One of the common congenital heart pathologies is the bicuspid aortic valve. Epidemiology shows that this defect occurs in almost 2% of the population and is usually detected in adulthood. In most cases, the bicuspid aortic valve operates without disruption of hemodynamics and does not cause problems in the functioning of the organ, but often for this reason an aneurysm (protrusion of the wall of an artery or heart cavity) or aortic stenosis develops.
Fact! According to statistics, in 75-80% of cases of aortic valve stenosis in children, the valve is bicuspid.
Briefly about the essence of the problem
A normal valve must have three well-moving leaflets that open and close at regular intervals to ensure the outflow of blood into the aorta. The valves are shaped like crescents. There are cases when disturbances occur during the intrauterine development of the fetus, which lead to fusion of two of the three valves and the appearance of a congenital heart defect (CHD) called a bicuspid aortic valve.
The formation of the cardiovascular system occurs in the period from the sixth to the eighth week, this is the most dangerous period, because negative factors can lead to disruption of the formation of various organ elements and blood vessels. That is why doctors strongly recommend that pregnant women in the first trimester be especially attentive to their health, give up all bad habits and avoid stress.
General information
Acquired defects can manifest themselves in different forms. By origin:
- due to rheumatism, which is a general inflammatory disease of connective tissue that affects the heart; Source: A.N. Kalyagin Features of management of patients with rheumatic heart defects and chronic heart failure // Modern Rheumatology, 2009, No. 3, pp. 24-29
- against the background of syphilis;
- due to an inflammatory process on the inner lining of the heart (endocarditis);
- and due to other systemic diseases leading to damage to the heart muscle or complications to it.
According to the degree of defect, the acquired defect can be:
- local (when the defect is only in 1 valve);
- combined (more than 1 valve is affected);
- combined (both stenosis and insufficiency are observed in one valve).
The defect may be a stenosis due to inflammation, which led to the formation of scars, prolapse (eversion of the valves into the heart cavity), or failure (valve valves do not close completely). In this case, different valves may be defective (aortic, tricuspid, mitral, located on the trunk of the pulmonary artery).
An acquired defect can be expressed in different ways; it has three degrees:
- mild (minor effect on blood circulation);
- moderate;
- heavy.
This group of pathologies entails a number of complications:
- heart failure;
- heart rhythm disturbances;
- blood clots
If left untreated or not detected early, heart disease can lead to disability and even death.
Signs of a cardiac abnormality
Very often, the defect - bicuspid aortic valve in children - occurs without symptoms, it is not suspected for decades, but the older a person gets, they more often show signs of an anomaly.
Typical symptoms include the following:
- the appearance of shortness of breath, which increases significantly after physical exertion. Over time, shortness of breath begins to appear even with light exertion;
- strong pulsation in the head;
- frequent tachycardia (many patients mistake it for palpitations);
- pain in the cardiac region (they are the result of ventricular hypertrophy).
A special symptom that characterizes a congenital heart defect called bicuspid aortic valve is a violation of blood flow in which reverse movement occurs, i.e. blood leaves the aorta back into the ventricle. This manifestation of a defect in a patient can only be identified by a specialist conducting an examination, but it is for this reason that other signs appear.
Degrees of heart defects in a child
Depending on the severity of the symptoms of heart disease, there are four degrees of impairment:
- first degree
- heart function deviates slightly from the norm; - second degree
- symptoms of the disease appear, parents can notice them; - third degree
- in addition to specific symptoms, disturbances in the functioning of the nervous system appear, as a result of a lack of oxygen to the brain; - fourth degree
- respiratory and cardiac activity is inhibited, such changes can lead to the death of the child.
Causes of the phenomenon
As the main reason for the development of this defect, doctors call the impact of harmful and dangerous factors on the body of a pregnant woman during the formation of elements of the cardiovascular system. This may be radiation exposure, x-ray exposure, infection, poor ecology and other mutagens.
The next factor is a woman’s smoking during pregnancy. Nicotine has a negative effect on the formation of any organs during fetal development.
It affects the development of the bicuspid aortic valve and heredity, it is transmitted from one of the parents. Therefore, doctors strongly recommend that those parents who have this anomaly conduct a full examination of the child immediately after birth in order to take the necessary measures and carry out therapy in a timely manner.
