Local therapist
Ablyazov
Irshat Ravilevich
21 years of experience
Local therapist of the highest category. Member of the Russian Scientific Medical Society of Therapists.
Make an appointment
Thrombocytopenia is a separate disease or a symptom of another disease that is characterized by a low platelet count (less than 150,000 units per microliter). The condition is accompanied by high bleeding, as well as slow stopping of bleeding from small vessels.
Symptoms
Symptoms of thrombocytopenia include:
- Purpura. This is the name for hemorrhages in mucous tissues or skin. In fact, it looks like red spots - most often they can be seen in places of strong contact with clothing. The spots do not hurt, they can be pinpoint or quite extensive - including bruises of different colors (depending on the time of formation).
- Regular nosebleeds. Since small vessels are weakened, bleeding can begin due to a cold, sneezing, or minor injury. Bright red blood may flow for ten minutes or more, putting the patient at risk of losing a lot of blood.
- Bleeding gums, prolonged bleeding after tooth extraction. The mechanism is the same: due to weak blood vessels, the blood cannot stop quickly in case of small or large injuries.
- Bleeding of internal organs. For example, blood is found in the gastrointestinal tract, when the stool becomes colored, or in the genitourinary system - then the urine becomes colored. Both symptoms are very alarming and require immediate contact with specialists.
- Too heavy and long menstruation. Moreover, bleeding can be observed on other days of the cycle.
All of these symptoms may indicate other diseases - both concomitant with thrombocytopenia and independent. What complicates the situation is that there are a lot of reasons and mechanisms for the development of this condition. In medicine, there are several types of this disease.
References
- Battinelli E.M., Markens B.A. Italiano JE Release of angiogenesis regulatory proteins from platelet alpha granules: modulation of physiologic and pathologic angiogenesis Blood. 2011; 118(5): 1359–1369.
- Bourdon DM, Mahanty SK, Jacobson KA, Boyer JL, Harden TK (N)- methanocarba-2MeSADP (MRS2365) is a subtype-specific agonist that induces rapid desensitization of the P2Y1 receptor of human platelets/ J Thromb Haemost. 2006; 4(4): 861–868.
- Fisher M., Vasilevko V., Cribbs DH Mixed Cerebrovascular Disease and the Future of Stroke Prevention. Transl Stroke Res. 2012; 3(1): 39–51.
Classification of thrombocytopenia
Let's talk about the causes of thrombocytopenia that underlie the different types of this disease.
Hereditary thrombocytopenias
These conditions are based on diseases of genetic origin. These may be May-Hegglin anomaly, Bernard-Soulier syndrome, Wiskott-Aldrich syndrome, TAR syndrome, as well as congenital amegakaryocytic thrombocytopenia.
Each of these diseases has many characteristics. For example, Wiskott-Aldrich syndrome occurs exclusively in boys and occurs in four to ten cases per million. Bernard-Soulier syndrome can only develop in a baby who has received the altered gene from both parents, and May-Hegglin anomaly can develop in 50% of cases, provided that only one parent has the prerequisites for this. As a rule, all of these diseases have among their symptoms not only a low level of platelets, but also a number of other pathological conditions, and therefore require special treatment.
What are platelets responsible for in the body?
The site of platelet production is the bone marrow. They are produced from large megakaryocytes. Platelets are plate-shaped, oval or round in shape. The diameter of blood cells is 2-4 microns. Platelets can change from a circle to a spherical shape, forming protrusions on their outer membrane, which is possible due to the presence of receptors on their surface, the basis of which are glycoprotein complexes. With these outgrowths they connect to each other and to the vascular walls in the place where they are damaged. Fibrin threads allow platelets to attach to existing defects, after which these blood cells begin to secrete an enzyme called thrombostenin. Under its influence, the threads twist and become denser.
Platelets also produce enzymes responsible for normal blood clotting, as well as platelet fibrinogen, platelet growth factor, peroxidases, serotonin, immune complexes and other substances that play an important role in the normal functioning of the body.
So, platelets are necessary for a person to ensure his life, as they take part in many important processes, including:
- The formation of a blood clot, which is necessary to stop bleeding at the site of damage to small vessels.
- Maintaining vascular spasm.
- Nutrition of the vascular wall.
- Production of immune complexes.
- Dissolving blood clots.
Platelet levels over a 24-hour period may fluctuate within 10% of the normal level. If a woman is menstruating, then these fluctuations range from 20 to 50%. Therefore, when diagnosing thrombocytopenia, it is necessary that the platelet level be less than 100 * 10 9 / l.
- Platelets are elevated in an adult - what does this mean, and how to reduce them?
80% of people with low blood platelet levels experience nosebleeds. Pathology is also indicated by prolonged menstruation and increased bleeding of the gums.
On average, a new platelet lasts no more than 10 days. After this it becomes smaller. If the platelet size is less than 7.0 fl, then the person either recently had their spleen removed or suffers from Wiskott-Aldrich syndrome. This disease is accompanied not only by thrombocytopenia, but also by immunodeficiency and skin eczema. Therefore, during laboratory diagnostics, it is necessary to take into account the average size of blood platelets. This indicator is designated in the analysis results as MPV. Its normal values are 7.4-10.4 fl.
Productive thrombocytopenia
They are also caused by a huge list of reasons and factors of various origins. All of them are associated with the fact that platelet formation processes in the red bone marrow are disrupted.
For example, this includes some types of anemia, cancer metastases, acute leukemia, and taking cytostatic medications. There are even factors such as radiation or alcohol abuse.
