Subarachnoid hemorrhage is a condition caused by cerebral bleeding, in which blood accumulates in the subarachnoid space of the cerebral membranes. It is characterized by intense and sharp headache, short-term loss of consciousness and confusion in combination with hyperthermia and meningeal symptom complex. Diagnosed by CT and cerebral angiography; if they are unavailable, by the presence of blood in the cerebrospinal fluid. The basis of treatment is basic therapy, relief of vasospasm and surgical exclusion of the cerebral aneurysm from the bloodstream.
ICD-10
I60 Subarachnoid hemorrhage
- Causes Risk factors
- Pre-hemorrhagic period
- Basic and specific therapy
Diagnosis and treatment of subarachnoid cerebral hemorrhage
The doctor clarifies the victim’s medical history and conducts an external examination. The diagnosis is established on the basis of CT data, which makes it possible to determine the extent of the process, the presence of edema, and assess the condition of the cerebrospinal fluid system. If the results are negative, a lumbar puncture is performed.
MRI is a sensitive tool for diagnosing pathology after a few days. Vascular angiography is used to determine the source of bleeding in the brain.
Therapy for subarachnoid hemorrhage takes place in a neurological hospital and depends on the severity of the patient’s condition. It is aimed at solving the following problems:
- stabilization of the patient's condition;
- prevention of recurrent episode;
- normalization of homeostasis;
- treatment and prevention of ischemia, vascular spasm;
- therapy for the disease that caused the hemorrhage.
The aneurysm is clipped or endovascular occlusion is performed. Vasospasm and ischemia are treated with medication. In case of local spasm of a vessel, a vasodilator drug is injected directly into it or balloon angioplasty is performed.
In 50% of cases, subarachnoid hemorrhage leads to death. The majority develop significant impairments in the functional activity of the brain.
You can get help with this pathology at the Department of Neurosurgery of the City Clinical Hospital named after. A.K. Eramishantseva. The clinic has modern diagnostic equipment and advanced equipment for performing complex operations.
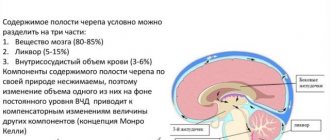
General information
Subarachnoid hemorrhage (SAH) is a separate type of hemorrhagic stroke in which blood leaks into the subarachnoid (subarachnoid) space. The latter is located between the arachnoid (arachnoid) and soft cerebral membranes and contains cerebrospinal fluid. Blood poured into the subarachnoid space increases the volume of fluid contained in it, which leads to an increase in intracranial pressure. Irritation of the soft cerebral membrane occurs with the development of aseptic meningitis.
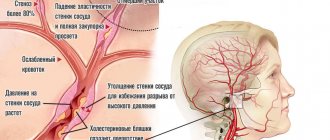
Vasospasm that occurs in response to bleeding can cause ischemia of certain areas of the brain with the occurrence of ischemic stroke or TIA. Subarachnoid hemorrhage accounts for about 10% of all strokes. Its frequency of occurrence per year varies from 6 to 20 cases per 100 thousand population. As a rule, SAH is diagnosed in people over 20 years of age, most often (up to 80% of cases) in the age range from 40 to 65 years.
Subarachnoid hemorrhage
Causes of hemorrhages in the ventricles of the brain
The reasons for the formation of hemorrhage in the ventricles of the brain are not fully understood and there are no specific clear reasons for this pathology.
Risk factors include the following:
- Arterial hypertension (in primary hemorrhages) is a chronic increase in blood pressure, especially dangerous in the absence of at least basic treatment.
- Uncontrolled use of antiplatelet agents, fibrinolytics.
- Vascular aneurysms are enlargements of an artery and can be congenital or acquired.
- Diabetes mellitus (with this disease the level of glucose in the blood constantly increases, which causes all kinds of complications).
- Mechanical damage to cerebral vessels (trauma).
- Hemorrhagic diathesis is increased fragility of the walls of blood vessels.
- Oncological diseases - benign and malignant tumors.
- Infectious and inflammatory processes in brain tissue (encephalitis).
