Chronic arterial hypertension is a common medical problem of the 21st century, with which people of different ages turn to specialists in developed countries.
Specialists at the Yusupov Hospital diagnose and treat patients with arterial hypertension. The appearance of symptoms of hypertension should be a reason to consult a doctor.
Doctors have modern methods of treating hypertension at their disposal. Achieving a positive result in the treatment of hypertension is possible only with an integrated approach and careful adherence to the instructions of a specialist.
A timely examination can save your life and health.
Hypertension: general information
With arterial hypertension, a person constantly experiences high blood pressure. This condition occurs due to spasm of blood vessels, as a result of which blood flow through them becomes difficult. The diagnosis of arterial hypertension is made by a specialist when there is a stable increase in systolic pressure above 140 mmHg. Art.
To determine pressure, it is necessary to take at least three measurements at different times. The patient should be in a calm state and not take medications that lower or increase blood pressure.
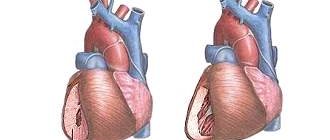
Features of the course of hypertension with heart damage
A prolonged or particularly malignant course of the disease affects the heart muscle. Initially, myocardial hypertrophy develops - with the help of this, the heart tries to compensate for the excess load. Without treatment or if it is insufficiently effective, as well as with irregular medication use, the following types of heart damage may develop:
- angina pectoris - acute pain in the heart caused by a lack of oxygen;
- heart attack - an extreme degree of coronary artery disease, manifested by necrosis of the heart muscle;
- acute left ventricular failure - manifested by cardiac edema.
Causes of arterial hypertension
Experts fail to establish the causes of arterial hypertension in 90% of cases. In 10% of cases, the disease can develop as a complication of another disease or as a result of taking medications. The risk of developing hypertension syndrome may increase due to several factors:
- hereditary predisposition;
- age and gender of the person;
- smoking;
- frequent stressful situations;
- drinking alcohol in large quantities;
- excessive consumption of salt in food;
- low mobility and obesity;
- kidney diseases;
- metabolic disorder;
- diabetes.
Course of hypertension
The risk associated with increased blood pressure is continuous, with each 2-3 mmHg increase in systolic blood pressure. Art.
Hypertension increases the risk of mortality from coronary heart disease by 7% and the risk of mortality from stroke by 10%. The most common immediate cause of death associated with hypertension is heart disease, but death from kidney failure is also common.
Complications arise directly from increased blood pressure (cerebral hemorrhage, retinopathy, left ventricular hypertrophy, congestive heart failure, arterial aneurysm and vascular rupture), from atherosclerosis (increased coronary, cerebral and renal vascular resistance), as well as from decreased blood flow and ischemia ( myocardial infarction, cerebral thrombosis, infarction and renal nephrosclerosis).
If your blood pressure is not well controlled, you are at risk of:
- Bleeding from the aorta, the largest blood vessel,
- Chronic kidney disease,
- Heart attack or heart failure,
- Poor blood supply to the legs,
- Vision problems
- Stroke,
- Disturbance of cerebral blood supply.
Types of arterial hypertension
The classification of arterial hypertension is based on various parameters, one of which is the origin. Based on origin, the patient can be diagnosed with:
- Primary arterial hypertension is caused by many factors, which are being elucidated by specialists all over the world. However, it has been reliably established that the basis of this disease is unfavorable heredity in combination with the factors acting on it. The vast majority of patients - about 90% - suffer from this type of arterial hypertension. This disease has a second name – essential hypertension;
- Secondary arterial hypertension manifests itself when organs involved in the regulation of blood pressure are damaged, therefore the disease is otherwise called symptomatic arterial hypertension.
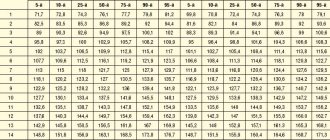
Classification of hypertension
There is no single classification, but the one recommended by WHO is most often used. Hypertension, depending on the degree of increase in pressure, is divided into three stages:
Stage 1 hypertension. Soft or borderline stage. The pressure is 140/90 mm Hg. or higher.
Stage 2 hypertension. Moderate stage. The pressure is 160/100 mmHg. or higher.
Hypertension stage 3. Severe form of hypertension. Clinical systolic blood pressure is 180 mmHg. or higher, and diastolic is 110 mm Hg. or higher.