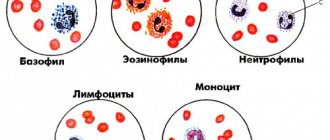
For example, in acute leukemia, a disease of the circulatory system causes a mutation in the bone marrow stem cell. Because of this, it divides and begins to displace hematopoietic cells. As a result, the number of not only platelets, but also leukocytes, erythrocytes, and lymphocytes decreases. This condition has its own name - pancytopenia. That is, immune thrombocytopenia in this case is part of it.
If we are talking about the effect of medications, then most often a decrease in platelet levels is caused by drugs from the following groups:
- antidiabetic,
- anti-inflammatory,
- antipsychotics,
- antithyroid,
- antibiotics,
- diuretics,
- anticonvulsants.
Of course, not all medications and not in all cases are capable of causing such a reaction, but this is another reason to think about the fact that you should not prescribe any medications yourself or take them without the supervision of your doctor.
Moreover, there is also such a factor as increased sensitivity to certain medications. Usually it is initially determined by a peculiar genetic predisposition, but this is quite rare.
When we talk about radiation, we are talking not only about a person’s presence in dangerous areas, but also about treatment with radiation therapy. When tumors are destroyed, the blood-forming cells of the red brain can be affected, so a condition where platelet levels drop can become a side effect of cancer treatment.
The development of symptoms of thrombocytopenia due to alcohol abuse most often occurs against the background of binge drinking and is associated with a high level of ethyl alcohol in the blood. It has negative and long-lasting effects on the bone marrow and usually causes a temporary decrease in platelets. If binge drinking becomes frequent and too long, there is a risk that the changes will be irreversible.
Causes
Platelets are formed elements of blood, nuclear-free flat plates ranging in size from 1 to 2 microns. They are formed from megakaryocytes (precursor cells) in the red bone marrow.
Megakaryocytes are relatively large cells. They have long processes and are almost completely filled with cytoplasm. During maturation, tiny fragments of their processes break off and enter the bloodstream. These are platelets. According to scientific data, from 2000 to 8000 platelets can be formed from one donor cell.
Thrombopoietin, a protein hormone produced in the kidneys, liver and muscles, is responsible for the development and growth of megakaryocytes. It is transported through the bloodstream to the red bone marrow, where it ensures the formation of megakaryocytes and platelets. The more platelets there are, the more the process of thrombopoietin formation is inhibited. This allows you to maintain the number of blood cells at the same level.
If any of these steps fail, the number of platelets in the peripheral blood decreases. Thrombocytopenia develops.
Taking into account the causes and mechanism of development, the disease comes in different forms:
- hereditary;
- productive;
- destruction;
- consumption;
- redistribution;
- breeding.
Hereditary thrombocytopenias
Hereditary thrombocytopenia is observed with various congenital anomalies. Its causes are genetic mutations:
- Wiskott-Aldrich syndrome. Caused by mutations that cause the red bone marrow to produce very small platelets (less than 1 µm in diameter). Due to their abnormal structure, they are quickly (within a few hours) destroyed in the spleen.
- May-Hegglin anomaly. A very rare genetic pathology, due to which the process of separating platelets from megakaryocytes is disrupted. As a result, the number of blood cells decreases, but their sizes become gigantic (6-7 microns). In parallel, there is a disturbance in the formation of leukocytes (leukopenia).
- Congenital amegakaryocytic thrombocytopenia. Typically, this form of thrombocytopenia is diagnosed in infants. It is associated with impaired platelet production by the bone marrow.
- Bernard-Soulier syndrome. Thrombocytopenia in a child appears only if he has inherited a defective gene from both his mother and father. The disease manifests itself in early childhood. It is characterized by the formation of functionally incompetent giant platelets (6-8 µm), unable to attach to damaged vascular walls and communicate with each other.
- TAR syndrome. A very rare cause of congenital thrombocytopenia, combined with the absence of both radius bones.
Productive thrombocytopenia
The group of productive thrombocytopenias includes pathologies of the hematopoietic system associated with disruption of the process of platelet formation in the red bone marrow. Causes of diseases:
- Acute leukemia. Stem cells mutate, and a large number of clones appear that are unable to perform specific functions. Gradually, clones displace hematopoietic ones from the red bone marrow. Not only the number of platelets decreases, but also the number of leukocytes, lymphocytes and erythrocytes.
- Myelodysplastic syndrome. The bone marrow cannot produce enough healthy cells. Hematopoietic cells multiply rapidly, but their maturation processes are disrupted. As a result, many functionally immature cells are formed (among them platelets) that undergo apoptosis (self-destruction).
- Aplastic anemia (the body produces very few new blood cells).
- Cancer metastases. Tumor cells in the final stages of cancer begin to leave the primary focus and spread throughout the body. Settling on tissues and organs, they begin to actively reproduce. This leads to the displacement of hematopoietic cells from the red bone marrow.
- Myelofibrosis. The stem cells mutate and the bone marrow is replaced by scar tissue. Foci of hematopoiesis develop in the liver and spleen (the size of the organs increases greatly due to this).
- Radiation. Ionizing radiation has a destructive effect on the hematopoietic cells of the red bone marrow. They begin to mutate.
- Alcoholism. Alcohol inhibits the processes of hematopoiesis in the red bone marrow, which reduces the content of platelets, leukocytes and red blood cells in the blood.
- Cytostatic drugs. Used to treat tumors. They can inhibit hematopoiesis in the bone marrow, which reduces the number of platelets.