There are many reasons that contribute to hemorrhage in the ventricles of the brain. They primarily affect nervous tissue. Primary factors provoke multiple complications, which leads to hemorrhages of this kind. One of the first such complications is an increase in the permeability of the walls of the vessels of the ventricular system.
Causes
Most often, subarachnoid bleeding is a complication of cerebrovascular diseases and head injuries.
- Rupture of a vascular aneurysm. It causes subarachnoid hemorrhage in 70-85% of cases. If you have a cerebral aneurysm, the chance of it rupturing ranges from 1% to 5% per year and from 10% to 30% throughout your life. Diseases often accompanied by the presence of a cerebral aneurysm include: Ehlers-Danlos syndrome, phakomatoses, Marfan syndrome, anomalies of the circle of Willis, coarctation of the aorta, congenital hemorrhagic telangiectasia, polycystic kidney disease and other congenital diseases. Cerebral AVMs usually lead to hemorrhage into the cerebral ventricles or parenchymal-subarachnoid hemorrhage and are rarely the etiological factor of isolated SAH.
- Head injuries. Subarachnoid hemorrhage of traumatic origin occurs during TBI and is caused by injury to blood vessels due to a skull fracture, brain contusion or compression. An example of such SAH is subarachnoid hemorrhage caused by birth trauma of the newborn. Risk factors for SAH in a newborn are a narrow pelvis in a woman in labor, rapid labor, post-term pregnancy, intrauterine infections, a large fetus, fetal developmental abnormalities, and prematurity.
- Pathology of ectracranial arteries. Subarachnoid hemorrhage can occur due to dissection of the vertebral or carotid artery. In the vast majority of cases, we are talking about dissection of the extracranial sections of the vertebral artery, spreading into its intradural section.
- Rare factors. In some cases, the cause of SAH is cardiac myxoma, cerebral tumor, vasculitis, angiopathy due to amyloidosis, sickle cell anemia, various coagulopathies, and anticoagulant treatment.
Risk factors
Along with the direct causes of SAH, contributing factors are identified: arterial hypertension, alcoholism, atherosclerosis and hypercholesterolemia, smoking. In 15-20% of SAH, the cause of hemorrhage cannot be determined. In such cases, they talk about the cryptogenic nature of SAH. Such variants include nonaneurysmal perimesencephalic benign subarachnoid hemorrhage, in which bleeding occurs in the cisterns surrounding the midbrain.
Causes of subarachnoid hemorrhage
In most cases, this condition is caused by non-traumatic factors:
- aneurysm rupture;
- rupture of a vessel in the brain against the background of arterial hypertension, atherosclerosis and other vascular diseases.
Subarachnoid hemorrhage in the brain can also be caused by traumatic factors:
- traumatic brain injury;
- brain contusion;
- fracture of the skull bones.
Main services of Dr. Zavalishin’s clinic:
- consultation with a neurosurgeon
- treatment of spinal hernia
- brain surgery
- spine surgery
Classification
In accordance with the etiofactor, subarachnoid hemorrhage is classified into post-traumatic and spontaneous. Traumatologists are often faced with the first option, and specialists in the field of neurology with the second. Depending on the area of hemorrhage, isolated and combined SAH are distinguished. The latter, in turn, is divided into subarachnoid-ventricular, subarachnoid-parenchymatous and subarachnoid-parenchymatous-ventricular.
In world medicine, the Fisher classification is widely used, based on the prevalence of SAH according to the results of CT scans of the brain. In accordance with it, they distinguish:
- class 1 - no blood
- class 2 - SAC less than 1 mm thick without clots
- class 3 - SAC more than 1 mm thick or with clots
- class 4 - predominantly parenchymal or ventricular hemorrhage.
