Classification of vasculitis
Large arteries
Giant cell arteritis (old Horton's disease)
Horton's disease is characterized by damage to the temporal artery and extracranial branches of the carotid artery. Develops in people after 50 years of age in combination with polymyalgia rheumatica or separately.
Takayasu's disease (nonspecific aortoarteritis)
Chronic inflammation of the aorta and its branches, which leads to thickening of the wall, which causes a narrowing of the lumen of the vessel up to its occlusion. Causes blockage (occlusion) of blood vessels. Accompanied by the absence of a pulse in one or both arms. Often complicated by the development of aneurysm and aortic stenosis. It affects mainly young people; according to statistics, women predominate.
Medium caliber arteries
Polyarteritis nodosa
It is not primary in 20% of cases. Accompanied by necrosis of small and medium-sized arteries with severe damage to any organ. It is segmental and has a tendency to zones of vascular bifurcation. Mostly occurs in middle-aged men. Most often associated with hepatitis B or C. Less common due to vaccination against hepatitis B.
Small and medium arteries
ANCA-associated vasculitis
ANCA-associated vasculitis includes granulomatosis with polyangiitis (Wegener's granulomatosis), eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome), microscopic polyangiitis, and damage to small vessels.
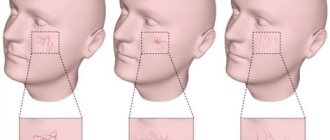
It is characterized by a clinical triad of granulomatous vasculitis, glomerulonephritis and varying degrees of small vessel vasculitis. Upper respiratory tract symptoms are usually present, including sinusitis, nasal obstruction and perforation, which can lead to deformity. Other common symptoms include otitis media, ear pain and hearing loss.
Hemorrhagic vasculitis
Affects arterioles, venules and capillaries. Characterized by immune deposits of IgA. Accompanied by disorders of small vessels in the intestines, skin and kidneys. Combined with arthritis and arthralgia.
About 5% of patients with cutaneous vasculitis have a systemic form of the disease.
It is characterized by damage to small and medium-sized vessels, including granulomatosis and microscopic polyangiitis. It is characterized by inflammation and granuloma formation affecting small arteries, arterioles, venules and capillaries. The most common symptoms are sinus pain, rhinorrhea or nasal ulcers, otalgia or deafness, cough, shortness of breath, and hemoptysis.
Churg-Strauss syndrome
Allergic inflammatory lesion of medium and small vessels. Occurs with the appearance of eosinophilic necrotizing granulomas. It is characterized by involvement of the joints, nervous system (peripheral and central), gastrointestinal tract, heart, bronchi and lungs.
Microscopic vessels
Microscopic vasculitis (microscopic polyangiitis)
The form of the disease is associated with rapidly progressing kidney disease (focal segmental necrotizing glomerulonephritis), skin lesions (>75% purpura), damage to the lungs, peripheral nervous system, and the presence of antibodies to p-ANCA. Microscopic vasculitis has the worst
prognosis than other forms of the disease.
Cryoglobulinemic vasculitis
Organ damage is caused by vascular occlusion. This condition develops against the background of various pathologies, including infections, autoimmune diseases and neoplasms. Characteristic clinical findings: purpura, arthralgia and weakness. Ulcers and ischemic lesions also occur.
Combined form of the disease
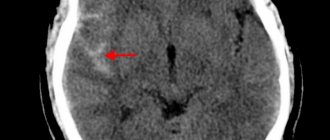
Cerebral vasculitis (vasculitis affecting the central nervous system)
The disease is caused by inflammation of the walls of cerebral vessels of various sizes. It is characterized predominantly by a secondary form of development. Signs are variable - paresis, encephalopathy, epileptic seizures, mental disorders and fainting.
Diagnosis of vasculitis
Which doctor should I contact to diagnose vasculitis? First of all, you need to make an appointment with a rheumatologist. To clarify the diagnosis, a rheumatologist may involve other specialists, in particular dermatologists and immunologists.
A doctor cannot diagnose vasculitis based only on the skin manifestations of the disease. The fact is that the pathology can “masquerade” as others, so the patient needs to perform a number of tests:
- general blood analysis;
- general urine analysis;
- coagulogram;
- determination of the level of antistreptolysin-O, IGA in peripheral blood;
- determination of antibodies to hepatitis B and C (with vasculitis they are often found in the blood);
- tissue biopsy of the affected organ or body part followed by histological examination of the biopsy;
- PCR test;
- determination of antibodies to hepatitis B and C (with vasculitis they are often found in the blood);
- X-ray, ultrasound, CT or MRI (as indicated).
To make a diagnosis of hemorrhagic vasculitis, the patient must have two or more diagnostic criteria:
- specific rashes not associated with low platelet levels;
- manifestation of the disease before the age of 20 years;
- widespread abdominal pain that worsens after eating, intestinal bleeding;
- granulocytic infiltration of the walls of microvasculature vessels, which is confirmed histologically.