The disease is also divided into three stages, depending on the degree of development:
Stage 1: slight increase in blood pressure. There are no complaints, the functioning of the cardiovascular system is not impaired.
Stage 2: constant increase in blood pressure and associated enlargement of the left ventricle of the heart.
Stage 3: increased blood pressure affects the functioning of the heart, brain and kidneys.
Diagnosis of arterial hypertension
With this disease, irreversible changes occur in the body that require immediate treatment. Diagnostics takes place in several stages and includes an examination by a specialist and collection of materials for making a diagnosis.
Diagnosis of a patient begins with measuring blood pressure; at least three measurements are required to confirm the diagnosis. If high indicators are obtained, the patient is sent for laboratory and instrumental studies:
- electrocardiogram;
- general and clinical urine analysis;
- biochemical detailed blood test;
- Ultrasound of the heart and internal organs.
The examination regimen is selected by the doctor individually for each patient. If the doctor assumes that the patient has secondary arterial hypertension, the classification of which is extensive, additional studies are carried out on organs whose dysfunction could cause arterial hypertension.
Diagnosis and treatment of hypertension
Diagnosis of the disease
Diagnosis of hypertension at the A-Media clinic is carried out using the following methods:
- blood pressure measurement
- ECG
- 24-hour ECG monitoring with blood pressure (Holter monitoring)
- echocardiography (echocardiography or ultrasound of the heart)
- Ultrasound of the abdominal cavity with kidneys
- Ultrasound Dopplerography of the BCA (ultrasound Dopplerography of brachiocephalic arteries and veins).
Treatments for hypertension
Treatment of hypertension in our clinic is planned by a qualified cardiologist only after an accurate diagnosis has been made.
First step: Our doctor will take measures to lower the patient's blood pressure.
Further therapy is planned individually based on the type of hypertension. Mild and moderate forms of the disease can be treated with medications. For severe hypertension, antihypertensive drugs are always prescribed. Lifestyle modification is a prerequisite.
Classification of arterial hypertension
During the study of arterial hypertension, specialists have developed several classifications on various grounds: etiology, causes of increased pressure, degree of damage to systems and organs, stability and level of pressure, nature of the development of the disease. Some classifications have not lost their relevance over time: according to the stages and extent of the disease.
Based on the recommendations of the World Health Organization, a classification by pressure level has been developed, which has practical significance; the following conditions and degrees of arterial hypertension are distinguished:
- Optimal blood pressure is 120/80 mm Hg. Art.;
- normal blood pressure does not exceed 120/80 – 129/84 mm Hg. Art.;
- borderline blood pressure is in the range of 140/90 – 159/99 mm Hg. Art.;
- Arterial hypertension of the 1st degree is diagnosed when the pressure level is from 140/90 to 159/99 mm Hg. Art. In international practice, risk factors are taken into account when making a diagnosis. So, in a person with given blood pressure levels and in the absence of aggravating factors, a diagnosis can be made: arterial hypertension, stage 2, risk 1;
- Arterial hypertension of the 2nd degree is characterized by blood pressure in the range of 160/100 – 179/109 mm Hg. Art. With one or two aggravating factors, grade 2 arterial hypertension is noted, risk 2;
- Arterial hypertension of the 3rd degree is observed in a patient with a pressure of 180/110 mm Hg. Art. and higher. If more than three aggravating factors are present, arterial hypertension of the 3rd degree, risk 3, is diagnosed. If organ damage is observed, then the diagnosis of arterial hypertension of the 3rd degree, risk 4 is established;
- isolated arterial hypertension is characterized by a systolic blood pressure equal to or exceeding 140, and a diastolic blood pressure below 90 mmHg.
Classification of the disease is important in diagnosing hypertension and determining treatment options depending on the degree and stage. Thus, arterial hypertension of the 1st degree, risk 2, and arterial hypertension of the 2nd degree, risk 3, suggest different methods of treating hypertension.
Degrees and stages of hypertension
Hypertension is classified according to stages and degrees. The division into degrees is based on the level of pressure rise:
- I degree - rise in systolic pressure above 139 up to 159 mm Hg. art (diastolic fluctuates in the range of 90-99 mm Hg);
- II degree - from 160 to 170 mm Hg. Art. (diastolic oscillation interval - 100-109);
- III degree - pressure rises above 180 mm Hg. Art.