- Allergic reactions to certain medications (diuretics, antibiotics, antipsychotics, anticonvulsants and anti-inflammatory drugs, antidiabetic drugs).
- Megaloblastic anemia. They develop with a deficiency of folic acid and vitamin B12.
Thrombocytopenia destruction
The cause of thrombocytopenia in this case is the increased destruction of platelets in the spleen (can also be in the lymph nodes, vascular bed or liver). Pathology is observed when:
- thrombocytopenia of newborns;
- Evans-Fisher syndrome;
- some viral diseases (viral thrombocytopenia);
- post-transfusion thrombocytopenia;
- taking medications (drug-induced thrombocytopenia);
- idiopathic thrombocytopenic purpura.
Thrombocytopenia of newborns
Occurs if there are antigens on the surface of children's platelets that are not on maternal platelets. Antibodies produced by the mother's body enter the newborn's bloodstream and destroy his platelets. The described process can last up to 20 weeks of intrauterine development. As a result, the child may be born with thrombocytopenia.
Fisher syndrome
It is a consequence of systemic diseases - autoimmune hepatitis, rheumatoid arthritis, systemic lupus erythematosus. Also, Evans-Fisher syndrome can develop against a background of relative well-being. Then they talk about idiopathic thrombocypenia.
Viral thrombocypenia
Once entering the body, viruses actively multiply. Antibodies are formed on the surface of the affected cells, and the cell's own antigens also change. The affected cells are destroyed in the spleen. Among the viruses that can cause thrombocypenia are measles, rubella, influenza, and chickenpox.
Post-transfusion thrombocytopenia
Post-transfusion thrombocytopenia is a consequence of platelet or blood transfusion. They are characterized by pronounced destruction of platelets in the spleen. The cause of the disease is that foreign platelets enter the body during a transfusion, to which antibodies begin to be produced.
Drug-induced thrombocytopenia
Some medications can bind to antigens on the surface of blood cells. Antibodies are produced to the formed complexes, which causes platelets to begin to be destroyed in the spleen. Among the “provoking” drugs are Quinidine, Meprobamate, Chloroquine, Ranitidine, Heparin, Cimetidine, Gentamicin, Ampicillin, etc.
Idiopathic thrombocytopenic purpura
Idiopathic thrombocytopenic purpura (also known as autoimmune thrombocytopenia or essential thrombocytopenia) is characterized by a sharp decrease in the level of platelets in the peripheral blood. At the same time, the composition of other blood elements is not disturbed.
Thrombocytopenia destruction
Here we are talking about the active destruction of platelets, which is usually observed in the spleen. Such processes are also caused by a large number of factors. These include taking certain medications, some viruses, Fisher-Evans syndrome, etc.
Idiopathic thrombocytopenia deserves special consideration. This is the case when it is not possible to establish the cause even with a huge number of possible options. At the same time, doctors note that even in such a situation, the action of provoking factors is observed. For example, the problem appears after bacterial and viral infections, preventive vaccinations, use of a number of medications, hypothermia or prolonged exposure to the sun.
This condition also occurs in newborns. It begins to form in the womb, when antibodies in her body cause the destruction of platelets in the child.
Fisher-Evans syndrome is also not an independent cause, since it itself is a consequence of various systemic diseases. This syndrome occurs in systemic lupus erythematosus and rheumatoid arthritis, but in some cases it can be an independent deviation. As for viruses, rubella, chicken pox, measles, and influenza can lead to a decrease in platelet levels. Sometimes this is a reaction to vaccination, although such a mechanism is described quite rarely and almost never occurs.
Activation
To perform their main function - repairing damage in the vessel wall - platelets must enter an active state. Like most cells in our body, this process proceeds according to the following scheme: signal - receptor - intracellular signal - amplifier - regulator - response (Fig. 3). The signal for activation is the appearance in the bloodstream of an agonist - a special signaling molecule, which should appear only when necessary and bind to a specific molecule that penetrates the platelet membrane (receptor). The agonist interacts with one “tail” of the receptor, protruding from the outside, and this leads to a change in the other, on the cytosol side, where the next signaling molecule, the secondary messenger, appears. It triggers the synthesis of several more messengers, which, in turn, triggers several more, and so the signal propagates in the cytosol and is amplified through a cascade of intracellular reactions, which ultimately leads to a complex platelet response. It is important that in the platelet there are special regulatory systems that modulate the concentrations of intracellular messengers at different stages of activation, so that, for example, there is no reaction to trace amounts of the agonist.
Rice. 3.