CT scan of the brain. Blood in the subarachnoid cerebrospinal fluid spaces on the right. (photo by V.N. Vishnyakov)
Symptoms of subarachnoid hemorrhage
Pre-hemorrhagic period
Precursors of SAH are observed in 10-15% of patients. They are caused by the presence of an aneurysm with thinned walls through which the liquid part of the blood leaks. The time of occurrence of precursors varies from a day to 2 weeks before SAH. Some authors distinguish it as the pre-hemorrhagic period. At this time, patients note transient cephalgia, dizziness, nausea, transient focal symptoms (damage to the trigeminal nerve, oculomotor disorders, paresis, visual impairment, aphasia, etc.). In the presence of a giant aneurysm, the clinic of the pre-hemorrhagic period has a tumor-like character in the form of progressive cerebral and focal symptoms.
Acute period
Subarachnoid hemorrhage manifests itself with acute, intense headache and disturbances of consciousness. With aneurysmal SAH, unusually strong, rapidly growing cephalalgia is observed. With arterial dissection, the headache is biphasic. Short-term loss of consciousness and confusion lasting up to 5-10 days are typical. Possible psychomotor agitation. Prolonged loss of consciousness and the development of severe disturbances (coma) indicate severe bleeding with bleeding into the cerebral ventricles.
The pathognomonic sign of SAH is the meningeal symptom complex: vomiting, neck stiffness, hyperesthesia, photophobia, meningeal symptoms of Kernig and Brudzinski. It appears and progresses on the first day of hemorrhage, can have varying severity and persist from several days to a month. The addition of focal neurological symptoms on the first day speaks in favor of combined parenchymal-subarachnoid hemorrhage. The later appearance of focal symptoms may be a consequence of secondary ischemic damage to brain tissue, which is observed in 25% of SAH.
Typically, subarachnoid hemorrhage occurs with a rise in temperature to febrility and viscero-vegetative disorders: bradycardia, arterial hypertension, and in severe cases, respiratory and cardiac dysfunction. Hyperthermia can be delayed and occurs as a consequence of the chemical action of blood breakdown products on the cerebral membranes and the thermoregulatory center. In 10% of cases epileptic seizures occur.
Atypical forms of SAH
In a third of patients, subarachnoid hemorrhage has an atypical course, masquerading as a paroxysm of migraine, acute psychosis, meningitis, hypertensive crisis, and cervical radiculitis.
- Migraine form. Occurs with the sudden onset of cephalgia without loss of consciousness. The meningeal symptom complex appears 3-7 days later as the patient’s condition worsens.
- False hypertensive form. Often regarded as a hypertensive crisis. Because cephalalgia manifests itself against the background of high blood pressure numbers. Subarachnoid hemorrhage is diagnosed during further examination of the patient if the condition worsens or rebleeds.
- The false inflammatory form imitates meningitis. Cephalgia, febrility, and severe meningeal symptoms are noted.
- The false psychotic form is characterized by a predominance of psychosymptomatics: disorientation, delirium, severe psychomotor agitation. It is observed when an aneurysm of the anterior cerebral artery, which supplies blood to the frontal lobes, ruptures.
Subarachnoid hemorrhage
The patient is prescribed strict bed rest with the exception of any physical and emotional stress. It is necessary to ensure a sufficient supply of fluids and nutrients. For agitation, diazepam is prescribed; to reduce headaches, non-narcotic analgesics and codeine are prescribed. Repeated lumbar punctures to reduce intracranial pressure are performed in those patients for whom the first diagnostic lumbar puncture brought relief from headaches. With the development of acute hydrocephalus, dehydrating drugs are administered, sometimes the ventricles are drained, up to the application of a ventriculoperitoneal shunt.
Coagulants are administered only in the first 2 days. Then their administration is impractical due to the development of microcirculation disorders in the brain due to prolonged spasm of the large arteries of the base of the brain. In cases of deterioration - an increase in cerebral and focal symptoms on the 3-5th day from the moment of subarachnoid hemorrhage and the absence of signs of repeated subarachnoid hemorrhage in the cerebrospinal fluid - small doses of heparin (5000 units under the skin of the abdomen 2 times a day) or fraxiparin can be administered.