The stage of hypertension also takes into account the degree of target organ damage:
- Stage 1 (low risk) - mild hypertension, in which there is no damage to target organs;
- Stage 2 (high risk) - moderate or severe course of the disease, in which target organs are involved in the process: cardiac hypertrophy, spasm of the retinal arteries, deterioration of renal blood flow;
- Stage 3 (very high risk) - an extremely severe course, accompanied by frequent hypertensive crises and dangerous damage to target organs in the form of stroke, heart attack, and retinal hemorrhages.
Classification of arterial hypertension by stages
Currently, doctors use a classification based on the nature of organ damage, which distinguishes 3 stages of arterial hypertension:
- arterial hypertension stage 1. At this stage, the patient experiences an intermittent and slight increase in blood pressure, and there are no complaints. The functioning of the cardiovascular system is not impaired.
- Arterial hypertension stage 2, in particular degree 2, is characterized by increased blood pressure. At this stage of the development of the disease, the left ventricle enlarges, and narrowing of the retinal vessels may also be observed.
- arterial hypertension stage 3. This stage is characterized by the following patient conditions: angina pectoris, heart failure, heart attack, stroke, renal failure, disturbances in the blood supply to the brain and eyes.
Symptoms of hypertension
The severity of clinical symptoms depends on the level of pressure increase and the involvement of the so-called target organs in the process. This term refers to those organs on which a prolonged increase in pressure affects the most unfavorably: the retina of the eyes, the brain, the kidneys, the heart.
At the initial stage, patients are usually bothered by dizziness and periodic headaches. An increase in pressure is usually accompanied by tinnitus, nausea, palpitations, and pulsation in the head.
The progression of the disease leads to symptoms of heart failure: shortness of breath during exercise, a feeling of lack of air. The chronic nature of the pathology is accompanied by swelling of the legs and puffiness of the face.
When blood pressure jumps, visual impairment may occur in the form of “floaters” in front of the eyes and decreased visual acuity. The most important symptom is an increase in pressure, confirmed instrumentally!
Arterial hypertension: treatment with modern methods
The choice of treatment for hypertension is made by specialists based on research data. Treatment methods for arterial hypertension are divided into non-pharmacological and medicinal.
Patients diagnosed with mild hypertension, in particular stage 1 arterial hypertension, may be exempted by their doctor from taking special medications. The main method of non-drug treatment is changing the patient’s lifestyle:
- rejection of bad habits;
- weight control;
- regular moderate physical activity. Daily activities such as moderate walking or light strength training are effective;
- reducing stress. During stressful situations, a person’s blood pressure may increase; it can be lowered with the help of massage, breathing exercises or meditation;
- including foods rich in macro- and microelements in the diet and reducing salt intake.
Medicines for arterial hypertension are prescribed to patients when non-drug therapy has proven ineffective within 3-4 months, and there are risk factors. Thus, arterial hypertension 2 risk 3 requires taking special medications. The number of drugs is determined by blood pressure and the presence of concomitant diseases.
Modern doctors prescribe drugs for the treatment of arterial hypertension in accordance with one of the strategies: monotherapy or combination therapy. When drawing up a treatment plan, the question of the admissibility of using one drug is the most pressing for the specialist.
In monotherapy, a patient with grade I is prescribed one drug at the beginning of the course of treatment. An important factor when prescribing a drug is its effectiveness in reducing the risk of complications. Currently, to control blood pressure, doctors use the most studied drugs belonging to two groups: thiazide-like and thiazide diuretics, which have a diuretic effect.
Combination therapy is prescribed to patients with a high degree of risk, as well as with stages II and III of the disease. With this method of treatment, drugs with different mechanisms of action are selected to lower blood pressure and reduce possible side effects.
Experts on the question of how, if a patient has arterial hypertension, how to treat this disease with drugs, prefer to use several groups of drugs:
- beta blockers. For several decades, beta blockers have been used as the mainstay of treatment for hypertension in children and adolescents. However, multiple side effects have now been identified, and therefore their use has become limited. Experts include the main side effects: sleep disturbances, increased blood glucose levels, weakness and mood swings. An important condition when using these funds is an electrocardiogram and regular monitoring of blood sugar;
- Diuretics are prescribed to patients for a long period; they remove excess fluid from the body. Side effects include: fainting, decreased calcium levels in the blood;
- calcium channel blockers. Drugs in this group are used quite widely to treat patients; doctors give preference to drugs with a long period of action. Side effects of blockers include: gastrointestinal disorders, rapid heartbeat, weakness, dizziness and swelling;
- ACE inhibitors. The mechanism of action of these drugs is to block the action of enzymes that are involved in the formation of a vasoconstrictor;
- alpha adenoblockers. The effect of drugs in this group is manifested in a decrease in pressure through blocking receptors located in the artery wall.