Platelet activation scheme
How is this scheme implemented in our body? In blood vessels, platelets are pushed out of the main flow by red blood cells and move along the walls, conducting a kind of monitoring of their condition. One of the first signals for platelet activation is collagen, the main protein of connective tissue, exposed when a vessel is damaged. Having detected collagen, they bind to it through special receptors, simultaneously becoming activated and firmly attaching to the site of damage. The interaction of a platelet with collagen leads to the launch of the mentioned intracellular signaling cascade and the appearance of a secondary messenger in the cytosol - inositol triphosphate (IP3). This small water-soluble molecule is able to move quickly in the cytosol and serves as a signal for the release of calcium ions from intracellular stores. And an increase in its intracellular concentration can lead to various responses of the platelet: splashing out the contents of granules (secretion), changing shape, attaching to the vessel wall (adhesion), bonding with other platelets (aggregation), and the appearance of procoagulant activity (Fig. 4). After the circulatory system has already recognized the damage to the vessel, three more natural platelet activators appear in the blood - thrombin, ADP and thromboxane A2. The thrombin protein is formed from its precursor, prothrombin, in the blood plasma, but in large quantities - already on the membranes of activated platelets. When their dense granules are secreted, large amounts of ADP (a small molecule that primarily performs energy functions in cells) are released, and much less ADP is released from damaged endothelial cells lining the inner surface of blood vessels. Thromboxane A2 is synthesized from arachidonic acid, located in the membranes of activated platelets. The binding of these three activators to their receptors on the platelet membrane leads, as in the case of collagen, to the appearance of IP3 in the cytosol and an increase in the calcium concentration in it (Fig. 4). Thus, all three soluble activators and collagen act through the same pathway, but induce different platelet responses. For example, thromboxane A2 provokes the release of dense granules, but ADP does not. Activation separately by collagen or thrombin causes all of the above responses simultaneously, and together leads to the appearance of a group of procoagulant platelets and the synthesis of thrombin on their membranes. Apparently, there are still insufficiently studied differences in the signaling triggered by different agonists. To prevent accidental activation from turning a platelet into a real “bomb”, carried in the bloodstream and triggering the entire coagulation system, intact endothelial cells in the body constantly secrete prostacyclin and nitric oxide, which block cell activation, preventing an increase in calcium concentration in them.
Rice. 4.
Scheme of the main pathways of platelet activation and its responses:
ADP
- adenosine diphosphate,
IP3
- inositol triphosphate,
ER
- endoplasmic reticulum
Signaling is one of the most complex and poorly understood areas in platelet research. There are many questions about the structure of each receptor and signaling pathway, and the simplest of them is: why are there so many activators at all?
Thrombocytopenia consumption
Here the mechanism is as follows: platelets, for some reason, begin to be activated in the vascular bed. In response to this, the red bone marrow begins to actively produce them - and as a result, its capabilities are slowly depleted. After this, the level of red cells begins to fall.
One of the causes of consumption thrombocytopenia is disseminated intravascular coagulation syndrome. It stands for disseminated intravascular coagulation syndrome. And it can develop against the background of severe tissue destruction during operations, burns, injuries, due to severe infections, chemotherapy, organ transplants, etc. That is, there are many underlying reasons that can cause a decrease in the level of platelets in the blood.
Introduction
It is generally accepted that the diagnosis and treatment of thrombocytopenia (TP) are within the professional competence of a hematologist. At the same time, a lot of data has now been accumulated indicating a decrease in the number of platelets in various pathological conditions. This explains the need for wider discussion of this issue among doctors of various clinical specialties.
General provisions
The term “thrombocytopenia” is usually used when platelet levels are below 100.0 × 109/L, although normal platelet levels are generally considered to be between 150.0 × 109/L and 450.0 × 109/L [1]. Therefore, a number of experts identify latent AFL at platelet levels from 100.0×109/L to 150.0×109/L [2]. The identification of latent TP, in our opinion, is justified from a practical point of view. On the one hand, such a clinical situation requires dynamic monitoring of platelet levels regardless of the cause, on the other hand, when the platelet count is 100.0 × 109/l or more, hemostasis is fully ensured, which, as indicated in most available guidelines, is safe in the context of the risk of developing bleeding [3] and which allows for various surgical interventions, incl. and delivery, at the specified platelet level.
Moreover, platelet concentrations from 100×109/L to 50×109/L, occurring without spontaneous hemorrhagic syndrome, can also be considered safe. In cases where signs of bleeding appear at the specified number of platelets, one should look for an additional factor provoking hemorrhagic syndrome, or take into account the presence of vascular pathology, for example, in elderly patients. Existing approaches indicate that correction of TP should be carried out when the platelet count is from 50×109/L to 30×109/L only in the presence of hemorrhagic manifestations. A platelet count below 10.0×109/L is critical for the development of life-threatening hemorrhagic manifestations. Patients with this level of TP require immediate treatment, regardless of the degree of clinical manifestations of hemorrhagic syndrome [3, 4].
Etiopathogenesis of TP
Speaking about TP, it is necessary to emphasize the diversity of pathogenetic mechanisms leading to it and the even greater number of pathological conditions in which these pathogenetic mechanisms are realized [5]. There are two main mechanisms of the pathogenesis of TP (Table 1): impaired platelet formation and increased platelet destruction.
Diagnostic algorithms for TP
When identifying TP in a patient, a detailed analysis of the disease history is very important, in particular, establishing the factors that preceded the development of TP: bacterial or viral infection, incl. and viral hepatitis; vaccination or use of medications; stay in countries with a risk of contracting infectious diseases (malaria, rickettsiosis, dengue fever, etc.); consumption of alcoholic and quinine-containing drinks; varicose veins, thrombosis, cardiovascular pathology and its therapy with anticoagulants and antiplatelet agents; the presence of concomitant diseases, especially autoimmune, infectious or tumor ones, occurring with TP, DIC syndrome; transfusion; history of organ transplantation; pregnancy; the presence and duration of bleeding after surgery.
In the family history, it is necessary to clarify the presence of diseases of the hematopoietic system in relatives.
When conducting an objective study, one should actively identify symptoms such as hypo- or hyperthermia, weight loss, symptoms of intoxication, hepato- and splenomegaly, lymphadenopathy, pathology of the mammary glands, heart, veins of the lower extremities, as well as congenital anomalies. All this data is not specific.
