The rapid development of reconstructive cardiac surgery and the emergence of modern framed pericardial bioprostheses have made it possible to obtain excellent long-term results in the treatment of heart defects and solve one of the serious problems of reconstructive surgery of the aortic root [1]. Today, to determine the optimal tactics of reconstructive surgery and obtain good results in the immediate and long-term period, the surgeon needs reliable decision-making criteria in favor of installing a frame prosthesis or performing aortic root reconstruction. The absence of such criteria leads to the fact that the surgeon often makes the final decision on the possibility of preserving his own aortic valve (AV) only during surgery, guided by the results of a visual assessment of the degree of degenerative-dystrophic changes in the aortic wall and calcification of the semilunar valves, and not by preoperative geometric characteristics AK [2]. The assessment of the relationship between valve insufficiency and the deviation angles of inter-flap structures by A.K. still remains relevant. It is difficult to overestimate the importance of developing clear recommendations for achieving optimal closure function of the aortic valve and criteria for restoring the correct geometry of the aortic root structures after reconstructive operations. Of clinical importance is the correlation between morphometric characteristics, which can be assessed during intraoperative revision, and geometric parameters obtained before surgery [3]. Obviously, determining the optimal ratio of the linear and angular characteristics of the aortic valve will not only make it possible to decide whether the valve is suitable for reconstruction, but also to establish the intervals of values of the morphometric parameters of the reconstructed aortic root, within which optimal co-optation of the valves will be maintained after surgery [4].
It is known that degenerative changes in the walls of the ascending aorta lead to its dilatation and a decrease in strength characteristics, contribute to the deformation of the aorta with a violation of the closing ability of the semilunar valves [5, 6]. Moreover, the risk of developing such pathological changes increases if the semilunar valve has two valves, which occurs in 1-2% of the population [7]. The presence of a bicuspid aortic valve (BAV) is combined with dilatation of the aortic root and its ascending part, accompanied by cystomedian necrosis, fragmentation of elastic fibers and changes in the orientation of smooth muscle cells in the wall of arterial vessels [5]. There is an opinion that in BAV, the main predictor of the development of aortic insufficiency is an increase in the diameter of the sinuses of the aortic root [8]. Other researchers believe that, in addition, not only an increase in the diameter of the sinus of the aortic root, but also the expansion of the ascending aorta has a great influence on the development of dysfunction of the BAV [9]. In addition, in the presence of BAV, there are disturbances in the properties of the connective tissue, which in any case affect the deformation and strength characteristics of not only the BAV, but also the aortic wall [10].
It is obvious that anatomical and clinical studies of the morphometric parameters of the aortic valve will allow a new look at the problems of reconstructive correction of congenital and acquired diseases of the aortic valves.
The purpose of the work is to conduct a comprehensive morphometric study of the linear and geometric parameters of the aortic valve and determine which changes in parameters are combined with incomplete closure of the semilunar valves of the aortic valve and dilatation of the aortic root.
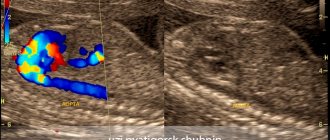
Ultrasound of the aorta in the abdominal cavity
Ultrasound of the abdominal aorta: indications, performance, interpretation of results
Ultrasound is used to diagnose the abdominal aorta. The technique makes it possible to find out about the presence of blood flow disturbances, damage or changes in the walls of the vessel. This procedure is performed with Doppler ultrasound.
Ultrasound of the abdominal aorta: what is it?
During the procedure, the ultrasound doctor will examine the area from the last thoracic vertebra to the sacrum. Standard ultrasound does not make it possible to assess the condition of the vessels in full, so Doppler sonography is used to diagnose the aorta. It is based on the possibility of reflecting ultrasound waves from objects in motion.
During Dopplerography, the branches of the aorta and the aorta itself are painted in different colors, which helps the ultrasound specialist make a conclusion about the state of the blood flow.
In what cases is aorta diagnosed?
The main task of this procedure is to detect the aneurysm. It is characterized by thinning of the vessel wall and the appearance of a sac. This leads to improper blood flow in the vessel. The disease is dangerous due to rupture of the vessel wall and heavy bleeding.
Diagnosis of the abdominal aorta is carried out in the following cases:
- The appearance of throbbing pain in the head;
- The patient has arterial hypertension;
- Severe pain in the abdomen on the left side, spreading to the lower back;
- The patient has memory problems;
- Changing the shape of the abdomen;
- Unreasonable nausea and repeated vomiting;
- The presence of blood in the stool;
- Presence of pulsation in the middle part of the abdomen;
- Decrease or increase in pressure;
- Previously suffered a heart attack or stroke;
- Suspicion of an aneurysm in a smoking patient.
How to properly prepare for the procedure?
If you have been prescribed an ultrasound examination of the abdominal aorta, then you should properly prepare for it. Before such an ultrasound, it is imperative to cleanse the intestines and prevent flatulence. In the absence of preparation, the study may be uninformative, since the object being examined is located behind the intestines, and if it is full, it will be almost impossible to see the artery.
You should start preparing for an ultrasound 3 days before the intended examination. During this time, you should adhere to certain dietary rules and also take certain medications. From the diet you need to completely exclude foods that can cause gas: fermented milk products, legumes/peas, bread (black), cabbage.
If necessary, 2 days before the test, the doctor will recommend medications that improve digestion.
1 day before the ultrasound in the evening, you should cleanse the intestines naturally or with an enema.
The last time you can eat is 8 hours before the ultrasound. You can drink for the last time 2 hours before the test.
Preparation is not carried out only if the patient is admitted to the hospital with complaints of acute pain in the abdominal area. In this case, emergency care may be required, and the preparation time may adversely affect the patient's health.