Types of heart defects
| Type | Name |
| Congenital | |
| Without the development of cyanosis (pale type) | Defects of the interventricular and interatrial septa |
| Patent ductus arteriosus | |
| Pulmonary stenosis | |
| Coarctation of the aorta | |
| With the development of cyanosis (blue) | Transposition of the great vessels |
| Common ventricle | |
| Tetralogy of Fallot | |
| Purchased | |
| Mitral valve (between the left atrium and ventricle) | Mitral stenosis |
| Mitral regurgitation | |
| Tricuspid valve (between the right atrium and ventricle) | Tricuspid valve stenosis |
| Tricuspid valve insufficiency | |
| Aortic valve (between the left ventricle and the aorta) | Aortic stenosis |
| Aortic insufficiency | |
| Pulmonary valve | Pulmonary valve stenosis |
| Pulmonary valve insufficiency | |
Stenosis
- narrowing of the valve opening, which causes difficulty in blood flow.
Failure
- inability of the valves to close tightly. In people with valve stenosis, valve insufficiency develops over time - this is called combined PS.
Septal disorders:
A condition in which the septum between the chambers of the heart is damaged:
- atrial septum -
“extra” blood enters the right atrium and causes it to enlarge; - interventricular
- blood flows from the right to the left ventricle, expanding its boundaries.
Changes are found in 2 out of 1000 newborns. Perhaps the most favorable form, since small defects can heal on their own.
Coarctation of the aorta:
Narrowing of the lumen of the main vessel in the area of the isthmus - the transition of the arch to the descending part. The defect causes disruption of the blood supply to organs. This form of pathology accounts for 10% of all defects. Often combined with disruption of interchamber septa. A serious condition requiring medical attention immediately after birth.
Pulmonary valve stenosis:
At the site of the valves from the right ventricle to the pulmonary artery, a narrowing occurs. The heart requires more effort to pump blood. 10% of the total number of defects.
Transposition of the great vessels:
Rare pathology (about 5%). In this case, the main vessels “change places.” Arterial blood flows through the veins, and venous blood through the arteries.
Tetralogy of Fallot:
The most severe form. Consists of four violations simultaneously:
- the opening between the left and right ventricles;
- pulmonary stenosis – narrowing of the pulmonary trunk;
- enlargement of the right ventricle;
- Aortic displacement is the exit of the aorta from the heart in an atypical location.
Diagnostic examination methods
If any signs indicating problems with the heart appear, an examination by a cardiologist is immediately required. In addition to collecting anamnesis, the doctor prescribes the necessary types of hardware diagnostics.
The very first method that will reveal the presence of congenital heart disease in the form of a bicuspid aortic valve is echocardiography (a type of ultrasound (you can watch it on video), which allows you to identify not only the presence of an anomaly, but also the degree of regurgitation).
In addition, diagnostics may include:
- radiography;
- electrocardiogram;
- Doppler study;
- cardiac catheterization.
Diagnosis of acquired defect
The most important thing in diagnosis is taking an anamnesis. The doctor analyzes past and existing diseases, their severity, characteristics of the course, and the effectiveness of the therapy. The child’s complaints are examined with close attention, and the specialist asks about injuries in the chest area. The child’s parents are always asked about heart disease or pathologies in someone in the family, about cases of heart defects.
The child is examined. Using a stethoscope, murmurs and pulmonary wheezing are detected. The doctor measures blood pressure and taps to determine the boundaries of the heart and, accordingly, its size.
Knowing the type of murmur can help preliminarily determine the type of heart defect.
Based on a comprehensive history and examination, the patient may be prescribed various laboratory and instrumental tests.
- Determination of liver size.
- General urine analysis.
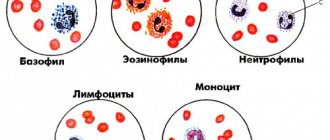
- Clinical blood test.
- Blood chemistry.
- FKG.
- ECG.
- ECHO-KG.
- .
- X-ray with contrast.
- MRI. Source: R.K. Georgikia, G.I. Kharitonov Modern aspects of diagnosis and treatment of acquired heart defects // Kazan branch of Apteka-Holding CJSC, 2003, No. 2, pp. 25-26
Treatment of diseases
If a bicuspid aortic valve is detected with grade 1 insufficiency, and it does not show any signs and does not affect the patient’s quality of life, does not interfere with physical activity, then the defect can be left for some time without surgical intervention. However, the patient must undergo periodic examinations, ultrasound scans and avoid overloading the heart. However, with age, surgery will still be indicated.
A bicuspid aortic valve requires surgical intervention, which involves:
- prosthetics (replacement with a biological or mechanical prosthesis);
- transcatheter implantation of valve prosthesis (modern method of percutaneous implantation).
Treatment Options
The severity of the symptoms of the disease entirely determines the treatment tactics. If before the examination the patient did not have any health problems, the body was subjected to intense physical activity, no specific therapy is required. However, after confirming the diagnosis, the doctor must register him with a dispensary, which obliges him to take a series of tests several times a year.