Laboratory and instrumental diagnostics includes several areas. In a clinical blood test, an optical count of the number of platelets and an assessment of the morphology of platelets (microforms and giant platelets) are required, but it should be remembered that in the presence of platelet aggregates, a repeat analysis is necessary to exclude “false” LT when using the preservative EDTA (ethylenediaminetetraacetate calcium-sodium). a test tube containing sodium citrate is used). All patients undergo an ultrasound or computed tomography (CT) scan of the abdominal cavity and retroperitoneal space, radiography or CT of the chest, as well as an examination to exclude oncological diseases. Taking into account that idiopathic thrombocytopenic purpura (ITP) is a diagnosis of exclusion, the range of laboratory tests used is quite wide (Table 2), according to their diagnostic significance they are divided into mandatory, potentially useful and tests with unproven informativeness.
Principles of ITP treatment
There are several lines of therapy in the treatment of ITP. At the first stage, hormones (prednisolone, dexamethasone) and specific immunoglobulin are used. Second-line therapy includes splenectomy and thrombopoiesis stimulators (thrombopoietin mimetics). Rituximab and other drugs with immunosuppressive effects (azathioprine, cyclophosphamide, cyclosporine A, vincristine, vinblastine) are considered as a reserve agent (third line of therapy) [4].
TP in gastroenterology
Taking into account the multiplicity of causes of TP, it is necessary to exclude diseases that may have a decrease in platelet levels in the clinical picture; in the practice of a gastroenterologist, these are primarily H. pylori-associated diseases and liver lesions of various origins.
In 1998, A. Gasbarrini et al. published in the Lancet journal the article “Regression of autoimmune thrombocytopenia after eradication of Helicobacter pylori”, which marked the beginning of a new direction in the study of helicobacter pylori, associated conditions, as well as closer interaction between doctors of two clinical specialties, namely gastroenterologists and hematologists [6] . It has previously been shown that autoimmune reactions through cross-mimicry between Lewis system antigens of gastric epithelial cells and H. pylori may play a role in Helicobacter-induced mucosal damage; monoclonal anti-H. pylori antibodies interact with tissues outside the gastrointestinal tract, namely with epithelial cells of the ducts of the salivary glands and renal tubules [7]; polyclonal anti-H. pylori antibodies interact with the capillaries of the renal glomeruli, which can lead to membranous nephropathy [8]. Based on data from previous studies, in particular on the results of observations [9] on the relief of manifestations of Henoch-Schönlein disease after successful eradication therapy, A. Gasbarrini et al. suggested a pathophysiological link between ITP and chronic H. pylori infection. They described an increase in platelet levels in all 8 ITP patients who received eradication therapy, while the platelet level in 3 people who did not receive such therapy remained unchanged.
To date, a lot of works, systematic reviews have been published that have studied the relationship between ITP and H. pylori, the mechanisms of development of this relationship, identifying predictors of a positive response to eradication therapy.
Several hypotheses have been proposed for the mechanisms by which H. pylori causes the development of ITP. It is believed that cross-reactive antibodies are produced that interact with both components of H. pylori and platelet surface antigens through molecular mimicry. Italian scientists led by R. Scandellari have shown that infection with H. pylori strains expressing CagA (cytotoxin-associated gene A) can cause chronic cases of ITP. According to their study, an increase in platelet count after eradication therapy was observed in 43% of patients after 6 months of follow-up. Patients were comparable for all major clinical features with one exception: serum anti-CagA antibodies were present in 83% of responders and only 12.5% of non-responders (p=0.026). The authors concluded that antibiotic therapy for H. pylori infection can lead to the disappearance of immune cross-reacting antibodies and, therefore, can be considered as a treatment option for patients with ITP, especially for those individuals who have antibodies to CagA [10]. Subsequently, based on data obtained by R. Scandellari et al., and also taking into account the fact that almost all CagA-positive strains of H. pylori also express a vacuolating toxin, a group of researchers led by N. Figura suggested the existence of molecular mimicry of some platelet peptides with vacuolating cytotoxin A of H. pylori. In particular, the platelet component binding domain of the 289 amino acid receptor for von Willebrand factor (GP1b-platelet) showed some structural similarity to H. pylori VacA-[11]. M. Michel et al. [12] also explored the molecular mimicry hypothesis and found that platelets from H. pylori-infected ITP patients, which have the ability to react with GPIIb/IIIa or GPIb, cannot recognize H. pylori antigens. On the other hand, T. Takahashi et al. [13] reported that platelets from patients with ITP infected with H. pylori “recognized” CagA in an immunoblotting reaction, but platelets from patients infected with H. pylori but without ITP did not. Y. Bai et al. studied the cross-reaction of a monoclonal antibody against Helicobacter urease B with the platelet surface glycoprotein GPIIb/IIIa and suggested that the immune response to UreB may be involved in the pathogenesis of ITP [14]. Taken together, these data suggest that cross-reacting antibodies against H. pylori may be present in patients with ITP, but their pathogenetic role is not completely clear.
Another mechanism considered is that chronic H. pylori infection may nonspecifically affect the host immune system, stimulating acquired immune responses through the production of T and B autoantibodies. Japanese researchers S. Yamanishi et al. [15] showed that H. pylori urease is capable of initiating autoimmune reactions by activating B1 cells, but this does not explain the development of a platelet glycoprotein-specific autoimmune response in ITP. Moreover, in the work of R. Pellicano et al. showed no differences in the production of nonspecific autoantibodies (antinuclear, antimicrosomal, antismooth muscle) in ITP in individuals with and without H. pylori [16].
