Types of iron-containing drugs
Pharmacological companies offer a wide range of medicines and dietary supplements containing iron. The first group is prescribed for treatment, since the medications have a higher dosage of the main active ingredients. Supplements are used to prevent iron deficiency and maintain it within normal limits.
Main types:
- Iron tablets. Medicines contain ferrous iron in the form of ferrous gluconate or ferrous sulfate. The second substance has a little more iron, but the difference is smoothed out by selecting the dosage. The effectiveness of both substances is approximately the same. Iron tablets should not be prescribed to yourself, as they are used to treat confirmed anemia. Medicines have side effects and contraindications, but they are fast-acting and easy to digest. If you take the tablets for 14-28 days, you can significantly improve your hemoglobin level.
- Iron in vitamin complexes. Multivitamins can help with mild anemia, but are not suitable for treating severe conditions. In pharmacies you can buy complex preparations with ferric iron. The substance is less digestible, but easier to tolerate. To achieve an effect, the duration of use should be from two to three months. The effect of taking iron as part of vitamin complexes is enhanced by the presence of other minerals and vitamins - ascorbic and folic acids, vitamin B12, copper, manganese.
- Biologically active additives. Vitamins can also be classified as dietary supplements. However, dietary supplements with iron may contain extracts of medicinal herbs, as well as vitamin compounds. To increase vitality, supplements may contain eleutherococcus or ginseng extract. A permanent or course treatment is indicated.
In what forms are iron supplements available?
For ease of use by both adults and children, manufacturers produce medications in different forms.
For oral administration we offer:
- pills. The main active ingredients are gradually released in the stomach, the tablets do not irritate the mucous membrane. Pros: the effect is independent of food intake, you can take it with you, it’s convenient to take. The downside is that iron from tablets has lower absorption compared to other forms. It is better to find out from your doctor which iron tablets are best to choose;
- syrups. Suitable for babies and older children. The viscous consistency promotes envelopment of the stomach walls and rapid and complete absorption. Disadvantages - they may have an unpleasant taste, and with a high iron content they can stain teeth. Contains sugar and is not suitable for people with diabetes;
- capsules. They are convenient for adults to take, but dissolution in the stomach can cause discomfort. The capsule is indivisible and is not suitable for use by small children.
- hematogen. Can be used by children and adults, has a pleasant taste and is well absorbed. Abuse must be avoided and age-specific dosages must be observed.
Iron is also available in the form of chewable tablets, drops, and powders for preparing solutions.
In a hospital setting, treatment can be carried out by injection into a vein, into a muscle, or using systems using iron-containing solutions. The choice in favor of parenteral administration is made in situations that threaten the patient’s life, as well as when it is impossible or ineffective to use drugs for oral administration.
Development of anemia
Over time, iron deficiency progresses, flows latently for many years, and then, after complete depletion of iron stores in the depot, IDA develops. The main mechanism for the development of anemia is a violation of hemoglobin formation in erythrokaryocytes of the bone marrow. The pathology of erythropoiesis in iron deficiency is based on a violation of heme synthesis, as a result of which the hemoglobinization of erythronormoblasts is delayed compared to the process of reverse development of nuclear structures. Since hemoglobin synthesis suffers to a greater extent due to iron deficiency than the formation of red blood cells, IDA, with a relatively moderate decrease in the number of red blood cells, is characterized by a more pronounced drop in the hemoglobin content in them, which is manifested by hypochromia of red blood cells and the development of hypochromic microcytic anemia.
The second pathological mechanism that occurs under conditions of iron deficiency is a decrease in the formation of other important proteins involved in the accumulation and transport of oxygen. The myoglobin content in striated muscles decreases. Violation of the formation of cytochromes and catalases leads to inhibition of the energy metabolism of all cells of the body, while rapidly dividing tissues (skin and mucous membranes) are mainly affected.
Depending on the causes of iron deficiency, five groups of IDA are distinguished:
1) chronic posthemorrhagic IDA;
2) IDA associated with impaired absorption and intake of iron from food;
3) IDA associated with insufficient initial levels of iron in the body (more often in children);
4) IDA, caused by an increase in the body's need for iron (without blood loss);
5) IDA associated with impaired iron transport.