How is ultrasound of the aorta performed?
Do not be afraid, the examination is completely painless and safe, it is carried out in the same way as a simple ultrasound. During the ultrasound, the patient lies on his back. An ultrasound technician moves an ultrasound probe across the abdomen to diagnose the abdominal aorta. The duration of the procedure is about half an hour.
The patient can watch the procedure on a large screen located opposite the couch. If necessary, the ultrasound doctor asks the necessary questions and comments on what is happening on the screen. Immediately after the study, a conclusion is issued. To prescribe treatment or adjust it, you must contact the attending doctor who referred you for an ultrasound scan.
Diseases that can be detected during ultrasound examination of the abdominal aorta: aortic dissection (which is characterized by a rupture of the walls); aneurysm (depletion of the wall of the abdominal artery will be clearly noticeable); occlusion (impaired vascular patency; a break in blood flow can be seen on the image); atherosclerosis (the appearance of cholesterol plaques, an ultrasound specialist diagnoses them by thickening the artery wall); stenosis (the main branch of the aorta narrows); calcification (formation of calcium salts).
How to decipher the research?
Thanks to Doppler ultrasound, it is possible to obtain information about the exact sizes of blood vessels, identify certain pathologies, determine the possibility of a risk of their occurrence, understand the speed of blood flow and study in detail places with obstructed blood flow.
The abdominal aorta should not be more than 3 centimeters in thickness. With a smaller diameter, there is a high probability of atherosclerosis or stenosis. If the diameter is more than 3 centimeters, an aneurysm is suspected. The ultrasound doctor examines the aorta; the diagnosis is made only by the doctor who prescribed the diagnosis.
If the size of the abdominal aorta exceeds 5 centimeters, surgery will be prescribed to remove the cause of the pathology. Otherwise, it may be dangerous to the patient's life.
The procedure is prescribed for patients predisposed to cardiovascular diseases, as well as for the elderly. By identifying pathology at an early stage of its development and prescribing appropriate treatment, the chances of a speedy recovery increase.
Advanced blood flow pathologies are quite difficult to treat and in most cases require surgery.
Ultrasound of the abdominal aorta in Nizhny Novgorod.
In Nizhny Novgorod, diagnostics of the aorta using ultrasound is carried out at the VIP Academy clinic. The examination is performed on the latest ultrasound machine by a certified specialist.
Cost of ultrasound examination Ultrasound of the abdominal aorta.
The price for an ultrasound of the aorta in a medical clinic is the average city price. The availability of this diagnostic method makes it possible to timely identify and prevent life-threatening diseases. Pathologies of the abdominal aorta are characterized by blood loss, as well as damage to vital organs of the body. It was thanks to timely, high-quality ultrasound diagnostics and the work of surgeons that in many cases patients were able to save their lives.
If a doctor prescribes this procedure, it should not be ignored under any circumstances.
You can sign up for an ultrasound of the abdominal aorta at the VIP Academy clinic through the administrators at: +7 (831) 200-47-38.
MSCT of the aorta at the Innovative Vascular Center
Multislice computed tomography angiography of the abdominal aorta is widely used by doctors at our clinic for preoperative diagnosis of problems with the aorta and its branches. This technology allows you to plan a surgical intervention, select the correct size of stent graft for an aortic aneurysm and an instrument for passing chronic occlusions. We also use MSCT to evaluate postoperative results after stenting or resection of an aortic aneurysm, and the status of vascular reconstructions in the long-term period.
Statistical method. Statistical methods were used to identify and evaluate risk factors for the following prognoses: annual mean aneurysm growth, complication rates (acute dissection and/or rupture), mortality, and long-term survival.
Survival analysis. Five-year survival estimates were calculated by life table analysis (Kaplan-Meier). Differences in survival were tested using the LIFEREG procedure in SAS version 6.07, 1994 (SAS Institute, Inc, Kari NS).
Kaplan-Meier survival plot. Five-year survival estimates are illustrated for patients with thoracic aortic aneurysms (TAAs) versus the general (age- and sex-matched) population (EA).
Results and discussion. Joyce JW et al. [21] reported a 5-year survival rate of 61% for ascending thoracic aortic aneurysms with a diameter of 6 cm or less; aneurysms larger than 6 cm had a five-year survival rate of 38% of cases. Complete five-year survival in our series was observed in 64% of cases. Mortality is expected to be related to the aneurysm in the vast majority of cases, although adequate details for this distinction have often been unavailable. Survival was significantly lower for descending aortic aneurysms (39% at 5 years) (p=0.031). Patients with dissection had lower survival (46% at 5 years).
Growth parameters. The estimated annual growth rate for thoracic aortic aneurysms was 0.29 cm/year. This is in close correlation with the results reported by Dapunt OE et al. [26] (0.32 cm/year). Masuda Y. et al. [27] reported a growth rate for thoracic aortic aneurysms of 0.13 cm/year. Hirose Y. et al. [28] report a high annual growth rate of 0.42 cm/year for thoracic aortic aneurysms. In a subsequent study, however, Hirose Y. et al. [28] gave a significantly lower rate.
The discrepancy between the two studies [28] may well explain the different strategies used to estimate growth. In recent studies by Hirose Y. [28], the regressions used are close to those used by Dapunt OE et al. [26] and in the current study, when assessing the growth of a thoracic aortic aneurysm. Earlier studies by Hirose Y.'s group [28] calculated that height is equal to the difference between the last and first measured size divided by the duration between studies.
