulcerative defect, cholecystectomy, opening and drainage of the abscess, etc. For myeloproliferative pathologies, in case of ineffectiveness of conservative therapy, they resort to stem cell transplantation cells.
Reasons for the increase in some cells and the decrease in others
An increase or decrease in neutrophil levels in the blood can be correlated with many factors of natural and pathological origin. There are many uniform elements that are called upon to fight “strangers” in this case. There are two options:
- if neutrophils are elevated, and lymphocytes, on the contrary, this is the first phase of the immune reaction, when central immunity is not yet active enough, and there is no need for it: fluctuations are insignificant;
- if neutrophils are reduced, and lymphocytes, on the contrary, this is the second phase of the immune response, when central cells work more actively, and local-level structures reduce their intensity for a short time.
The general rule is one: when neutrophils increase, lymphocytes decrease and vice versa. This is the norm. There is no simultaneous increase or decrease observed.
How to increase neutrophils
It is impossible to buy a medicine that can increase neutrophil levels. However, it is still possible to influence their content in the blood. For example, if a decrease in phagocyte cells occurred while taking sulfonamide antibiotics, it makes sense to review the course of therapy with your doctor and replace the drugs.
In some cases, the production of neutrophils is affected by a pronounced imbalance of nutrients in the body. The most commonly reported levels of vitamin B9, known as folic acid, and B12 are significantly reduced. Therefore, often, if there is a lack of neutrophils, they additionally take an analysis for vitamin deficiency and prescribe a course of group B. 10-14 days after restoring the balance of nutrients in the body, an increase in the number of neutrophils is observed, which is fixed within acceptable values.
Special cases of decreased neutrophils
We are talking about genetically determined neutropenia, which is quite rare, but affects the result of a blood test. This:
- benign chronic neutropenia is asymptomatic, there is no danger to life, but when interpreting the analysis, this point is always taken into account;
- cyclic neutropenia occurs in one person per million, does not affect the quality of life, manifests itself in a periodic causeless decrease and then restoration of neutrophils to normal;
- Kostmann's syndrome is a condition when neutrophils are deprived of the opportunity to mature, as a result a person is deprived of natural protection and constantly suffers from all possible infections. Today, provided that the pathology is detected in a timely manner, patients are given courses of drug correction.
What indicators does the blood test contain?
Donating blood for testing is necessary during planned hospitalization, to assess the effectiveness of the therapy, and during pregnancy. To make an accurate diagnosis and prescribe treatment, the doctor always prescribes a general blood test. Material for research is taken from a finger or from a vein. The second option is preferable, since venous blood more accurately shows the level of hemoglobin and red blood cells.
First of all, red blood cells, white blood cells and platelets are analyzed, as well as:
- Hemoglobin level.
- Erythrocyte indices.
- Hematocrit level.
- Reticulocyte count.
Additionally, the erythrocyte sedimentation rate (ESR), color and blood clotting period are determined.
An extended study involves indicating the leukocyte formula, including the count of eosinophils, lymphocytes, monocytes, band and segmented neutrophils.