Surgical treatment of aneurysms is the main method and can be carried out in the form of open operations or intravascular interventions. In 1931, the English neurosurgeon Dot was the first to wrap an aneurysm with muscle, and in 1937, Dendy clipped the neck of the aneurysm with a specially designed self-clamping clip with favorable results. The first operations for arterial aneurysms in the CIS were performed in 1959 in Leningrad by Professor B.A. Samotokin, V.A. Khilko, and in Minsk - E.I. Zlotnik. Transcranial surgery is performed in the first 3 days after aneurysm rupture (acute period), if the patient’s condition allows. If no operation is performed during this period, then the next date for surgical intervention is the 5th and subsequent weeks after the rupture of the aneurysm (cold period).
In the 1970s prof. F. Serbinenko proposed a new method for treating arterial aneurysms, called intravascular ballooning. The method involves percutaneous needle puncture of the internal or common carotid artery. Through this needle, a fluoroplastic catheter with a dischargeable balloon at the end is inserted into the vessel, which is inserted into the saccular aneurysm under the control of the electron-optical converter of the X-ray machine. After the liquid polymer (silicone) introduced into the balloon hardens, the balloon is discarded and the catheter is removed. This technique allows you to turn off the aneurysm from the blood circulation. This treatment method has become widespread in all neurosurgical clinics around the world.
In the 1980s, a more advanced technique for intravascular occlusion of saccular aneurysms using metal coils was proposed.
Many patients who have had subarachnoid hemorrhage and undergo surgery may still have some kind of neurological deficit. Ischemic brain damage due to reactive vasospasm can be reduced by timely use of heparin and early use of the calcium antagonist nimodipine 90 mg orally every 4 hours. If stupor and confusion persist, recovery of movements is delayed, gliatilin, nootropic drugs, cortexin and other peptides are prescribed. Secondary communicating hydrocephalus requires shunting of the ventricular system of the brain.
Forecast. With the first hemorrhage from an aneurysm, the mortality rate is about 60%; another 15% of patients die if they rupture again in the next few weeks. After 6 months The chance of re-rupture is about 5% per year. In general, the prognosis for cerebral aneurysms is very serious. It is somewhat better for bleeding from arteriovenous malformations and is most favorable in cases where cerebral panangiography does not reveal an aneurysm, which indicates independent closure of the source of bleeding (self-healing of the aneurysm).
Complications of SAH
Analysis of the results of transcranial Doppler sonography showed that subarachnoid hemorrhage is almost always complicated by spasm of cerebral vessels. However, clinically significant spasm is observed, according to various sources, in 30-60% of patients. Cerebral vasospasm usually develops within 3-5 days. SAH and reaches a maximum on days 7-14. Its degree directly correlates with the volume of blood shed. In 20% of cases, primary subarachnoid hemorrhage is complicated by ischemic stroke. With repeated SAH, the incidence of cerebral infarction is 2 times higher. Complications of SAH also include concomitant hemorrhage into the brain parenchyma and breakthrough of blood into the ventricles.
In approximately 18% of cases, subarachnoid hemorrhage is complicated by acute hydrocephalus, which occurs when the outflow of cerebrospinal fluid is blocked by the resulting blood clots. In turn, hydrocephalus can lead to swelling of the brain and dislocation of its structures. Somatic complications include dehydration, hyponatremia, neurogenic pulmonary edema, aspiration or congestive pneumonia, arrhythmia, myocardial infarction, decompensation of existing heart failure, pulmonary embolism, cystitis, pyelonephritis, stress ulcer, and GI bleeding.
Clinical picture of subarachnoid hemorrhage
This condition develops rapidly against the background of a person’s normal well-being and manifests itself:
- sharp acute headache, worsening with the slightest physical activity;
- nausea, vomiting;
- convulsions;
- psycho-emotional disorders (fear, agitation, drowsiness);
- increased body temperature (up to febrile and subfebrile levels);
- disorders of consciousness (from stupor to fainting, coma);
- symptoms of damage to the oculomotor nerve (gaze paresis, drooping eyelid), hemorrhage in the eyeball.