Symptoms of anemia include:
- muscle weakness not corresponding to the degree of anemia;
- perversion of taste, in the form of a desire to eat inedible substances (chalk, coal, clay), raw foods, cereals, dough, raw minced meat), as well as an addiction to unusual odors (kerosene, fuel oil, gasoline, acetone, shoe polish, naphthalene, exhaust gases) cars);
- hair loss and dry skin with the formation of cracks, especially often in the corners of the mouth (angular stomatitis);
- changes in nails: fragility, appearance of striations, concavity (koilonychia);
- soreness and focal redness of the tongue mucosa with atrophy of the papillae (“geographic tongue”);
- dysphagia, characterized by difficulty swallowing dry food and the development of painful spasms of the esophagus (Plummer-Wilson syndrome);
- dysuric disorders (urinary incontinence, nocturnal enuresis).
Review of drugs for anemia
Pharmacies offer a wide range of medicines that increase hemoglobin. The most frequently prescribed by doctors are:
- Fenyuls in capsules. Indicated for regular blood loss, to replenish iron deficiency. Contains B vitamins and ascorbic acid. You can buy capsules inexpensively in the online store. The price for a pack of 30 pieces starts from 250 rubles;
- Ferrum-Lek in the form of chewable tablets, syrup, solution for intramuscular administration. Intended for the treatment of hidden iron deficiency, the treatment of anemia, and is suitable for preventing the development of anemia in pregnant women. The syrup is allowed for small children. You can reserve medications on the store’s website. Information about prices, promotions, discounts and available drugs is also available there;
- Maltofer in drops, tablets, syrup, solution for intramuscular administration. In the form of drops, it is used to treat anemia in newborns and premature babies. Tablets are allowed from 12 years of age;
- Ferretab capsules. They have a prolonged effect and contain folic acid. Suitable for pregnant women. One capsule per day is enough. The cost of 30 pieces starts from 380 rubles. You can quickly order and pay for your purchase directly on the website at a time convenient for you.
- Sorbifer Durules tablets. It is prescribed for anemia and iron deficiency, and is also indicated for preventive purposes for pregnant, lactating women and donors. Can be used in children from 12 years of age. For prevention, one tablet per day is enough. Additionally contains ascorbic acid.
The choice of an iron-containing drug should be entrusted to a doctor, who will prescribe a blood test and, based on the results, choose the appropriate medication.
Treatment of iron deficiency anemia and iron deficiency
27.05.2021
Treatment of iron deficiency anemia and iron deficiency
About modern ideas about the correction of iron deficiency and the main characteristics of iron-containing drugs, the principles of their selection and dosage in iron deficiency states. Diet for iron deficiency and sources of iron in food
The main source of iron for humans is animal products. In nature, iron exists in two chemical forms: 2-valent (heme) and 3-valent (non-heme). Heme iron is well absorbed in the intestine. The richest meats in heme iron are beef, especially beef and blood sausage. There is much less heme iron in poultry and fish. Liver (pork and veal), kidneys, heart, liver sausage are rich in ferritin and hemosiderin, containing non-heme iron (the latter is poorly absorbed in the gastrointestinal tract). A lot of non-heme iron is found in some brands of red wine, fruit juices, apples, pomegranates, buckwheat, dairy products, eggs, nuts and chocolate. The bioavailability of such iron is minimal, and all these products are not a source of iron. Vegetarianism is a strong risk factor for iron deficiency anemia (IDA) at any age. At the same time, the diet should include greens, vegetables, and fruits, since iron absorption improves with the presence of vitamin C in food. Iron absorption is impaired by tannin (found in tea and coffee), phytin (found in rice, soy flour), milk and cottage cheese due to its high calcium content. Since the absorption of iron from food is limited, drug therapy for anemia is the mainstay.
The World Health Organization (WHO) conducted a global study between 1993 and 2005, which showed that 24.4% of all inhabitants of the globe suffer from various forms of anemia. Anemia most often occurs in preschool children (47% of the general population), pregnant women (41.8%) and non-pregnant women of childbearing age (30.2%). In the structure of anemia: 37% is iron deficiency anemia, 27% is anemia due to chronic diseases (CD).
Among women of fertile age, iron deficiency anemia (IDA) occupies a leading position. Anemic syndrome is the most common hematological syndrome encountered in clinical practice. Anemia is not a diagnosis, but only a syndrome that requires a special differential diagnostic algorithm.