M. Kuwana et al. [17] proposed a “pathogenic loop” model: the appearance of antiplatelet autoantibodies in patients with ITP. The point is that macrophages of the reticuloendothelial system “capture” platelets through Fcγ receptors and “transfer” platelet antigens (glycoproteins) to T cells (CD4+), which in turn, being activated, stimulate B cells to produce antiplatelet antibodies , resulting in binding to circulating platelets, thereby closing the “pathogenic loop”. After successful eradication of H. pylori, antiplatelet antibodies are removed [18], therefore, the “pathogenic loop” is stopped. M. Kuwana et al., having conducted a prospective study, showed increased phagocytic ability and low levels of expression of the inhibitory FcγRIIB in circulating monocytes in ITP patients infected with H. pylori; similar changes were not detected in H. pylori-negative patients. In the case of successful eradication, suppression of the activated monocyte phenotype was observed, followed by a decrease in the level of antiplatelet autoantibodies and an increase in the number of platelets. Thus, H. pylori may modulate the monocyte/macrophage Fcγ receptor balance in favor of Fcγ receptor activation [17, 19].
A number of studies have attempted to define the characteristics of H. pylori-associated ITP by comparing the clinical findings of adult patients with ITP with or without H. pylori infection. ITP patients infected with H. pylori were significantly older than those uninfected [20], but this may be because the prevalence of H. pylori infection increases with age in the general population. Many other studies found no significant differences in any other demographic or clinical characteristics, including gender, platelet count, or response to therapy. Several studies have found differences in the genetic factors of patients with ITP with or without H. pylori. Italian researchers D. Veneri et al. [21] studied the HLA-DRB1 and DQB1 alleles of patients with ITP and found that H. pylori-positive patients had lower frequencies of DRB1*03 and higher frequencies of DRB1*11, DRB1*14 and DQB1*03 compared with H pylori-negative patients. However, in Japanese patients with ITP, no association was found between H. pylori infection and the HLA-DRB1 or DQB1 alleles, but gene polymorphisms at loci for interleukin-1β (IL-1β) were found to be associated with H. pylori infection in patients with ITP in under 50 years of age [17, 22]. There were no differences in IL-2, -4, or -6 levels between ITP patients with and without H. pylori infection [23]. Serum levels of chemokines, typically regulated by T cells, were significantly higher in ITP patients with H. pylori infection than in patients without it, but similar increases also occurred in individuals who had H. pylori-associated gastrointestinal pathology. -intestinal tract, but there was no ITP [24]. Thus, to date, no demographic, clinical, genetic, or immunologic characteristics unique to H. pylori-infected ITP patients have been identified. This is likely due to the fact that there are at least two distinct subgroups of ITP patients infected with H. pylori: patients with secondary ITP caused by H. pylori, in which case these patients respond to eradication therapy, and those with primary ITP. ITP and “occasional” co-infection with H. pylori.
Factors predicting the positive effect of eradication therapy on the course of ITP, namely an increase in the number of platelets, have been widely studied. The most frequently identified favorable predictor is a shorter history of ITP [20, 25, 26], but other studies do not find this association [27–29]. Some investigators have reported a significant beneficial effect of H. pylori eradication in patients with mild AFL, but patients with severe AFL showed a poor response to eradication [30]. Clinical characteristics such as age less than 65 years at diagnosis of ITP [25], higher baseline platelet count [25], no prior corticosteroid therapy [27], no concomitant corticosteroid therapy [31, 32], and no prior therapy for ITP [25 ], are also considered as factors predicting a positive platelet “response” to treatment, but information about their reliability is even more controversial. Several studies have examined genetic predisposition to platelet response to H. pylori therapy; in particular, an association has been shown between HLA-DQB1*03 haplotypes and a higher likelihood of a positive platelet response [21]. Single nucleotide polymorphisms in the tumor necrosis factor β and Fcγ receptor IIB inhibitor (FcγRIIB) genes have been found to be useful for predicting the response of LT to eradication therapy [32, 33]. The presence of antiplatelet-specific anti-GPIb autoantibodies has been found to predict resistance to H. pylori eradication therapy [17]. There is conflicting evidence regarding the effect of anti-CagA antibodies on the prognosis of elevated platelet counts: a study in Italy found that patients with ITP and anti-CagA antibodies were more likely than patients without them to respond favorably to eradication therapy [10], but a study in Japan, this observation was not confirmed [26]. R. Sato et al. [34] assessed the potential relationship of platelet response to H. pylori eradication with fibroesophagogastroduodenoscopy data and the results of histological examination of gastric biopsies: severe inflammation and signs of atrophy in the body of the stomach were regarded as predictors of a favorable outcome. Thus, both genetic background and bacterial factors that regulate the level of inflammatory response to H. pylori infection can be used to predict the success of eradication therapy for the treatment of LT.
Despite encouraging research data, a number of scientists doubt the existence of a causal relationship between ITP and H. pylori infection, and, accordingly, the effect of eradication therapy on platelet counts. Thus, the results of work carried out by AD Samson et al. [35] report no significant differences between H. pylori-positive and H. pylori-negative patients in terms of platelet counts. Researchers from Malaysia [36] reported a low prevalence of H. pylori infection in patients with ITP and no significant effect of H. pylori eradication on platelet counts.
LT is a common hematological disorder in patients with chronic liver disease [2, 37]. The prevalence of LT varies depending on a number of factors, such as the patient population and the severity of the underlying liver disease, and the degree of LT serves as an early prognostic marker (APRI - Aspartate-aminotransferase-to-Platelet Ratio Index), allowing a preliminary assessment of the presence of significant liver disease. liver fibrosis without resorting to biopsy [38]. The incidence of AFL among patients with liver cirrhosis reaches 80% [39].