In half of the cases, this condition leads to death. The main complications and consequences of subarachnoid hemorrhage:
- spasm of cerebral vessels caused by ischemia;
- recurrence of an aneurysm episode (may occur early or several weeks after the first episode);
- hydrocephalus (in the initial stages or in the late period);
- pathologies caused by subarachnoid hemorrhage in the brain (myocardial infarction, pulmonary edema, bleeding from a stomach or duodenal ulcer).
Among the long-term consequences of subarachnoid hemorrhage in the brain: memory disorders, attention, psycho-emotional disorders (depression, insomnia, agitation). Also, a standard complaint of patients who have suffered this condition is headache. Somewhat less frequently, hormonal disorders develop in the hypothalamic and pituitary gland systems.
Diagnostics
A typical clinical picture allows a neurologist to suspect subarachnoid hemorrhage. In the case of atypical forms, early diagnosis of SAH seems very difficult. All patients with suspected subarachnoid hemorrhage undergo a CT scan of the brain. The method makes it possible to reliably establish a diagnosis in 95% of SAH; identify hydrocephalus, bleeding into the ventricles, foci of cerebral ischemia, cerebral edema.
- Visualization techniques. Detection of blood under the arachnoid membrane is an indication for cerebral angiography to determine the source of bleeding. Modern non-invasive CT or MRI angiography is performed. In patients with the most severe degree of SAH, angiography is performed after their condition has stabilized. If the source of bleeding cannot be determined, repeat angiography is recommended after 3-4 weeks.
CT scan of the brain. Hyperdense blood in the subarachnoid liquor spaces
- Lumbar puncture. If subarachnoid hemorrhage is suspected, it is performed in the absence of CT and in cases where, in the presence of a classic clinical picture of SAH, it is not diagnosed by CT. Detection of blood or xanthochromia in the cerebrospinal fluid is an indication for angiography. In the absence of such changes in the cerebrospinal fluid, another cause for the patient’s condition should be sought.
- Ultrasound methods. Transcranial Doppler Doppler Doppler Doppler and Doppler Doppler Doppler Doppler (USD) of cerebral vessels make it possible to detect vasospasm in the early stages of SAH and monitor the state of cerebral circulation over time.
During diagnosis, subarachnoid hemorrhage should be differentiated from other forms of stroke (hemorrhagic stroke, TIA), meningitis, meningoencephalitis, occlusive hydrocephalus, traumatic brain injury, migraine paroxysm, pheochromocytoma.
Subarachnoid hemorrhage. Causes. Symptoms. Diagnostics. Treatment.
Subarachnoid hemorrhage is sudden bleeding into the subarachnoid space.
Etiology and pathogenesis
Spontaneous, or primary, subarachnoid hemorrhage (SAH) usually occurs from the rupture of an aneurysm of the superficial vessels of the brain. Less commonly, it is associated with atherosclerotic or mycotic aneurysm, arteriovenous malformation, or hemorrhagic diathesis. In cases of traumatic brain injury, subarachnoid hemorrhage is common, however, it is inferior in its clinical significance to other consequences of brain contusion.
In approximately half of the cases, the cause of intracranial hemorrhage is cerebral aneurysms. They can be congenital or acquired. Externally, an aneurysm often has a saccular appearance, in which a neck, body and bottom are distinguished. Typically, the diameter of the vascular sac ranges from a few millimeters to 2 cm. Aneurysms larger than 2 cm in diameter are considered giant. They occur equally often in men and women.
Aneurysm ruptures usually occur between the ages of 25 and 50 years (in approximately 91% of cases). Unruptured aneurysms occur in 7-8%, and asymptomatic aneurysms occur in 0.5% of people. Aneurysm rupture almost always occurs in the area of its bottom, where under magnification one can often see pinpoint holes covered with thrombotic masses. The favorite localization of aneurysms is the site of division of vessels of the 1st and 2nd order into branches. The most common localization of aneurysms is the supraclinoid section of the internal carotid artery (30-34%), anterior cerebral, anterior communicating artery - 28-30%, middle cerebral artery -16-20%, vertebrobasilar system - 5-15%. Multiple aneurysms occur in 20% of cases.