Size has traditionally been considered an important risk factor for complications (ie, acute dissection and/or rupture) in patients with thoracic aneurysms, and it has been considered the most important independent factor in the decision to undergo elective surgery. The effect of size on the rate of growth of aneurysms is a matter of debate. Dapunt OE et al. [26] note that more intense dilations were found in those patients whose aortic diameter at diagnosis was >5 cm. On the other hand. Hirose Y. et al. [28] found no significant effect of size on growth rate.
Dapunt OE et al. [26] reported that the presence of hypertension correlates with a large aortic diameter, but does not significantly affect the rate of aortic enlargement growth. Masuda Y. et al. [27] reported a direct relationship between the magnitude of diastolic pressure and the degree of aortic dilatation.
Possibility of complications. It is important to consider the natural history of patients with thoracic aneurysms, e.g. cases of acute dissection and/or rupture in this population. Pressler V., McNamara JJ [22] reported that in eight of nine cases of ruptured descending thoracic aortic aneurysms, the aortic size was greater than 10 cm. Subsequent studies reported complications with much smaller sizes. A study by Gott VL et al [11] of ascending aortic aneurysms in patients with Marfan syndrome reported a mean size of 7.8 cm at the time of dissection.
However, in seven of 26 patients (26.9%), dissections were observed with aneurysms measuring 6.5 cm or smaller. In addition, Crawford ES et al. [9] reported a mean size at rupture of 8.0 cm among 117 patients with descending thoracic and thoracoabdominal aneurysms. Dapunt OB et al. [26] report ruptures of thoracic aneurysms occurring in even smaller sizes, with an average size of 6.1 cm.
These observations indicate dissections or ruptures as aneurysms expand in size. The average size at the time of rupture or dissection was 6.0 cm for ascending aneurysms and 7.2 cm for descending aneurysms. A multivariate retrospective analysis was performed to isolate risk factors for acute dissection or rupture, which showed that a size greater than 6.0 cm increased the likelihood of dissection or rupture by 32.1% for ascending aneurysms (p=0.005). For descending aneurysms, this probability increased by 43% for sizes greater than 7.0 cm (p=0.006). Frist WH et al. [33] provide the following data for ascending and descending aneurysms: 6 cm for the ascending aorta and 7 cm for the descending aorta.
Criteria for surgical intervention.
Below we have attempted to demonstrate the importance of the thoracic size of the aneurysm in dire complications such as aortic rupture and dissection. Our observations attempt to demonstrate a clearly increasing incidence of complications with increasing aortic size. These observations indicate that the average size at rupture and dissection is 6.0 cm for ascending aneurysms and 7.2 cm for descending aneurysms. Multivariate analysis of risk factors affecting acute dissection and/or rupture shows that size greater than 6.0 cm is a significant risk factor (p=0.005). Logistic analysis indicated a 32.1% increase in the likelihood of dissection or rupture for ascending aneurysms with a mean size greater than 6.0 cm (p=0.005) and a 43.0% increase for descending aneurysms greater than 7.0 cm (p=0.006).
These data strongly call for the use of a size criterion for surgical replacement of aneurysmal aorta to prevent complications of rupture and dissection. Additionally, these data suggest that a lower size criterion than previously recommended should be used.
If the average size at the time of complication (in this case: 6.0 cm for the ascending and 7.2 cm for the descending aorta) is used as an intervention criterion, then half of the patients are likely to experience serious complications during the intervention. Accordingly, the authors suggest intervention for slightly below average size criteria at the time of complication. It is suggested that surgical intervention be used for 5.5cm ascending and 6.5cm descending aortic aneurysms. These above criteria allow intervention to occur before the catastrophically increased likelihood of rupture and/or delamination.
These recommendations indicate that elective surgery is much safer than emergency surgery. For ascending aneurysms and aortic arch aneurysms, elective surgery was very safe (mortality rate 4.3%). These mortality results are broadly consistent with those reported by other centers. Although surgery on the descending aorta has a higher risk (19%), the number of patients in this category is relatively smaller to influence the final outcome.
Many of the above data have shown that surgery on the ascending aorta is safer. CPB via left atriofemoral cannulation using a centrifugal pump has been shown to be a safe and reliable method for preventing postoperative complications such as ischemic complications such as renal failure and spinal cord injury. In addition, the advent of a protease inhibitor (aprotinin) led to a significant reduction in blood loss as a result of the protection of platelet wall receptors at the beginning of CPB. The introduction of a collagen-impregnated Dacron graft has led (Hemashield Meadox Medicals Inc, Oakland, NJ) to improve surgical hemostasis, essentially eliminating bleeding through the graft wall. These facts support priority selective intervention to avoid rupture and dissection of aneurysms.
For descending aortic aneurysms, the risk of paraplegia should be considered as a significant intraoperative complication. The risk of paraplegia (spinal origin) in the literature remains between 2 and 20%, in this case it is 4.0%. Obviously, advanced age and concomitant diseases can lead to frequent complications for which surgical intervention is not indicated. Thus, each patient must be assessed individually, and the expected risk of complications (especially paraplegia in descending aortic aneurysms) must be weighed to avoid complications such as rupture and dissection. In addition, the level of doctors in the medical center in question must be taken into account. The size criteria presented here are suggested for less severely ill patients treated at more experienced centers.
Studies of patients with Marfan syndrome.
More than 90% of deaths in Marfan syndrome are due to complications of ascending aortic aneurysms. Because most patients with Marfan syndrome have some degree of aortic regurgitation (aortic root 6.0 cm), Gott, Lima et al recommend prophylactic treatment for aneurysms that reach 5.5 to 6.0 cm. We recommend an intervention criterion of 5.0 cm for patients with Marfan syndrome, other hereditary collagen vascular diseases, or familial cases of aortic regurgitation.