A different approach is required by a severe form of pathology. The patient is indicated for surgery with installation of an aortic valve prosthesis. Surgical intervention does not involve open manipulation of the chest. Modern techniques allow the installation of a prosthesis through the skin. The implant is inserted through the subclavian or femoral artery. After the operation, the patient is prescribed constant medication to reduce blood clotting.
Patient prognosis and recommendations
Now, about how long the patient will live after he is diagnosed with “Bivalve aortic valve”, the prognosis will depend on the rate of changes in the functioning of the organ caused by the presence of the defect, and on whether there is a manifestation of heart or coronary insufficiency.
If no serious destructive problems are found, then ten years may pass from the moment of diagnosis, but if destruction occurs and the presence of a defect affects the functioning of the organ, then the forecasts do not exceed two years.
Attention! This defect requires constant monitoring and observation by specialists, and clinical manifestations indicate the need for immediate treatment in a specialized clinic.
Even if the functional bicuspid valve does not affect the rhythm of life, doctors recommend avoiding nervous strain, trying to avoid stress, maintaining a work-rest schedule, eating more vitamins (in the form of vegetables and fruits) and be sure to take daily walks in the fresh air. Prevention should be aimed at protecting against infections such as endocarditis, and it also helps against sclerosis.
As for the question: bicuspid aortic valve and sports, it should be resolved individually in consultation with a doctor.
Aortic valve disease: features of its course and treatment
According to statistics, disorders of the cardiovascular system have become increasingly observed in people over 30 years of age. There are many reasons that provoke pathologies. If some diseases are treatable and, by removing provoking factors, one can achieve normalization of health, then others accompany the patient throughout his life and can significantly shorten his life.
Aortic valve disease is a serious pathology. More often requires surgical intervention. It can be congenital or acquired. Appears as a result of narrowing of the aortic mouth or incomplete closure of its valve.
Causes and symptoms
There are no exact statistics on the prevalence of the disease by age group and gender, but cardiologists note that it is detected several times more often in women than in men. The peak number of patients is observed among people of older retirement age. The main reasons may be:
- leaflet calcification;
- progression of rheumatism;
- idiopathic dilatation of the aorta;
- arterial hypertension and endocarditis;
- aneurysm;
- congenital defect of the aortic valve.
Chest trauma, arthritis, syphilis and some pathologies that develop in a person over a long period of time can also give impetus to the appearance or progression of disruption of the normal functioning of the organ.
8
24/7
Degrees
The risk to the patient's health and the need for surgery depends on the degree of aortic regurgitation.
| Stage | Amount of thrown blood, % | Prosthetics |
| First, full compensation | no more than 15 | Not required |
| Second, hidden CH | from 15 to 30 | Required under certain conditions |
| Third, relative coronary insufficiency | up to 50 | |
| Fourth, severe left ventricular failure | more than 50 | |
| The issue is resolved individually | Not required due to its uselessness. |
Depending on the degree, the valves are deformed and the quantitative volume of blood entering the heart through the aorta changes. The initial, first stage of the disease is virtually impossible to determine. The patient’s symptoms are completely absent or feel like side effects of other diseases. This occurs because the heart adjusts to the change in volume and compensates for it.
Symptoms
As the pathology develops, the organ ceases to cope with its functions, and symptoms characteristic of aortic valve disease appear:
- tinnitus and dizziness when moving or changing position;
- increased heartbeat, pronounced pulsation in the blood vessels;
- shortness of breath, fatigue, fainting and pre-fainting states, nausea;
- a pressing feeling of heaviness in the right hypochondrium, as well as swelling of the lower extremities;
- coughing attacks when lying down, standing, feeling of constant weakness.
Due to a lack of oxygen, a person’s complexion becomes pale gray, a bluish tint to the lips is observed, and typical circles appear under the eyes. Also, when examining a patient, the cardiologist examines the presence and severity of symptoms:
- the difference between the upper and lower blood pressure readings;
- pulsation on the carotid arteries, uvula and tonsils;
- reaction of the pupils to heart contractions, heart murmurs;
- changes in the size of the organ, protrusion in the chest area.
Diagnostics
Accurate diagnosis of the disease can only be made on the basis of objective data, a complete cardiac examination, biochemical blood test and a number of other tests.
Based on the presence of clinical symptoms, the severity of the defect, and the severity of aortic insufficiency, a decision about surgery is made. In elderly patients, due to the low contractility of the organ, the functional impairment is almost invisible. The severity of the pathology can be determined after studying the area of the hole in relation to the blood flow. Arterial insufficiency is determined by the indicator of reverse blood flow.
