Sedatives are medications that reduce increased irritability, conflict, nervous tension, and have a slight calming effect by reducing the excitability of the nervous system.
Despite the wide selection of drugs with a pronounced sedative effect (tranquilizers), sedatives are used very actively, especially in cases of high nervous excitability, irritability, sleep disturbances, especially associated with negative emotions, and neurosis-like conditions that are accompanied by heart pain.
Unlike tranquilizers, sedatives, especially herbal ones, do not have such a pronounced calming effect. At the same time, sedatives are well tolerated by patients, they do not have serious negative effects - they do not cause muscle relaxation, gait disturbances, a feeling of lethargy, or a decrease in the speed of mental reactions.
To sedatives, addiction does not develop (decrease in effect with long-term use) and drug dependence (an irresistible need to use the drug again and again).
Due to these advantages, sedatives are very widely used throughout the world.
Indications for use
Sedatives are used to treat neurasthenia - conditions that are accompanied by increased irritability, absent-mindedness, conflict, and nervous tension.
In addition, sedatives are used in the complex treatment of diseases that are easily aggravated by stress - angina pectoris (oxygen starvation of the heart), hypertension (persistently high blood pressure), gastric and duodenal ulcers, pruritic neurodermatoses (skin diseases that are accompanied by itching). ), migraine.
In addition, sedatives are used for hysteria, menopausal syndrome, and vegetative-vascular dystonia.
Classification of sedatives
Based on their origin, sedatives that are widely used in clinical practice are grouped into the following classes:
- herbal preparations: valerian extract, motherwort tincture, peony tincture, hawthorn tincture, passionflower extract, mint herb, lemon balm herb and combinations thereof;
- synthetic drugs: sodium bromide, potassium bromide, magnesium lactate, magnesium sulfate, phenobarbital.
In addition, many psychoactive substances can have a sedative effect and reduce the level of irritability. These drugs include anxiolytics (tranquilizers), antidepressants, some antipsychotics, as well as antiarrhythmic and antihypertensive drugs (for example, the β-blocker propranolol) and antihistamines and antiallergic drugs (for example, diphenhydramine).
Sedatives and hypnotics
Sedatives (from the Latin Sedatio - calm) have a regulatory effect on the processes of inhibition and excitation in the central nervous system, facilitate the onset of sleep, enhance the effect of hypnotics, analgesics and other neurotropic substances. They are usually well tolerated, do not cause serious side effects, addiction or dependence, and do not have extensive contraindications for use. This group of drugs includes preparations of valerian and other plants, bromides.
| | Attention! Do not start pharmacological treatment without consulting a psychiatrist |
1. Rhizomes with roots of valerian (Rhizomatа cum radicibus Valerianae). They prepare tinctures, infusions, valerian extracts, sedative mixtures, and make camphor-valerian drops. Valerian preparations contain essential oil, the main part of which is the ester of borneol and isovaleric acid, free valeric acid and borneol, organic acids, including valeric acid (C-15 H-12 0–2), which has an antispasmodic effect, tannins, alkaloids, sugars and other substances.
2. Valocormidum . Ingredients: velerian tincture (10 ml), lily of the valley tincture (10 ml), belladonna tincture (5 ml), sodium bromide (4 g), menthol (0.25 g), distilled water (up to 30 ml). Soothing and antispasmodic. Used to treat cardiovascular neuroses accompanied by bradycardia. Prescribe 10–20 drops 2–3 times a day before meals. Available in 30 ml bottles.
3. Valosedan . Ingredients: valerian extract (0.3 g), hop tincture (0.15 g), hawthorn tincture (0.133 g), rhubarb tincture (0.83 g), sodium barbital (0.2 g), ethyl alcohol (20 ml ), distilled water (up to 100 ml). Used to treat neuroses and neurosis-like conditions, 1 teaspoon 2-3 times a day.
4. Corvalolum. Composition: ethyl ester of a-bromoisovaleric acid (about 2%), phenobarbital (1.82%), sodium hydroxide (to convert phenobarbital into soluble phenobarbital sodium - about 3%), peppermint oil (0.14%), mixture ethyl alcohol 96% and distilled water up to 100%. Similar to foreign Valocordin (milocordin). Has a sedative, mild hypnotic, antispasmodic effect. Used to treat neurasthenia with irritable weakness, mild coronary spasms, tachycardia, sleep disorders, intestinal spasms, early stages of hypertension. Prescribed orally before meals, 15–30 drops 2–3 times a day. The dose can be increased to 40–50 drops (for tachycardia and vascular spasms). Available in 15 ml bottles.