This size criterion is slightly lower than the recommendations for intervention for atherosclerotic aneurysms of the ascending aorta. Experience has shown that in several patients with Marfan syndrome the dissection or rupture occurred at sizes less than 5.0 cm. These young patients were often in severe clinical condition. Thus, prophylactic surgical treatment can significantly improve their clinical condition and prognosis.
Developing intervention criteria is a complex research endeavor. Research into this problem is important to improve patient survival. To determine appropriate size criteria for the intervention, we used statistical analysis. These intervention criteria should take into account the patient's age, physical condition, life expectancy, that is, approach the intervention criteria using statistical methods in terms of preventing complications (dissection and rupture). Organ pressure from the aneurysm, concomitant aortic regurgitation, and acute aortic dissection are widely accepted common indications for surgical intervention regardless of aortic size.
Some points of view are still debated in the surgery of chronic ascending aortic disease: which technique to use in treatment (open or wrap technique, direct or indirect reimplantation of the coronary arteries), how to protect the brain during the restoration of the aortic arch. When the aortic root was included in the surgical plan, implantation of a valved conduit was typically performed using a wrap technique with coronary artery reimplantation and a Dacron graft (8mm). Valve replacement alone does not protect against recurrence of ascending aortic aneurysm, leading to reoperation. However, repeated operations have a high mortality rate.
Some authors have used the wrapper technique. Regarding bleeding, the probability of early reoperation is low - 4.5% in this series and can be compared with the data of Kouchoukos N. (2% - open technique). In the studied patients there was no need for repeated operations for pseudoaneurysms of the ascending aorta.
Coronary reimplantation using a Dacron graft (8mm) appears to be more reliable and technically feasible than direct reimplantation or reimplantation with aortic buttons. Kouchoukos N. [7] Taniguchi K. et al. [12] reported the appearance of pseudoaneurysms in the coronary ostium after these operations [12,13].
It is therefore believed that the use of a Dacron graft prevents these complications (as shown by standard coronary angiography). The resulting right atrial fistulas closed, with the exception of one case where reoperation was required. Nine cases in which a tubular graft was implanted resulted in sudden death of unknown cause (no autopsy was performed). The possibility of false aneurysms or fistulas leading to death was not excluded.
Aortic arch repair is always indicated when the aneurysm extends into the aortic arch, when the dissection extends into the arch, or when the intimal tear is localized to the arch (2 cases in this series). The authors believe that stopping hypothermic CPB leads to neurological complications. Griepp RB et al. reported a rate (5.6%) of neurological complications in 87 patients [15]. The authors prefer stopping hypothermic CPB during selective catheterization of the great vessels of the brain.
30-day mortality was observed in 7.6% of patients and 6% in patients with prosthetics (valve-containing conduits were used). Galloway AC et al. [6] reported similar case fatality rates of 5.3 and 5%, respectively.
Many analyzes also indicate that concomitant coronary artery transplantation and older age are major risk factors, as has been shown by other authors. Survival is poor in patients undergoing surgery for chronic ascending aortic disease: 48% at 12 years in Kouchoukos NT et al. [13] and 57% over 7 years in Culliford AT [34]. In this series, complete survival was 59.6% ± 3.7% over 9 years for all patients and 66.3% ± 4.5% over 9 years for patients with prosthetics with a valve-containing conduit (intraoperative mortality was also included).
The predominant cause of late mortality was not found in this series. Factors that increase risk as shown by univariate analysis are: CPB time, aortic arch repair, chronic aortic dissection, and older age.
Conclusion
Coarctation of the aorta in the fetus. Diagnostic accuracy and errors
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.
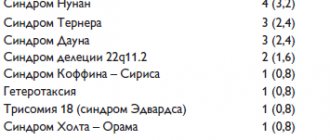
Most congenital heart defects (CHDs) are diseases that threaten the health or life of a newborn. The experience of Russian and foreign colleagues shows that the incidence of congenital heart defects ranges from 10 to 13 cases per 1000 newborns, of which 4:1000 are complex congenital heart defects. In our country, the average frequency of congenital heart disease ranges from 8-9 to 11-13 cases per 1000 live births. Up to 50% of newborns die from cardiac pathology in early infancy.
The distribution of diagnosis of congenital heart disease depending on the nosological form varies significantly. Prenatal diagnostics can detect certain congenital diseases in 90% of cases. Statistics figures inexorably show a low percentage of detection of congenital heart disease (30%) based on the results of a screening study. In specialized institutions, the detection rate of congenital heart disease is higher and reaches 54% [1, 2].
In recent years, the accuracy of ultrasound diagnosis of fetal pathology has been repeatedly criticized by obstetricians-gynecologists and, to a greater extent, pediatricians. Sometimes clinical signs are of much less interest to specialists than the data of an antenatal ultrasound examination of the fetus.
This work presents an analysis of the capabilities of prenatal ultrasound examination for aortic coarctation. The work takes into account the data available in the publications of domestic and foreign authors, as well as material from the functional diagnostics department of the Center.
The Latin term "coarctatius" means "narrowed, compressed." It was first described by JF Meckel in 1750. Coarctation of the aorta is a pathological narrowing of its lumen, which can occur anywhere along its entire length. The frequency of the defect is 6.3%, according to clinical observations from a sample of 2000 cases [3], and 8.4% according to the results of pathological material [4].
In children of the first year of life, coarctation of the aorta ranks fourth among congenital heart diseases. As a rule, it develops distal to the branch of the left subclavian artery near the ductus arteriosus. Depending on the location of the narrowing of the aorta relative to the ductus arteriosus, two classical types of coarctation are distinguished: preductal and postductal [5].