WHO research indicates that IDA is the third most common cause of temporary disability in women aged 15–44 years. Along with IDA itself, there is a hidden iron deficiency, which in Europe and Russia is 30–40%, in some regions – 50–60%. According to WHO, iron deficiency is determined in 20–25% of all infants, 43% in children under 4 years of age and up to 50% in adolescents (girls). Thus, the most common anemias both in Belarus and in other countries are IDA and ACD. Anemia is a leading factor in the deterioration of a patient’s well-being; according to rough estimates, it affects 2.4 billion of the world’s population.
The main reasons for the development of iron deficiency anemia are: blood loss (heavy menstrual bleeding, pregnancy, childbirth, gastrointestinal, pulmonary, kidney disease); iron absorption disorders (resection of the stomach and intestines, pancreatic insufficiency, celiac enteropathy, Crohn's disease); increased need for iron (rapid growth, premature babies, newborns, adolescents, pregnancy and lactation); insufficient dietary intake (vegetarian or vegan diet).
It must be remembered that IDA is the final stage of severe iron deficiency, in which erythropoiesis (hematopoiesis) decreases and, as a result, the hemoglobin content decreases.
There are three stages of iron deficiency:
- prelatent;
- latent;
- manifest.
Prelatent iron deficiency is characterized by a decrease in microelement reserves without a decrease in iron consumption for erythropoiesis. Latent iron deficiency is observed when the microelement reserves in the depot are completely depleted, but there are no signs of the development of anemia. Manifest iron deficiency, or iron deficiency anemia (IDA), occurs when the hemoglobin pool of iron decreases and has characteristic symptoms. A decrease in serum ferritin concentration below 12 μg/L in healthy children and 15 μg/L in adults, adjusted below 30 μg/L in children and 70 μg/L in adults with infectious or inflammatory diseases, means an inevitable decrease in hemoglobin concentration in the future.
Treatment of iron deficiency anemia. The principles of treatment of IDA include the following:
- the effect cannot be achieved with diet alone;
- Iron supplements are prescribed mainly orally, before meals;
- An improvement in the general blood test does not mean that the body’s iron supply has been restored;
- After normalization of hemoglobin levels, iron intake should be continued for another 1–2 months. with a reduction in the daily dose by half to fill the depot.
The basis of pathogenetic therapy for IDA is the use of iron supplements orally. Treatment with iron supplements should be long-term and depend on the initial severity of anemia (hemoglobin level and iron deficiency).
At the outpatient stage, treatment is carried out when the hemoglobin level is >80 g/l and the patient’s general condition is satisfactory. Oral administration of iron-containing drugs at a dose of 200-300 mg/day for 4-6 weeks until hemoglobin levels normalize, after which the drug continues at a dose of 100 mg/day for 2-3 months until the ferritin level is at least 40 μg/l. It is necessary to find the cause of iron deficiency and eliminate the cause of iron deficiency - this is treatment of the underlying disease that caused iron deficiency.
Principles for choosing an iron supplement for therapy
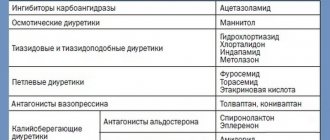
Currently, oral iron preparations are divided into two main groups: ionic and nonionic (the latter are represented by the protein and hydroxypolymaltose complex of ferrous iron).
Ionic preparations are represented by salts of 2-valent iron, including iron sulfate (ferrofol, tardiferon, ferroplex, sorbifer, ferro-foil, etc.); ferric chloride (hemofer); polysaccharide compounds - gluconate-fumarate combinations (heferol, ferronal, megaferrin). Ferrous chelates (citrate, lactate, gluconate, succinate) are better absorbed than ferrous sulfate. In case of intolerance to salt preparations of ferrous iron, which are currently the most effective in treating anemia and replenishing iron depots, it is possible to use nonionic preparations of ferrous iron in the form of a hydroxypolymaltose complex (maltofer, biofer, ferrum lek, etc.).
When choosing a drug and the optimal dosage regimen, it is necessary to remember that an adequate increase in hemoglobin levels in IDA can be ensured by the intake of 30 to 100 mg of ferrous iron into the body. Considering that with the development of IDA, iron absorption increases by 25–30% (with normal iron reserves in the body - only 3–7%), 100 to 300 mg of ferrous iron per day is prescribed. The use of higher doses does not make sense, since iron absorption does not increase. The degree of absorption of 2-valent iron salts is several times higher than that of 3-valent iron, therefore preparations containing 2-valent iron give a quick effect and normalize hemoglobin levels on average after 1–2 months, and normalization of iron levels in the depot occurs after 3 –4 months from the start of treatment and depends on the severity of anemia and the dose of the drug. Longer use of drugs containing iron in the 3-valent state is required; in case of copper deficiency in the body, they will be ineffective. Normalization of hemoglobin levels during treatment with a ferric iron preparation will occur only after 2–4 months, and replenishment of iron deficiency in the depot will occur after 5–7 months from the start of therapy. The degree of absorption is also reflected in the incidence of side effects. The undesirable effect of solid forms of iron preparations (tablets, capsules) on the gastrointestinal mucosa can be reduced by taking them with meals, but this reduces the absorption of iron.