Symptoms of vasculitis in a child
There are dozens of vasculitis - each of them affects one or another type of vessel and is accompanied by specific symptoms. They appear when damaged:
- skin - spotty hemorrhages;
- nerves - partial or complete loss of sensitivity;
- joints - joint pain;
- visceral vessels – abdominal pain;
- kidney – glomerulonephritis;
- brain - strokes.
General symptoms:
- weakness and increased fatigue,
- temperature increase,
- loss of appetite,
- pallor.
The most common vasculitis:
- hemorrhagic,
- allergic,
- urticarial,
- Wegener's granulomatosis,
- Kawasaki disease.
Hemorrhagic vasculitis is manifested by a palpable hemorrhagic skin rash, pain in the ankle and knee joints, sometimes in smaller ones. Cramping abdominal pain lasting from 3 to 10 days is not uncommon, and its clinical manifestations are similar to appendicitis, ulcer perforation and intestinal obstruction. Sometimes they are accompanied by nausea and vomiting, blood in the vomit and stool, and kidney damage - homerulonephritis. The diameter of the rash is 1-3 mm. The rash is symmetrical and initially appears on the legs and feet. Erythema and areas of necrosis are possible. Source: E.V. Borisova Hemorrhagic vasculitis in children // Pediatrics, No. 6, 2004, pp. 51-56
Symptoms of allergic vasculitis:
- erythematous and hemorrhagic spots and nodules;
- hemorrhages under the toenails;
- itching and pain in the rash area;
- necrosis – necrosis and blackening of the skin in the area of the rash;
- pain in muscles and joints.
The disease affects the lower extremities, and in generalized forms it also affects the trunk and forearms. In Behcet's disease, the mucous membranes of the mouth and eyes are affected, ulcers and erosions form.
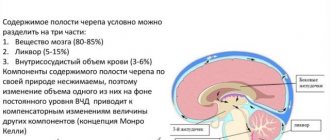
With urticarial vasuclititis, dense blisters appear. Fever and muscle weakness, joint pain and kidney failure may occur. Diarrhea, conjunctivitis, laryngeal edema, increased intracranial pressure and cardiac arrhythmias are common.
Wegener's granulomatosis is manifested by damage to the kidneys and lungs, laryngeal stenosis, and nodular rashes on the skin.
Kawasaki syndrome - damage to the blood vessels of the heart, respiratory tract and lymph nodes. It begins rapidly with an increase in temperature to 38-41 oC. Other symptoms:
- debilitating fever;
- a rash with plaques that resembles scarlet fever;
- damage to the eyes and respiratory system;
- thickening and redness of the skin on the palms and soles;
- enlarged cervical lymph nodes;
- redness of the tongue;
- peeling of the skin of the fingers;
- aneurysm and heart pain. Source: I.Ya. Lutfullin Kawasaki syndrome: clinical algorithms and the problem of underdiagnosis of the disease // Bulletin of modern clinical medicine, 2021, vol. 9, issue 2, 52-60
Treatment of vasculitis
Treatment of vasculitis in adults and children depends entirely on the form of the disease and the causes that caused it. A number of patients at the Yauza Clinical Hospital undergo extracorporeal hemocorrection, which not only improves the patient’s condition, but also corrects the functioning of the immune system.
Therapeutic measures
Treatment of vasculitis in our clinic, including hemorrhagic, is aimed at achieving the following goals:
- elimination of clinical signs of pathology;
- reducing the risk of complications;
- preventing damage to vital organs;
- complete recovery of the patient or achievement of stable long-term remission.
To do this, our specialists - rheumatologist, dermatologist, allergist - develop an individual treatment regimen for each patient, which includes:
- bed rest for at least 3 weeks;
- avoiding contact with allergens;
- diet therapy;
- prescribing enterosorbents, antihistamines, antispasmodics, hemostatic agents and antiplatelet agents;
- in some cases, the use of hormones and cytostatics is justified.
To reduce the destructive influence of circulating immune complexes and enhance the effectiveness of drug therapy, patients with severe forms of vasculitis are treated with extracorporeal hemocorrection methods.
Physiotherapeutic methods for treating vasculitis
Plasmapheresis has proven its effectiveness. The physiotherapeutic procedure is aimed at improving kidney function and preventing the development of renal failure. Extracorporeal methods of blood purification are effective in combination with intravenous administration of immunoglobulins.
The most significant therapeutic effect can be achieved if harmful substances are concentrated in the liquid component of the bloodstream. Before the procedure, precise dosing of the amount of VCP (volume of circulating plasma) is necessary.