In the presence of narrowing of the aorta, the clinical picture may increase like a flurry after the closure of the ductus arteriosus. During the first year, 56% of patients die. Most deaths are caused by a combination of coarctation with other cardiac anomalies. The isolated form in the first weeks and days of life is also characterized by a high mortality rate (34%). If children survive this period, then life expectancy is on average 30-50 years. The cause of death in newborns is cardiopulmonary failure. In case of high arterial hypertension, as an exception, there may be a cerebral hemorrhage.
At the Federal State Budgetary Institution “Scientific Center for Obstetrics, Gynecology and Perinatology named after. IN AND. Kulakova » Ministry of Social Development of the Russian Federation over a two-year period (2010-2011), 27 children were born with aortic anomalies, from slight narrowing to complete interruption. In 15 observations in the department of functional diagnostics, the diagnosis was made antenatally. These were pregnant women who applied late, from 35 to 39 weeks of gestation. In all cases, aortic pathology was combined with left ventricular hypoplasia. The diagnosis was confirmed in all cases. In isolated form, coarctation of the aorta was diagnosed in 6 cases during this period. In 3 of them, the diagnosis was made antenatally, in 2, the narrowing was detected in newborns on the 3-5th day after closure of the ductus arteriosus. In one case, aortic kinking was diagnosed after birth. Thus, our data indicate the complexity and low percentage of identifying isolated coarctation of the aorta. Only in those observations where there are pronounced hemodynamic disturbances leading to significant anatomical changes in the form of hypoplasia of the left ventricle, disproportion of the ventricles of the heart, an increase in the diameter of the pulmonary artery, the diagnosis can be made antenatally with great certainty.
The first works on the diagnosis of aortic coarctation in the fetus date back to 1984 [6, 7]. According to the literature, transvaginal access at 12-15 weeks of gestation allows diagnosing coarctation of the aorta in 21.4% of cases [1]. With transabdominal access, the frequency of detection of aortic coarctation increases: at 16-30 weeks it is 43%, after 30 weeks, as hemodynamic disorders progress, it does not exceed 54% [8].
According to the results of a screening ultrasound examination of 20,248 fetuses at 19-22 weeks of gestation in a large region of Germany (1990-1994), a prenatal diagnosis of aortic coarctation was not established in any of the 7 cases. Similar data were obtained in Norway, even in a specialized prenatal diagnostic center. According to a multicenter analysis conducted in 12 European countries, an accurate prenatal diagnosis of isolated coarctation of the aorta in the late 90s. was established only in 9 (15.8%) of 57 cases [9]. The average time to detection of isolated coarctation was 22 weeks, with 7 of 9 cases detected before 24 weeks. When coarctation of the aorta was combined with extracardiac defects and chromosomal abnormalities, the accuracy of its prenatal diagnosis was significantly higher due to the severity of hemodynamic disorders and extended echocardiographic examination of the fetus and amounted to 52%.
According to the Institute of Cardiovascular Surgery named after. A.N. Bakulev, diagnostic accuracy does not exceed 27%. As a rule, pathology is most often observed when coarctation of the aorta is combined with other cardiac anomalies [10].
Thus, summarizing the statistical data of the Center’s material, publications of leading Russian specialists and foreign colleagues, we can note a very low percentage of diagnostics of aortic coarctation in the fetus.
What is the reason for such a low percentage of detection of aortic coarctation antenatally?
There are several factors that make it difficult to diagnose coarctation of the aorta antenatally.
The first reason for undiagnosed coarctation of the aorta is the morphogenesis of the pathology and the theory of the primary disorder of the development of the aortic arch. The theory was proposed in 1828 [11]. The author believes that this pathology is associated with insufficient connection of the 4th and 6th aortic arches with its descending section. Therefore, the isthmus is the place where the area of narrowing is most often localized [12], since both sections are formed from different embryonic primordia. Normally, the area of the aortic isthmus is equal to 2/3 of the diameter of the ascending aorta (Fig. 1).
Rice. 1.
The ascending section, arch and descending section of the fetal aorta in power Doppler mode are normal.
According to the “ductal tissue theory,” coarctation of the aorta occurs as a result of migration of ductal smooth muscle cells into the preductal aorta, followed by constriction and narrowing of the aortic lumen [4]. When coarctation of the aorta forms in the isthmus region, narrowing of varying length and shape remains (Fig. 2, 3). Most often this manifests itself in the form of a local constriction, above or below which the aortic diameter remains normal.
Rice. 2.
Ultrasound examination of the ascending section, arch and descending section of the aorta. The arrow indicates the location of the narrowing.
Rice. 3.
Three-dimensional image of the fetal heart and aorta at 16 weeks of gestation. The arrow indicates the location of the narrowing of the aorta. AO DESC - descending aorta, COR - heart.
Consequently, assessment of aortic narrowing in a typical location as a sign of developing pathology is not always possible in the early stages of pregnancy. Since we are talking about preductal coarctation of the aorta (narrowing of the aorta is localized proximal to the duct), it is obvious that during intrauterine life at a later date there is a decrease in blood flow through the left parts of the heart and the aortic isthmus and hypoplasia of the left ventricle and aorta develops. This contributes to the later manifestation of pathology and the possibility of its ultrasound diagnosis.
The second reason that makes it difficult to diagnose aortic coarctation is the theory of postnatal development. In the fetus, the aortic isthmus is narrow and after birth and closure of the ductus arteriosus it should normally widen to provide adequate blood flow to the descending aorta. Thus, the existing physiological narrowing of the aortic isthmus does not suggest the formation of aortic coarctation after birth.