When taking the drugs in a sufficient dose, an increase in the number of reticulocytes is observed on the 7-10th day from the start of treatment. Normalization of hemoglobin levels is observed after 3–4 weeks from the start of treatment, and in some cases it lasts up to 6–8 weeks. The total duration of treatment depends on the initial severity of anemia. Standard terms for ferrotherapy of IDA: for mild severity - 4-6 weeks, for moderate severity - 8-12 weeks, for severe severity - 16 weeks or more. When using ferrotherapy drugs internally, nausea, vomiting, anorexia, constipation most often occur (since iron binds hydrogen sulfide, which is a physiological stimulant of motility), less often - diarrhea, a metallic taste in the mouth, staining of the mucous membranes and teeth black, allergic reactions , headache. These side effects lead to frequent refusal of treatment by patients.
The bioavailability of divalent iron salts is several times higher than that of trivalent iron salts, since they diffuse freely through the channels of DMT1 proteins and ferroportin. The pharmacological effect of the drugs is rapid, and normalization of hemoglobin levels occurs on average after 2 weeks - 2 months, and replenishment of iron stores occurs within 3-4 months from the start of treatment, depending on the severity of anemia and the dosage of the drug. Therefore, WHO recommends ferrous iron preparations as initial therapy for iron deficiency anemia. The absorption of ions from ferric iron preparations is slower, since active (energy-dependent) transformation with the participation of ferrooxidases is required. Therefore, such drugs require longer use, and in case of copper deficiency in the body they will not be effective at all.
The medicinal product Ferrofol produced by Minskintercaps Unitary Enterprise
contains in one capsule 50 mg of iron (II) sulfate and 500 mcg of folic acid.
Using Ferrofol in an average daily dosage of 1 capsule 2-3 times a day 1 hour before meals (100-150 mg per day), the goal of treating iron deficiency anemia is achieved - the introduction of iron in the amount necessary to normalize hemoglobin levels, complies with WHO recommendations on optimal therapeutic dose. The drug Ferrofol meets the basic requirements for treatment with iron supplements:
- sufficient elemental iron content in the preparation;
- the use of ferrous sulfate, which provides the greatest bioavailability;
- administration of folic acid, which plays an important role in hematopoiesis, with an iron supplement; the lack of these vitamins causes a disruption of DNA synthesis in hematopoietic cells, which negatively affects the rate of hemoglobin synthesis.
Advantages of the drug Ferrofol:
is produced in the form of long-acting capsules, the active ingredients are contained in pellets (microgranules), which ensure their absorption in the upper part of the small intestine, and therefore there is no local irritant effect on the gastric mucosa, which ensures good gastrointestinal tolerability. The use of pellets in Ferrofol capsules allows you to isolate the active substances from each other - folic acid and iron in one finished form. Folic acid increases DNA synthesis in hematopoietic cells, which has a positive effect on the rate of hemoglobin synthesis, which means faster relief of anemia.
The drug Ferrofol is indicated for the prevention of latent iron deficiency and iron deficiency anemia, especially during pregnancy.
Prevention of iron deficiency anemia and latent iron deficiency is indicated for patients at risk, which include:
- pregnant women and during lactation;
- women with an interval between pregnancies of less than 2 years;
- ongoing or recurrent bleeding of a person with hereditary hemorrhagic hemostasiopathies;
- persons with chronic kidney disease with established iron deficiency;
- persons with blood ferritin levels less than 30 mcg/l (tissue iron deficiency);
- women with menstruation lasting more than 5 days.
Ferrofol is a combination drug that replenishes the deficiency of iron and folic acid in the body.
Capsules should be swallowed whole with a glass of water. The capsule must not be dissolved, chewed or kept in the mouth.
Administration is carried out before or during meals, depending on gastrointestinal tolerance.
There are medical contraindications and adverse reactions.
BEFORE USING THE MEDICINE, READ THE INSTRUCTIONS