5. Motherwort herb (Herba Leonuri). Contains essential oil, saponins, tannins, alkaloids. In terms of action and indications for use, it is close to valerian. Motherwort tincture (Tinktura Leonuri) is taken 30–50 drops 3–4 times a day before meals. Liquid motherwort extract is taken 20 drops 3 times a day.
6. Passionflower herb (Herba Passiflorae). Passionflower tincture and extract have a calming and anticonvulsant effect. Passionflower extract is taken 20–40 drops 2–3 per day for 20–30 days.
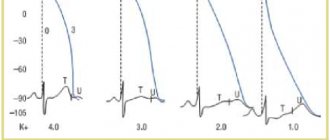
7. Sodium bromide (Natrii bromidum). Used as a sedative and anticonvulsant. It is prescribed orally before meals in tablets and mixtures, as well as intravenously. When taken orally, the dose for adults is from 0.1 to 1 g 3-4 times a day. For children under 1 year - 0.05-0.1 g, up to 2 years - 0.15 g, 3-4 years - 0.2 g, 5-6 years - 0.25 g, 7-9 years — 0.3 g, 10–14 years — 0.4–0.5 g. Available in powders and tablets of 0.5 g; 3% solution in 100 ml bottles.
8. Potassium bromide (Kalii bromidum). Prescribed orally 0.5 g 2-3 times a day. In pediatric practice, a solution of potassium bromide (1%, 2% and 3%) is used.
9. Bromcamphora. Prescribed orally after meals in powders, tablets for adults - 0.15-0.5 g 2-3 times a day, children under 2 years old - 0.05 g, 3-6 years old - 0.1 g, 7-9 years old - 0.15 g, 10-14 years - 0.15-0.25 g 2-3 times a day.
10. Sympathil. Sedative, calming combined remedy (includes in one tablet dry esolate extract 20 mg, hawthorn flower extract 75 mg, magnesium oxide 124.35 mg, microcrystalline cellulose, salt carboxymethyl starch (type A), stearic acid, azorubine (E 122). Eliminates anxiety , increased emotionality, reduces the excitability of the central nervous system and cardiovascular system, normalizes sleep.
Prescribed orally before meals, 2 tablets per day (morning and evening).
Side effects: gastralgia, diarrhea. Contraindications for use: severe renal failure, hypersensitivity, pregnancy, breastfeeding. It is not recommended to combine with medications containing quinidine (renal excretion of quinidine is reduced due to alkalinization of urine and its overdose is possible). In case of an overdose of Sympathil, there may be a delay in urination.
Release form: tablets.
Sleeping pills, or hypnotics, are no longer the same as they were used relatively recently. Barbiturates have practically gone out of use; their place has been taken by tranquilizers with a hypnotic effect, antidepressants, and some neuroleptics. However, the new drugs are far from ideal sleeping pills. The following sleeping pills are mainly used.
1–3. Nitrazepam, flunitrozepam, triazolam - see “Tranquilizers”.
4. Bromizovalum. N-(a-bromoisovalerianyl)-urea. Synonyms: Bromural, Bromodorm, Sedural, Somnurol, etc. Has a calming and moderate hypnotic effect. Well tolerated. As a sedative, adults are prescribed 0.3-0.6 g 1-2 times a day, and as a sleeping pill - 0.6-0.75 g half an hour before bedtime. For children, bromizal is prescribed for insomnia, chorea, whooping cough, 0.03–0.1–0.25 g per dose. Available in tablets of 0.3 g in a package of 10 pieces. It is included in the anticonvulsant drugs gluferal, pagluferal, and in the Sereysky mixture.
5. Methaqualone . Synonyms: Dormogen, Dormotil, Motolon, Bendor, Holodorm, Mekvalon, Revonal, Somnidon, Tofinal, etc. A sedative, hypnotic with anticonvulsant and antitussive effects. Enhances the effect of barbiturates, analgesics, and neuroleptics. Mainly used in the treatment of insomnia. Prescribe 0.2 g orally half an hour before bedtime. When waking up early, take another 0.1 g. It is usually well tolerated. Available in tablets of 0.2 g in a package of 10 pieces.