Postductal coarctation develops after birth and is almost always an isolated defect. This anomaly most likely results from the proliferation of muscle tissue from the ductus arteriosus into the fetal aorta. When the duct narrows after birth, the ectopic tissue inside the aorta also contracts, blocking, like a tampon, the lumen of the vessel along its entire circumference. Unlike preductal coarctation, in this case, aortic hypoplasia does not develop. Closure of the ductus arteriosus in some children leads to narrowing of the aorta and the development of coarctation 2-3 weeks after birth [13].
The third reason for undiagnosed coarctation of the aorta is the peculiarities of intracardiac hemodynamics in the fetus. The blood circulation of the fetus, just like that of an adult, is subject to a number of basic laws of physical and biological influence. Blood flow moves from an area of high pressure to an area of low pressure. With a pronounced flow, the dimensions increase; with a decrease in flow volume, they decrease. Thus, hypoplasia of the left ventricle and coarctation of the aorta often accompany defects with reduced blood ejection into the aorta (aortic stenosis, ventricular septal defect) and practically do not occur with defects with a large volume of flow through the aorta (tetralogy of Fallot).
Based on the characteristics of intracardiac hemodynamics of the fetus, indirect signs of pathology in the antenatal period were proposed for the diagnosis of aortic coarctation: dilatation of the right ventricle and its hypertrophy (see Fig. 3), dilatation of the pulmonary artery [6, 7, 14]. The authors believe that these are reliable signs and they occur quite often (in 18 out of 24 cases of verified diagnoses of aortic coarctation). Therefore, it was proposed to evaluate the indices of the ratio of the cavity of the right ventricle to the left (normally - 1.1) and the pulmonary artery to the aorta (in healthy people - 1.2). Based on the increase in these parameters, it can be assumed that there is obstructed ejection into the aorta or hypoplasia of the aortic arch. However, according to the authors who proposed these indirect signs, such changes are detected only in 30% of observations (Fig. 4).
Rice. 4.
Disproportion in the size of the ventricles of the heart during coarctation of the aorta. RV - right ventricle; LV - left ventricle; AO DESC is a cross section of the descending aorta.
In the second half of the 90s. Several studies have been published to examine the diagnostic value of right ventricular enlargement and left ventricular enlargement in coarctation of the aorta. The authors who published these results [2] believe that the earlier the study is performed (from 14-16 to 25 weeks of gestation), the more informative it is for diagnosing aortic coarctation. Evidence can be provided by the data obtained by D. Brown et al. [15]. In the presented studies, coarctation of the aorta was noted in 8 (62%) of 13 fetuses with disproportion in the size of the ventricles before 34 weeks and only in 6 (21%) of 29 fetuses after 34 weeks of pregnancy. Despite the fact that more than half of cases of aortic coarctation are accompanied by a disproportion in the size of the ventricles, which is quite easily detected when studying a four-chamber section of the fetal heart, in many studies in Norway it was not diagnosed, even with mandatory screening studies of heart size before 18 weeks of pregnancy [9] .
Such contradictory results can be explained by the hemodynamic theory [16, 17]. In utero, 50% of the total blood ejection enters the ascending aorta, 65% enters the descending aorta, and only 25% passes through the aortic isthmus. Based on the reduced volume of blood flow, a physiological narrowing occurs, which worsens only after birth.
Dopplercardiography, which allows assessing blood flow, is informative only in cases of pronounced narrowing of the aorta [18]. In this case, there is an inverse relationship between the maximum blood flow velocity in the ascending and descending aorta. Normally, the speed in the ascending section slightly prevails over the speed of the descending section.
When the aortic arch is interrupted, retrograde blood flow is observed filling the area of the aortic arch after the interruption through the open ductus arteriosus and the absence of direct blood flow at the level of the interruption.
And finally, the last reason for undiagnosed coarctation of the aorta is the frequency of its combination with other cardiac anomalies. Isolated coarctation of the aorta is only 15-18%. According to M. Campell and P. Polani [19], the percentage of combination of aortic coarctation with cardiac anomalies ranges from 13 to 18%. Most often (85%), coarctation of the aorta is combined with a bicuspid aortic valve [20], often combined with endomyocardial fibroelastosis, extending to the outflow tract of the left ventricle and the interventricular septum. It is possible that in coarctation of the aorta, there is an anomalous origin of the right subclavian artery or both subclavian arteries from the descending aorta, distal to the coarctation (5%).
The presence of concomitant cardiac pathology can neutralize hemodynamic changes in the fetal heart that are typical for coarctation, which a specialist must pay attention to during ultrasound examination.
There is also the concept of pseudocoarctation, or “kinking” of the aorta - a deformation of the aorta, similar to classical coarctation, but the obstacle to blood flow is insignificant, since there is a simple elongation and tortuosity of the aorta (Fig. 5).
Rice. 5.
Kinking of the aorta in the fetus at 34 weeks of pregnancy. Research in energy mode.
So, it becomes obvious that practically none of the ultrasound signs in the antenatal period have a high degree of diagnostic accuracy.
It is known that the diagnosis of this heart defect is based on a direct sign - visualization of the site of narrowing of the aorta, and, possibly, expansion of the proximal aorta. However, it is quite difficult to clearly visualize the area of narrowing of the aorta in the fetus and is possible only in isolated observations. The defect can be seen only when there is a decrease in the diameter of the aortic isthmus by more than 1/3 compared to the norm for each stage of pregnancy (see Fig. 2, 3).
The key to the prenatal diagnosis of aortic coarctation is a comprehensive accounting of data obtained both from studying a four-chamber section of the heart (dilatation of the right ventricle, hypoplasia of the left ventricle) and from assessing the main arteries themselves. In the presence of coarctation, the diameter of the aorta is on average 2 times less than the diameter of the dilated pulmonary artery. Therefore, to diagnose coarctation of the aorta, imaging of the aorta itself should be used, which is most appropriate when screening through a three-vessel section. Diagnosis can be aided by measuring the diameter of the ductus arteriosus, which is wide in coarctation of the aorta.