By listening, a cardiologist can determine the onset of development of bicuspid aortic valve disease:
- with stenosis, a systolic murmur is characteristic with a weakening of the 2nd tone in the aorta;
- Insufficiency is indicated by a murmur during diastole.
It is necessary to study the functioning of the heart by:
- ECG;
- X-ray examination;
- MRI to exclude coronary insufficiency and other pathologies.
However, the basis for choosing treatment is echocardiography.
When diagnosing, an accurate description of the patient’s feelings is of great importance, so before the appointment, you can write down all the complaints and let the doctor read them.
8
24/7
Treatment at different stages
Depending on the cause, extent, stage of aortic valve disease and other factors, different treatment methods may be used. The patient must be regularly observed by a specialist and undergo the examinations prescribed by him. In the absence of obvious symptoms:
- mild defect – once every 3 years;
- moderate form – once every 24 months;
- severe degree - annually, sometimes more often.
The following medications are prescribed:
- rheumatic nature of the disease - antibiotics;
- arterial hypertension - to normalize blood pressure.
Surgical intervention is not required, only constant monitoring by the attending physician is required.
If clinical complaints appear, to alleviate the patient’s condition in the preoperative period or if surgery is impossible, the following is prescribed:
- inhibitors, diuretics, nitrates;
- vasodilators and beta blockers;
- drugs that improve blood circulation.
A timely operation can help completely get rid of aortic valve disease. When blood reflux in an amount not exceeding 30% and slight deformation of the valves, intra-aortic balloon counterpulsation is recommended. In case of severe structural changes that allow more than 30% blood flow, implantation is required.
Surgery
In a person with heart disease, the bicuspid aortic valve requires replacement or replacement in several cases.
| Diagnosis | Cause |
| Severe stenosis | Complaints of severe pain and worsening condition. |
| Associated ischemia requiring coronary artery bypass grafting. | |
| Additional pathological changes in the organ requiring surgical intervention. | |
| The ejection fraction with cardiac contractility is below 50%. | |
| Severe valvular insufficiency | Clinical manifestations of the disease. |
| Surgery is required for other diseases of the organ. | |
| A decrease in ejection fraction in the absence of complaints from the patient. | |
| Too much enlargement of the ventricles. |
Surgical intervention is mainly performed after 30-35 years, but with the accelerated development of the disease it can take place at any time. The number of contraindications to prosthetics is minimal. They are:
- decompensated diabetes;
- oncological diseases;
- post-stroke condition;
- exhaustion and anemia.
For each patient, his condition is predicted at the time of the operation and during the rehabilitation period. Depending on this, a conclusion is given about the possibility of returning to normal life.
Forecast
The construction of treatment plans for the disease and the choice of methods occurs after diagnosis and identification of the severity of the aortic valve defect.
Mild hypertrophy with strong obstruction of blood flow leads to a decrease in the number of heart contractions and, accordingly, gradually reduces the therapeutic effect of surgery.
The process of hypertrophy allows, at a certain stage of the disease, to stabilize the functioning of the heart, but at the same time it can cause the development of angina pectoris and increase the likelihood of a heart attack.
If aortic heart valve disease developed asymptomatically, and then its rapid progression began, then the subsequent life expectancy of a person is no more than 3 years.
Risk factors and disease prevention
Aortic valve defects can be divided into 2 groups.
| View | Development time | Cause |
| Congenital | During intrauterine development of the fetus at 2-8 weeks of formation. | Genetic predisposition. Radiation exposure, rubella and other viral infections. Smoking, alcohol and drug addiction of the mother. |
| The defect becomes noticeable as the child grows. | The presence of a muscle cushion above the AC. The valve design is two- or single-leaf rather than three-leaf. Under the valve there is a membrane with a hole. | |
| Acquired | Any age | Infectious diseases that lead to microorganisms entering the organ. The subsequent appearance of a colony of connective tissue at the site of localization leads to deformation of the valves. |
| Autoimmune diseases become an impetus for the fusion of pouches and changes in the aortic mouth. | ||
| Age-related disorders, mainly calcification of the edges of the valves and the growth of fatty plaques, lead to closure of the lumen. |
There are no preventive measures that guarantee complete protection against the disease, but the following help reduce the risk:
- timely treatment of streptococcal infections;
- if you have rheumatism, constant monitoring by a specialist;
- taking certain groups of antibiotics and other drugs prescribed by a cardiologist;
- complete exclusion of alcohol, drugs and smoking;
- engaging in acceptable forms of exercise.
Aortic valve disease needs to be treated using scientific methods of therapy. Traditional methods do not have the desired effect and can lead to missed deadlines when the disease can be cured. Therefore, in case of any deviations, medical attention is needed.
8
24/7