Drug treatment
Medicines are prescribed individually, depending on the characteristics of the patient’s body and the form of the disease:
- giant cell arteritis - GC (glucocorticosteroids) and pulse therapy with methylprednisolone, as well as leflunomide, methotrexate, genetic engineering therapy with drugs such as tocilizumab;
- Takayasu arteritis – glucocorticosteroids, basic anti-inflammatory drugs (methotrexate, etc.), genetic engineering therapy (tocilizumab);
- polyarteritis nodosa - GK until a clinical effect is achieved, then in a maintenance dose in combination with azathioprine or cyclophosphamide;
- Wegener's granulomatosis - for dysfunction of the upper respiratory tract, biseptol is prescribed (helps cope with the infection). Treatment can be carried out with GC, azathioprine, cyclophosphamide (it always pulses first); rapid progression requires pulse therapy, also rituximab;
- Churg-Strauss syndrome – GC with dose reduction and cytostatics, genetic engineering therapy.
In any case, it is necessary to prescribe drugs that improve blood flow, suppress the immune system and relieve inflammation. If necessary, the patient is referred to other specialists.
Hemorrhagic vasculitis - treatment with hemocorrection methods
EG is indicated at the very beginning of clinical manifestations. Early treatment with hemocorrection methods effectively prevents the development of serious complications and allows for rapid and long-term remission of the disease, which has a beneficial effect on the patient’s ability to work and his quality of life.
Advantages of EG methods
This treatment method allows:
- reduce activity or quickly stop the pathological process and, thereby, reduce the risk of complications in hemorrhagic vasculitis from the kidneys, joints,
- accelerate the disappearance of clinical manifestations of the skin, kidneys, gastrointestinal tract, joints, etc., including in the treatment of vasculitis on the legs,
- improve blood supply to affected organs,
- increase the body's sensitivity to medications, including hormonal drugs, allowing their dosage to be reduced (even to the point of discontinuation).
The following methods of extracorporeal hemocorrection are indicated for the treatment of vasculitis:
- cryoapheresis;
- cascade plasma filtration;
- immunosorption;
- high-volume plasma exchange;
- extracorporeal pharmacotherapy;
- photopheresis
Indications for EG are: the presence of vascular lesions confirmed by biopsy, abdominal syndrome, ineffectiveness of drug therapy, side effects or complications when using drugs.
Prevention
Unfortunately, it is impossible to protect yourself one hundred percent from the appearance of vasculitis. Preventive measures include maintaining immunity, a healthy lifestyle, and paying attention to health.
If a person has already been diagnosed with vasculitis, we must not forget that the disease can return, so you need to carefully monitor your well-being.
Medical specialists in St. Petersburg remind: the sooner treatment is started, the less negative impact the disease will have on the body. If symptoms appear, consult a doctor immediately. Registration by phone is carried out around the clock.
Consequences and complications
Acute complications that lead to death from systemic vasculitis occur due to vascular occlusion or rupture, resulting in lack of blood supply or bleeding, respectively.
Vasculitis of large vessels can cause complications from:
- arteries - aneurysm (protrusion of the wall) and its rupture;
- brain (infarction or hemorrhage) is a rare phenomenon, mainly large vessels are affected, and cranial ones cause loss of vision, which is described below;
- eye (vision loss or double vision);
- limbs (lack of strength);
- heart disease (angina or heart attack) is a rare occurrence;
- kidneys and intestines (bleeding) is a rare occurrence with vasculitis of large vessels.
In small vessel vasculitis, the lungs and kidneys can be diffusely affected and cause acute failure. Characteristic damage to peripheral nerves due to lack of blood supply, which leads to impaired sensitivity and/or lack of strength in the limbs, the development of paresis. The skin may also be affected (purpura, nodules, or ulcers), depending on the type of vasculitis.
Chronic complications arise from the irreversible damage that vasculitis causes in organs or tissues initially or during various periods of progression. This is why it is important to establish a diagnosis and begin treatment as early as possible. These complications worsen the prognosis of the disease and, above all, the quality of life of patients. To the acute and chronic complications caused by this disease, one should also add the side effects of treatment with glucocorticoids and immunosuppressants used for vasculitis.
Which doctor treats, how is the disease diagnosed?
Having discovered the first symptoms indicating this disease, a person is interested in what the doctor is treating for it.
If you have a rash on the skin of your legs and other symptoms of vasculitis, consult your doctor. To make the correct diagnosis, he will refer specialists for consultations - a dermatologist, rheumatologist, neurologist, allergist, hematologist and others.
The attending physician prescribes additional tests:
- Clinical and biochemical analysis of blood, urine;
- ECG, X-ray, ultrasound;
- biopsy;
- immunological analysis.
Most often, when the disease is first detected, the final diagnosis is made by a rheumatologist, who, if necessary, refers the patient to a specialist. Based on the results of the study, the specialist prescribes treatment aimed at eliminating the causes of vasculitis.
After completion of treatment, the patient must be under medical supervision for two years to avoid relapse.