The final diagnosis of coarctation of the aorta is established using a section through the aortic arch, since most often the narrowing of the aorta is noted in the area of its isthmus - at the level of the confluence of the ductus arteriosus. It should be noted that the narrowing can cover a large area of the aorta up to tubular hypoplasia. The normal transition of the aortic arch into the ductus arteriosus is normally smooth and smooth. In addition, when examining the aorta along the long axis, hypoplasia of the transverse part of the aortic arch should be considered the most reliable sign. As one of the indirect signs of aortic coarctation, the tortuosity of the aortic arch can be used when studying its long axis [2].
Doppler echocardiographic examination is of additional importance, which, in case of coarctation of the orta, makes it possible to identify the acceleration and turbulent nature of blood flow in the aorta. However, in the antenatal period this sign may not appear [2]. It is more reliable to identify a left-to-right shunt through the oval window. It is believed that this shunt is a compensatory mechanism to reduce blood flow into the left ventricle and aorta. G. Sharland et al. [18] noted a left-to-right shunt through the foramen ovale in 7 of 12 fetuses with aortic coarctation. In the remaining 5 fetuses, both left-right and right-left directions of blood flow through the oval window were detected.
In cases of pronounced anatomical changes in the aorta and left ventricular function, heart failure may occur with an increase in afterload [21]. Hemodynamic disorders and heart failure are characterized antenatally by the presence of pericardial effusion, a decrease in cardiac output with a decrease in the size of the left ventricle [22].
After birth and closure of the ductus arteriosus, all blood flow enters the ascending aorta and the isthmus expands to normal levels. After birth, when the duct is blocked, coarctation of the aorta leads to serious clinical manifestations.
So, an analysis of the possibilities and errors of ultrasound diagnostics of aortic coarctation in the prenatal period shows how problematic it is to make a diagnosis in all cases of this heart defect in the fetus. Unfortunately, all echocardiographic antenatal signs of pathology do not provide a high percentage of diagnosis.
I would like to hope that the development of new technologies and the accumulation of positive and analysis of negative experience will allow in the future to increase the percentage of diagnosis of such a complex heart defect with high neonatal mortality.
Literature
- Bronshtein M., Zimmer EZ Sonographic diagnosis of fetal coarctation of the aorta at 14-16 weeks of gestation // Ultrasound Obstetric Gynecologie. 1998. N 11. R. 254-257.
- Allan LD, Cook AC, Huggon IC Fetal Echocardiography. A practical guide. Cambridge University Press. 2009. P. 258.
- Frederiksen T. Coarctation of the aorta. A genetic study // Acta genet.1963. V. 13. R. 263.
- Buncle G. Congenital defects of the heart and large vessels. M.: Medicine, 1980.
- Oztunc F., Eroglu AG, Aksoy F. et al. Antenatal diagnosis of posductal coarctation of the aorta report // Turk journal Pediatr. 2001. V. 43. N 1. P. 67-69.
- Allan LD, Crawford DC, Tynan M. Evolution of coarctation of the aorta in intrauterine life // Br. Heart J. 1984. V. 52. P. 471.
- Allan LD, Crawford DC, Anderson RH et al. Echocardiography and anatomical correlations in fetal congenital heart disease // Br. Heart J. 1984. V. 52. P. 542.
- Franklin O., Burch M., Manning N. et al. Prenatal diagnosis of coarctation of the aorta improves survival and reduces morbility // Heart. 2002. V. 87. N 11. P. 67-69.
- Norbenger LK, Sahn DJ, Kleimann CS et al. Antenatal diagnosis of coarctation of the aorta: a multicenter experience // J. Am. Coll. Cardiologie. 1994. V. 23. P. 417-423.
- Bespalova U.D., Suratova O.G., Tyumeneva A.I., Gasanova R.M. Ultrasound diagnosis of congenital heart defects in the fetus / Ed. Boqueria L.A. M., 2009.
- Rosenberg H. Coarctation of the aorta; Morphology and pathogenesis considerations. In: Perspectives in Pediatric Pathology. V. 1. Chicago, Year Book, 1974.
- Patten BM The changes in circulation after birth // Am. Heart J. 1930. V. 6. P. 192.
- Burakovsky V.I., Bockeria L.A. Cardiovascular surgery. M.: Medicine, 1989.
- Allan LD, Chita SK, Anderson RH, Fagg N., Crawford DC, Tynan MJ Coarctation of the aorta in prenatal life: and echocardiographic, anatomical and functional study // Brit. Heart J. 1988. V. 59. P. 356.
- Brown DL, Durfee SM, Hornberger LK Ventricular disgrepancy as a sonographic sign of coarctation of the aorta: how reliable is it? // J. Ulytrasound Med. 1997. V. 16. N 2. P. 95-99.
- Rudolf A., Heyman MA, Spitznas U. Hemodynamic considerations in the development of narrowing of the aorta // Am. J. Cardiolog. 1972. V. 30. P. 514.
- Palmer NS, Berman MA Postnatal development of obstruction in coarctation of the aorta; Role of the ductus arteriosus // Pediatrics. 1975. V. 56. P. 462.
- Sharland GK, Chan KY, Allan LD Coarctation of the aorta: difficulties in prenatal diagnosis // Br. Heart J. 1994. V. 71. R. 70-75.
- Campell M., Polani PE Etiology of coarctation of the aorta // Lancet. 1961. V. 1. P. 473.