6. Zopiclone - see "Tranquilizers".
7. Hemineurin. Synonyms: Geminevrin, Chlomethiazole, Somnevrin, etc. It is a derivative of chlormethiazole. It has a sedative, hypnotic and anticonvulsant effect. Indicated for the treatment of sleep disorders, status epilepticus, delirium, eclampsia and pre-eclamptic conditions, alcohol withdrawal, for the relief of mania, acute psychomotor agitation and pain relief during labor.
Prescribed orally and intravenously. As a sleeping pill, 2-4 capsules are prescribed (in capsules the drug is absorbed faster and acts more actively than in tablets) or tablets before bedtime, as a sedative - 1-2 capsules (tablets) 1-2 times a day before meals. For status epilepticus and delirium, the drug is administered intravenously in a stream of 40–100 ml of a 0.8% solution for 3–5 minutes or intravenously in a drip of 60–150 drops per minute until sleep; then the infusion is slowed down, maintaining shallow sleep (a total of up to 500–1000 ml is administered). Acute withdrawal syndrome is stopped by prescribing 2–4 capsules orally on the first day (after half an hour you can add 2 more capsules), on the 2nd and 3rd days - 3 capsules, on the 4th–6th day - 2 capsules and subsequent 4 days - 1 capsule. Mania is relieved by intravenous infusion of 40–80 ml of a 0.8% solution of the drug; for eclampsia, 30–50 ml of solution is administered dropwise (60 drops per minute), and upon the onset of drowsiness, the dose is reduced to 15–10 drops per minute. For labor pain relief, 2-3 capsules are prescribed, adding 2-3 capsules every 3 hours if necessary (no more than 7 capsules in total).
Side effects: local phlebitis, respiratory depression, hypotension and collapse, dyspepsia, allergic reactions. Patients with alcoholism may become dependent on the drug, so it should not be prescribed for more than 7 days in a row.
Release forms: capsules and tablets of 500 mg of gemineurin; 0.8% solution in bottles of 100 and 500 ml.
8. Ivadal. Synonym: Zolpidem, Ivadal. Selectively excites the omega 1 receptor subtype of the GABA-A receptor complex, promotes the opening of chloride channels, and potentiates inhibition processes in the central nervous system. Strengthens (mutually) the effect of sedatives, is incompatible with alcohol. In therapeutic doses, it shortens the period of falling asleep, reduces the number of night awakenings, lengthens the duration of the 2nd–4th phases of slow-wave sleep, and improves its quality. Indicated for the treatment of sleep disorders.
It is prescribed orally just before bedtime, once. The dose is individual. Adult patients are usually given 10 mg, persons over 65 years of age - 5 mg (if necessary - no more than 10 mg). For situational sleep disturbances, the drug is taken for 2–7 days, for chronic insomnia - up to a month, no more.
Side effects: drowsiness, headache, dizziness, gait disturbance, agitation (at night or upon cessation of treatment), anterograde amnesia, confusion, visual disturbances, nightmares, abdominal pain, dyspepsia, skin rash, itching; with long-term therapy - addiction, dependence.
Contraindications for use: sleep apnea, severe myasthenia gravis, severe respiratory or liver failure, breastfeeding, pregnancy, breastfeeding, hypersensitivity. In case of overdose - stunning consciousness up to coma (gastric lavage, intake of activated charcoal, symptomatic therapy are necessary). Use with caution in case of respiratory and liver failure; combination with benzodiazepines is undesirable.
Release form: tablets of 10 mg in packages of 7 and 10 pieces.
For other drugs with sedative and hypnotic effects, see the headings “Neuroleptics”, “Antidepressants”, “Tranquilizers” and “Nootropics”.
Back to contents
Basics of sedative treatment
Sedatives are safe even with long-term use, so they are classified as over-the-counter medications.
The effectiveness of sedatives does not decrease with prolonged use. There is no physical or mental dependence on these drugs – an irresistible need to take them constantly.
Sedatives usually do not reduce daytime performance; moreover, they can even increase it, relieving excessive irritability and emotional stress.
Features of the treatment of neurasthenia
Tinctures and alcohol extracts contain ethanol, which causes the main side effects - general weakness, fatigue, indifference to the environment, weakened memory, drowsiness.
In addition, alcohol-containing sedatives reduce physical and mental abilities, so they are not recommended for use by patients whose work requires quick mental, behavioral and emotional reactions - drivers, dispatchers, operators, etc., as well as people with alcohol addiction. Such patients need to choose drugs without alcohol, for example, dry plant extracts or combinations thereof.