With subarachnoid hemorrhage, on the 3-4th day, due to prolonged spasm of the large arteries of the base of the brain, relatively diffuse cerebral ischemia develops, which leads to post-hemorrhagic impairment of cognitive functions (lethargy, dementia). A secondary increase in intracranial pressure and increased headache are often observed.
Clinical picture
In the clinical course of a cerebral aneurysm, three periods are distinguished: pre-hemorrhagic, hemorrhagic, post-hemorrhagic. In the pre-hemorrhagic period, the disease does not manifest itself in half of the patients with cerebral aneurysms. Other patients during this period may experience a local headache in the forehead and eye sockets (like a migraine). Episodes of headache with meningeal symptoms are possible (lasting from several hours to 1-2 days). These symptoms appear more often in people over 40 years of age. Other manifestations may include epileptic seizures of unknown origin, as well as transient dysfunction of the nerves adjacent to the aneurysm: diplopia, strabismus, anisocoria (with compression of the III, IV, VI pairs of cranial nerves), prosopalgia (compression of the V pair), facial hemispasm (compression of the VII pair ). Reduced visual acuity and bitemporal visual field defects are the result of pressure on the chiasm, and transient homonymous hemianopsias are caused by compression of the optic tract. Such patients are often diagnosed with ophthalmic migraine.
The hemorrhagic period lasts 3-5 weeks. after the breakup. The rupture of an aneurysm is usually accompanied by an acute, intense headache, often with a feeling of heat (“like boiling water pouring under the skull”). At the moment of rupture or immediately after it, there is often a short-term loss of consciousness (total spasm of the superficial vessels of the brain with shutdown of the function of the reticular formation of the brain stem and hypothalamus). Sometimes a cerebral coma develops, but more often the patient is in a state of stunning. Blood poured into the cerebrospinal fluid irritates the meninges and increases intracranial pressure, which is manifested by headache, nausea, vomiting, dizziness, bradycardia, and slow breathing. Epileptic seizures are possible. Rigidity of the neck muscles and Kernig's sign begin to appear one day after the subarachnoid hemorrhage. During the first 5-10 days, body temperature rises. About a quarter of patients develop focal and conduction symptoms (paresis, pathological foot signs), speech disorders, memory, etc., which is associated either with spasm of the corresponding cerebral artery, or with the penetration of blood into the medulla (subarachnoid-parenchymal hemorrhage). In patients with diagnosed aneurysms who have not undergone surgical treatment, recurrent bleeding often occurs, especially if bed rest is not observed in the first 3-4 weeks. after subarachnoid hemorrhage.
Depending on the location of the ruptured aneurysm, a characteristic clinical picture appears.
When a supraclinoid aneurysm ruptures, superior orbital fissure syndrome occurs. Its clinical picture is associated with damage to the oculomotor nerve (III pair): ptosis, dilation of the pupil, impaired movements of the eyeball up, inward, downward, local pain in the fronto-orbital region (I branch of the V nerve), central scotoma in the visual field, sometimes blindness .
When an aneurysm ruptures, localized in the anterior cerebral - anterior communicating arteries, disorders of consciousness, mental disorders, motor aphasia, paresis of the distal parts of the lower limb on one side with Babinski's symptom appear.
Rupture of a middle cerebral artery aneurysm is accompanied by hemiparesis (hemiplegia), hemianesthesia, hemianopsia and aphasia.
Rupture of an aneurysm of the vertebrobasilar system is characterized by the appearance of general cerebral symptoms, damage to the caudal group of cranial nerves, cerebellar, brainstem symptoms with respiratory failure, up to its stop.
The posthemorrhagic period includes residual neurological manifestations after hemorrhage. During this period, in patients who have suffered an internal cerebral hemorrhage, there is a high risk of repeated hemorrhages, which are more severe.