- Edwards JE, Burchell HB The pathological anatomy of deficiency betwen the aortic rood and the heart including aortic sinus aneuvrysms // Thorax 1957. V. 12. P. 125.
- Rudolph AM Congenital Diseases of the Heart: Clinical-Physiologic Considerations in Diagnosis and Management. Chicago-Year Book. 1974.
- Kleimman CS, Donnerstein RL, De Vore GR et al. Fetal echocardiography for evaluation of in utero congestive heart failure: A technique for study of nonimmune fetal hydrops. N.Engl. J. Med. 1982.
Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.
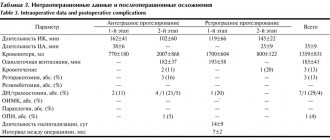
Material and methods
The study was conducted on 123 hearts taken at autopsy in city pathological and forensic departments from the corpses of patients of both sexes aged from 28 to 87 years (35 men and 57 women) who died from causes not related to diseases and injuries of the heart. The hearts were removed as a single complex along with the lungs, mediastinum, diaphragm and organs of the upper abdominal cavity. The heart chambers were washed with warm water to remove blood clots and blood clots. Through a cannula inserted into the thoracic aorta, after ligation of the large vessels of the aortic arch and coronary arteries, a solution of warm water was injected under a constant hydrostatic pressure of 0.18 bar, equivalent to 140 mmHg. to determine AA deficiency. In cases where the pressure in the aorta dropped rapidly, such hearts were assigned to the group with aortic valve insufficiency (group 2), which consisted of 15 hearts. The remaining hearts were assigned to the control group with preserved valve closure function (group 1), amounting to 108 hearts. Fixation of the preparations was carried out by continuous perfusion of an 8% formalin solution injected through a cannula into the aorta under a pressure of 0.18 bar (140 mm Hg) and into the superior vena cava under a pressure of 0.02 bar (15 mm Hg). within 5 days.
For the study, morphometric methods were used on freshly fixed preparations, on preparations made by silicone plastination at room temperature, as well as on preparations of hearts in which the chambers and large vessels were filled with a polymerized colored silicone composition with the addition of radiopaque red lead. In addition to morphometry, injected and plastinated hearts were examined using computed tomography and magnetic resonance imaging.
To prepare an injectable colored radiopaque silicone composition, a mixture of 92 parts by mass of SKTN E grade silicone, 5 parts by mass of red lead and 3 parts by mass of hardener K-1 was used. All components were thoroughly mixed until a homogeneous mass was obtained immediately before injection. A radiopaque composition was injected through a cannula installed into the ascending aorta at a pressure of 100 mmHg. Art., which contributed to the closure of A.K. The left ventricle and left atrium were filled through a cannula inserted into the left atrial appendage at a pressure of 20 mm Hg, which allowed filling the left chambers of the heart and maintaining their natural shape. To accelerate the polymerization of silicone, the organocomplex of the heart and lungs was immersed in warm water for 3-4 hours. This injection technique made it possible to maintain the relationship between the original geometry of the aortic root and the intracardiac structures of the left parts of the heart with the A.C. closed. After the silicone hardened, computed tomography of the injected heart was performed, after which modified preparation and morphometry techniques were used.
In all preparations, the circumference of the cross section of the ascending aorta, sinotubular junction (SJ), basal ring of the aorta, the length of the base and height of the intercuspid triangle of the aorta were measured (Fig. 1).
Rice. 1. Photograph of the parameters of the interleaf triangle by A.K. The aorta and left chambers are injected with silicone. 1 — length of the base of the inter-flap triangle; 2 — height of the inter-flap triangle. as well as the magnitude of the deflection angle of the inter-flap triangle (Fig. 2).
Rice. 2. Three-dimensional reconstruction of the AC on a multislice computed tomogram. The angle of deviation (α) of the inter-valvular triangle of the AC from the plane of the longitudinal section of the ascending aorta. The area of the intervessel triangle and AC regurgitation were also calculated using the formulas:
S
tr.=
p
(
p
–
a
)(
p
–
b
)(
p
–
c
),
S
reg.=π·
r
2,
where S
tr.
- area of a triangle; a
,
b
,
c
- sides of the triangle;
p
is the semi-perimeter of the triangle;
where S
reg.
- area of regurgitation; r
is the radius of regurgitation.
Measurement of the angle of deviation of the inter-valvular triangles of the AC from the plane of the longitudinal section of the aortic root was carried out using multislice computed tomography (MSCT) preparations (see Fig. 2). The base of the inter-valvular triangle is a straight line drawn from the lower point of attachment of one semilunar valve to the aortic wall to the lower point of attachment of the other. The apex of the inter-flap triangle is the upper point of the commissure of the AK flap.
After the measurements, the AC valves were assessed for the presence of commissural fenestrations. Particular attention was paid to the areas of the valves at the site of their attachment to the aortic wall and to the apex of the inter-valve triangle. Morphological changes were assessed according to the degree of degenerative changes: degree I - the presence of changes only in the semilunar valves (thinning, discoloration, atherosclerotic changes) without their calcification; II degree - the presence of changes in the semilunar valves (thinning, discoloration, atherosclerotic changes) in combination with fenestrations in the commissural areas of the valves and/or the presence of calcification of the aortic wall; III degree - the presence of changes in the semilunar valves (thinning, discoloration, atherosclerotic changes) in combination with fenestrations in the commissural areas of the valves and the presence of calcification in the inter-valve triangles.
Statistical processing of the obtained data was carried out using the IBM SPSS (Statistical Package for the Social Sciences) program version 20.0 for Windows. The method of multiple logistic regression analysis was used. The level of statistical significance of the differences was taken as 0.05.