The genesis of TP in liver diseases is multifactorial. The pathophysiology of TP in chronic liver disease has long [40] been associated with the hypothesis of hypersplenism, when portal hypertension causes the pooling and sequestration of all corpuscular elements of the blood, mainly platelets, in an enlarged and congested spleen. Liver transplantation normalizes liver failure and reduces hypersplenism [41].
Impaired platelet formation in liver diseases is also associated with a decrease in the activity and level of thrombopoietin, the main cytokine produced by the liver and affecting all stages of megakaryocyte differentiation and platelet synthesis.
In addition to the effect on hematopoietic cells, there is an assumption that thrombopoietin binds directly to platelets circulating in the vascular bed, which leads to an increase in their functional activity [42]. A decrease in thrombopoietin synthetic function of the liver leads to a decrease in thrombopoiesis in the bone marrow and, consequently, to TP in the peripheral blood. Restoration of adequate thrombopoietic production after liver transplantation leads to a rapid restoration of platelet production [43].
Suppression of platelet formation in the bone marrow can be caused by alcohol, one of the common etiological factors of liver disease. Alcohol-induced AFL is due to the direct toxic effect of alcohol on megakaryocytes, resulting in decreased platelet production, survival time, and function [44, 45]. A number of drugs used in the treatment of liver diseases (azathioprine, β-lactam antibiotics and fluoroquinolones, interferon) can potentially cause drug-induced AFL, having both a direct myelosuppressive effect and immune-mediated platelet destruction. Until recently, treatment regimens for patients with HCV (Hepatitis C Virus) included interferon, a common side effect of which is dose-dependent LT, interferon-induced myelotoxicity and cytopenia became a common reason for discontinuation of therapy [2, 46].
Another proven pathogenetic mechanism for the development of TP is autoimmune disorders. Among patients with chronic liver diseases of various etiologies, up to 64% have antiplatelet antibodies, which are mainly directed against the glycoprotein IIb-IX complex [47]. Most often, immune-mediated LT occurs with HCV, bacterial and drug-induced liver damage. Autoimmune liver diseases (autoimmune hepatitis and primary biliary cholangitis - PBC) are often associated with other autoimmune conditions. About 50% of patients with PBC have at least one additional autoimmune disease, which may include ITP [48].
Some etiological factors of liver damage have their own mechanisms that affect platelet levels. Thus, it has been shown that HCV infection can lead to the appearance of TP in a patient before the stage of cirrhosis and hypersplenism appears. More than 20 years ago, studies appeared indicating the association of HCV and TP [49–51]. Up to 30% of patients with ITP without evidence of progressive liver disease are HCV seropositive [52]. Chronic HCV infection can lead to LT through various mechanisms [53], one of which is direct suppression of bone marrow hematopoiesis [54]. Patients with HCV demonstrate platelet depression even in the absence of splenomegaly [55] and normalization of platelet levels after successful treatment of infection [56]. Chronic HCV infection is known to be associated with a variety of autoimmune disorders, with approximately 40% of patients with HCV infection having at least one immune-mediated extrahepatic manifestation during the course of their disease [57, 58]. A decrease in platelet levels in HCV correlates with the severity of the disease and is accompanied by an increase in antiplatelet Ig titers [49, 55]. In addition, HCV can directly interact with platelets to bind platelet membranes through multiple cell surface receptors, ultimately leading to phagocytosis of platelets with antibody and accelerated platelet destruction by the reticuloendothelial system [59].
Binding of HCV to platelets can also induce the formation of antigens on the platelet surface or alter the properties of the platelet glycoprodeid membrane, which contributes to the formation of autoantibodies, such as GPIIb/IIIa, and the subsequent development of LT [60]. Finally, HCV is closely associated with cryoglobulinemia, and cryoglobulins may play a role in the formation of immune complexes and the development of TP [61].
Conclusion
TP is a complex and multifactorial phenomenon, often encountered in the practice of a gastroenterologist. A thorough understanding of the pathophysiology of TP in relation to its cause is critical when choosing treatment strategies. Awareness of specialists about the mechanisms of development of TP in diseases of the digestive system will help to increase the success of therapy.
Thrombocytopenia redistribution
If we explain this mechanism very simply, it looks like this: due to some reasons, the patient’s spleen enlarges. And if under normal conditions it stores up to 30% of platelets, then in an enlarged state it retains up to 90% of these cells. At the same time, the system does not see that there are not enough platelets and does not trigger a compensatory mechanism.
The mechanism is also based on various causes: cirrhosis of the liver, some infections such as tuberculosis, autoimmune diseases (systemic lupus erythematosus), tumors of the circulatory system, alcoholism.
Causes of thrombocytopenia
Among the various reasons causing this serious disease, the main ones are:
Thrombocytopenia dilution
This condition is usually observed in people who receive a large number of transfusions of various liquids: for example, plasma, plasma substitutes, etc. As a result, the level of platelets decreases due to the banal dilution of the blood.
Considering the huge number of reasons that can cause immune thrombocytopenia (and we have not named all the options), a patient with its symptoms should immediately consult a doctor who will find the essence of the problem and prescribe effective treatment.
Diagnostics
Since there are so many reasons, it is not possible to name diagnostic measures in detail - everything will depend on the specific situation. But we can highlight the main components of diagnosis:
- General blood analysis.
- Checking bleeding time (Duke test).
- Determining the time it takes for blood to clot.
- Red bone marrow puncture. The method allows you to identify quantitative and qualitative changes in cells.