Description of hypertension
Hypertension is a widespread pathology of the cardiovascular system, which is characterized by a persistent or transient increase in arterial (blood) pressure.
Today, medicine knows that hypertension is a systemic disease that affects many human organs.
At the onset of the disease, an increase in blood pressure (blood pressure) may not affect the patient’s condition. Depending on the severity of the process, hypertension can cause destruction in the structures of the heart muscle, brain, kidneys and eyes.
Degrees of hypertension and risk groups
There are three degrees of severity of hypertension:
- Hypertension of the 1st degree (mild form).
- Hypertension of the 2nd degree (hypertension of moderate severity).
- Hypertension of the 3rd degree (the most severe degree).
The severity of hypertension is always determined together with risk factors for the development of possible complications from the cardiovascular system.
Based on these factors, the cardiologist predicts hypertension.
There are four risk groups for hypertension:
- risk 1 (lowest)
- risk 2 (medium)
- risk 3 (high)
- risk 4 (very high).
Accurate determination of the type of hypertension is of great therapeutic importance. Lack of adequate treatment for hypertension can cause the development of a hypertensive crisis.
Prognosis for arterial hypertension
Treatment of vasorenal arterial hypertension and the prognosis for this disease depend on the patient’s compliance with the recommendations of the attending physician and the adequacy of the prescribed therapy. The prognosis for hypertension can be quite favorable. However, for this it is important to identify the problem in a timely manner and develop treatment tactics.
The prognosis for women, as medical practice shows, is more favorable than for men. The course of the disease is influenced by the following factors: the rate of development of the disease, the stability of pressure and the presence of diseases of other organs and systems. Modern standards of treatment for arterial hypertension make it possible to achieve success in more than 85% of cases.
Treatment of hypertension at the Innovative Vascular Center
Our clinics employ experienced cardiologists who can accurately determine the causes of high blood pressure and prescribe therapy appropriate to the causes and stage of the disease.
In case of hypertension, we always conduct a thorough diagnostic search, identifying all possible causes of secondary hypertension, especially those related to vascular damage (vasorenal hypertension, increased blood pressure due to narrowing of the carotid arteries, in the presence of adrenal tumors).
At the Innovative Vascular Center, it is possible to correct the causes of arterial hypertension using endovascular methods (stenting of the renal arteries, radiofrequency denervation of the renal arteries).
Prevention of arterial hypertension
Giving up bad habits and normalizing lifestyle are the basis for preventing hypertension. Knowledge of the principles of preventing hypertension allows you to prevent the disease, facilitate its course, and also eliminate possible complications. Experts distinguish between primary and secondary prevention.
Primary prevention is to prevent the development of hypertension. People at high risk of developing arterial hypertension should not only fight bad habits and adhere to the principles of proper nutrition, but also monitor their physical activity.
Secondary preventive measures are carried out for people with an established diagnosis, for example, gestational hypertension. The efforts of doctors and patients are aimed at preventing complications. Secondary prevention consists of two components: arterial hypertension (treatment with tablets) and non-drug treatment.
Doctors at the Yusupov Hospital have extensive experience in treating arterial hypertension. The quality of services provided in the hospital is at the European level. All diagnostic and treatment procedures are performed using the latest medical equipment. The rooms are equipped with maximum comfort for patients. You can make an appointment with a doctor by phone.
Symptoms of hypertension
Signs of the disease may manifest themselves differently depending on the stage at which hypertension occurs.
Symptoms that are most often observed with hypertension:
- headaches and dizziness of various types
- feeling of heaviness and pulsation in the back of the head
- cardiopalmus
- general weakness
- problems with coordination of movements (sometimes)
- intolerance to loud sounds
- photophobia
- nosebleeds
- nausea
- feeling of fear.
If symptoms appear, make an appointment with a cardiologist to diagnose and treat a possible disease.