All sedatives enhance the effect of other drugs that depress the central nervous system - antipsychotics, tranquilizers, anticonvulsants.
Most sedatives cause a decrease in libido and potency.
Quick help for a panic attack
Benzodiazepine tranquilizers
The most effective and fastest-acting medications for panic attacks are a group of benzodiazepine tranquilizers
. These include:
- alprazolam (Xanax),
- clonazepam,
- diazepam (Relanium),
- bromodihydrochlorophenylbenzodiazepine (phenazepam).
These are potent drugs and therefore are not commercially available. They can be purchased using special prescriptions, which can only be prescribed by certified doctors in licensed clinics.
The action of benzodiazepine tranquilizers provides rapid relief of anxiety, vegetative manifestations (rapid pulse and breathing, sweating, trembling, chills and heat waves, dizziness, etc.), normalization of sleep and appetite.
Since the basis of any panic attack is anxiety and excessive activation of brain structures responsible for the protective anxiety reflex, then, regardless of the causes, mechanism of development and manifestation of panic, tranquilizers always have a quick effect. They will either prevent the development of a panic attack, or (if it has already begun) stop it.
Benzodiazepine tranquilizers are used once - as an ambulance, or in short courses (usually no more than a week). With long-term use, dependence is formed, one of the manifestations of which will be “increasing tolerance” - the need to increase the dose to achieve an effect.
These drugs are often used in tablet form. As a rule, taking one tranquilizer tablet ensures the development of a therapeutic effect in 20-40 minutes.
Some of these drugs (diazepam, bromodihydrochlorophenylbenzodiazepine) exist in the form of a solution, which allows them to be used as injections intramuscularly or intravenously, in which case the effect occurs very quickly - from a few seconds to several minutes.
Advantages of benzodiazepine tranquilizers: pronounced anti-anxiety effect, rapid onset of action, well tolerated.
Disadvantages: difficult to purchase (you need a doctor's prescription, a special prescription form), a common side effect is drowsiness and lethargy; if taken regularly, they can cause physical and mental dependence.
Non-benzodiazepine tranquilizers
The next group is non-benzodiazepine tranquilizers
. They are distinguished from the first group by a different chemical structure. The most common representatives:
- hydroxyzine (atarax),
- mebicar,
- etifoxine,
- meprobamate.
In terms of potency, they are inferior to the drugs of the previous group. But they also have their advantages: they are well tolerated, do not cause drowsiness, do not develop dependence, and are easier to purchase in pharmacies (no special prescriptions are needed).
The most common remedy in this group is ATARAX
. They can be used once to prevent or relieve a panic attack. It is also used for long-term use, which can prevent the recurrence of a panic attack.
Thus, tranquilizers
- the most common and popular group of pills for panic attacks. It has been noticed that many people who have long gotten rid of panic attacks, but remember these unpleasant anxiety states, try to carry a tranquilizer pill with them “just in case.”
Neuroleptics
Neuroleptics with sedative action. This is the next group of drugs that have a sedative effect and can relieve a panic attack. The most common tablets are:
- Thioridazine (Sonapax);
- Periciazine (neuleptil);
- Chlorprothixene (Truxal);
- Quetiapine (Seroquel);
- Alimemazine (teraligen);
- Sulpiride (eglonil).
The general sedative effect of these drugs allows, when taken continuously, to prevent the development of panic attacks, and when taken once, to relieve a panic attack.
The disadvantage of this group of drugs is that, in addition to anxiety, other emotional reactions (joy, surprise, delight, pleasure, curiosity, melancholy, etc.) can be suppressed.
Antidepressants with sedative effects
Despite the fact that antidepressants are the most prescribed pills in the complex treatment of panic attacks, they can also be used as an “ambulance” - once to stop a panic attack. For this purpose the following are most often used:
- Amitriptyline;
- Clomipramine (Anafranil);
- Mianserin (lerivon)
Unlike antipsychotics and tranquilizers, the effect of antidepressants does not develop as quickly, but is longer lasting.
Other drugs for quick relief of an attack
- aminophenylbutyric acid (phenibut),
- glycine,
- ethyl alcohol (alcohol),
- valocordin or corvalol (and their analogues),
- beta-blockers (anaprilin, atenolol),
- alpha-blockers (clinidine), etc.