- Determination of antibodies in blood.
- Research for genetic diseases.
- Ultrasound of internal organs. Most often, the liver and spleen are studied immediately, but this list can be very large.
- MRI. Used to study internal organs and blood vessels.
Diagnosis of the disease begins with a visit to a general practitioner, who, based on a survey, initial examinations and tests, prescribes visits to other specialists.
When should you take the Platelet Aggregation with Adrenaline test?
- Before prescribing drugs that affect the coagulation system.
- Differential diagnosis of diseases accompanied by pathological bleeding.
- As part of a comprehensive assessment of the platelet component of hemostasis in patients before (major) surgery, as well as in pregnant women at high risk of developing obstetric complications.
- Determination of resistance to drugs from the group of antiplatelet agents.
- Identification of hereditary and acquired thrombocytopathies.
Treatment and severity
Treatment of thrombocytopenia most often comes down to identifying the primary disease and its treatment, as well as eliminating various unpleasant symptoms. In the process, it is also important to take into account that the severity of thrombocytopenia varies:
Mild degree. It assumes that the platelet concentration is from 50 to 150 thousand units per microliter. The condition of the capillaries is usually normal, bleeding does not develop. Usually, treatment is not necessary at this stage - doctors recommend waiting and monitoring the development of the patient’s condition.
Average degree. In this case, the concentration is 20-50 thousand platelet units per microliter. Under this condition, bleeding gums and nosebleeds are observed. If injuries and bruises occur, serious hemorrhages form in the skin. At this stage, drug therapy may be prescribed.
Severe degree. The platelet concentration is below 20 thousand, hemorrhages are spontaneous and severe. At the same time, the patient himself may feel quite comfortable, does not complain of feeling unwell, but tests show that he needs help.
Since the treatment of thrombocytopenia requires the most thorough and detailed diagnosis, it is important to choose a modern clinic that will help you. JSC "Medicine" in Moscow is just the place where you can get qualified help from the best specialists. The clinic has everything necessary for both examination and treatment of each patient.
Treatment of thrombocytopenia
Thrombocytopenia is treated by a hematologist. First, the patient’s condition is assessed and the severity of the hemorrhagic syndrome is studied.
- With mild severity (50,000-150,000 platelets per μl of blood), the capillary walls are in normal condition, so blood does not leave the vascular bed. Severe bleeding does not develop. Therefore, the problem can be solved without medications. The cause of the disease is being determined. The doctor adheres to a wait-and-see approach. The patient is not hospitalized.
- With moderate severity (25,000-50,000 platelets per μl of blood), hemorrhages in the oral mucosa and nosebleeds are observed. With minor bruises, large bruises form. If there is a risk of bleeding (presence of a stomach ulcer, playing professional sports, etc.), drug therapy is carried out. The patient can undergo treatment at home.
- With severe thrombocypenia (less than 20,000 platelets per μl of blood), spontaneous bleeding occurs in the mucous membranes of the mouth and skin. Hemorrhagic syndrome appears. Prescription of complex drug therapy is mandatory. The patient is hospitalized.
Treatment of thrombocytopenia with drugs
Drug treatment for any form of thrombocytopenia is aimed at:
- stopping bleeding;
- eliminating the cause;
- treatment of the disease that caused the problem.
Patients are usually prescribed medications:
- "Prednisolone";
- "Intraglobulin", "Imbiogam";
- "Revolade";
- "Vincristine";
- "Etamzilat";
- "Depo-Provera";
- vitamin B12.
Non-drug treatments for thrombocytopenia
Treatment of thrombocypenia can be carried out using therapeutic and surgical measures. Most often, hematologists resort to:
- Transfusion therapy. The patient is transfused with donor blood (plasma or platelets).
- Removal of the spleen. The spleen is the main source of antibodies in immune thrombocytopenia and the main site of platelet destruction, so sometimes it is completely or partially removed. In most patients, after removal of the spleen for thrombocytopenia, the condition returns to normal and the clinical symptoms of the disease disappear.
- Bone marrow transplant. First, the patient is prescribed large doses of anticancer drugs that suppress the immune system. This is done in order to prevent the immune system from reacting to the introduction of donor bone marrow, as well as to destroy tumor cells if we are talking about a tumor of the hematopoietic system.
Treatment of thrombocytopenia during pregnancy
Thrombocytopenia in pregnant women requires proper treatment. Typically, expectant mothers are prescribed short courses of glucocorticosteroids (Dexamethasone, Prednisolone). In the third trimester, they accelerate the maturation of the fetal lungs, which makes early delivery possible.
If glucocorticosteroids are ineffective, immunoglobulin is administered intravenously. During the entire pregnancy it is used three to four times, and then again immediately after childbirth. In emergency situations, platelet transfusions are used.
If all the measures taken do not eliminate the symptoms of the disease, the spleen is removed in the second trimester (surgery is especially often resorted to if severe gestational thrombocytopenia is diagnosed in the first trimester). Ideally, surgery should be performed laparoscopically.
The issue of delivery is always decided on an individual basis. Thrombocytopenia during childbirth can lead to severe bleeding, so doctors carefully weigh the pros and cons. A cesarean section is considered less traumatic for the female body.
Treatment of thrombocytopenia with folk remedies
Thrombocytopenia is treated with the leaves of nettle, yarrow, and strawberry. Herbs are brewed with boiling water and drunk chilled, 1/4 cup 3-4 times a day.
Sesame oil has proven itself well for thrombocytopenia. It should be taken one tablespoon 3 times a day.