Diagnosis
Subarachnoid hemorrhage is diagnosed using a lumbar puncture, which reveals bloody (its color ranges from pink-red to cranberry juice) cerebrospinal fluid flowing under high pressure. After 6 hours or more from the moment of hemorrhage, the cerebrospinal fluid acquires a xanthochromic tint due to hemolysis of red blood cells. The presence of blood in the subarachnoid space can also be determined with a CT scan of the head. However, lumbar punctures are advisable not only for diagnostic, but also for therapeutic purposes. If repeated subarachnoid hemorrhage does not develop, the cerebrospinal fluid gradually clears and its composition returns to normal by about the 3rd week.
Acute subarachnoid hemorrhage sometimes mimics myocardial infarction, which may be facilitated by syncope and neurogenic changes on the ECG. When focal neurological symptoms appear, subarachnoid hemorrhage should be differentiated from parenchymal hemorrhage (parenchymal-subarachnoid hemorrhage), contusion or injury to the brain, subdural hematoma and hemorrhage into a brain tumor. Therefore, cerebral angiography and computed tomography are necessary both for differential diagnosis and for the purpose of planning surgical intervention. It is advisable to examine all 4 main arteries of the head, since there may be several aneurysms at the same time. Craniograms sometimes reveal calcification of the wall of an aneurysm or arteriovenous malformation.
Computed tomography or magnetic resonance imaging can detect the aneurysm itself if it is larger than 3-5 mm in diameter. In the hemorrhagic period, basal subarachnoid hemorrhage is visualized, which can be combined with intracerebral or intraventricular hemorrhage.
Forecast
With the first hemorrhage from an aneurysm, the mortality rate is about 60%; another 15% of patients die if they rupture again in the next few weeks. After 6 months The chance of re-rupture is about 5% per year. In general, the prognosis for cerebral aneurysms is very serious. It is somewhat better for bleeding from arteriovenous malformations and is most favorable in cases where cerebral panangiography does not reveal an aneurysm, which indicates independent closure of the source of bleeding (self-healing of the aneurysm).
Treatment
The patient is prescribed strict bed rest with the exception of any physical and emotional stress. It is necessary to ensure a sufficient supply of fluids and nutrients. For agitation, diazepam is prescribed; to reduce headaches, non-narcotic analgesics and codeine are prescribed.
Treatment of subarachnoid hemorrhage
Basic and specific therapy
Basic therapy for SAH consists of measures to normalize cardiovascular and respiratory functions and correct basic biochemical constants. In order to reduce hydrocephalus as it increases and relieve cerebral edema, diuretic therapy (glycerol or mannitol) is prescribed. If conservative therapy is ineffective and cerebral edema progresses with the threat of dislocation syndrome, decompressive craniotomy and external ventricular drainage are indicated.
Basic therapy also includes symptomatic treatment. If subarachnoid hemorrhage is accompanied by convulsions, anticonvulsants are included (lorazepam, diazepam, valproic acid); for psychomotor agitation - sedatives (diazepam, droperidol, sodium thiopental); for repeated vomiting - metoclopramide, domperidone, perphenazine. At the same time, therapy and prevention of somatic complications are carried out.
So far, subarachnoid hemorrhage does not have effective conservative methods of specific treatment that can stop bleeding or limit the amount of bleeding. In accordance with the pathogenesis, specific therapy for SAH is aimed at minimizing vasospasm, preventing and treating cerebral ischemia. The standard of therapy is the use of nimodipine and ZN therapy. The latter allows you to maintain hypervolemia, controlled hypertension and hemodilution, as a result of which the rheological properties of blood and microcirculation are optimized.
Surgery
Surgical treatment of SAH is optimal in the first 72 hours. It is performed by a neurosurgeon and is aimed at excluding the ruptured aneurysm from the bloodstream. The operation may consist of clipping the neck of the aneurysm or endovascular insertion of a balloon-catheter to fill its cavity. Endovascular occlusion is preferable in case of unstable patient condition, high risk of complications of open surgery, early vasospasm. With decompensation of cerebral vasospasm, stenting or angioplasty of the spasmed vessel is possible.
Prognosis and prevention
In 15% of cases, subarachnoid hemorrhage ends in death even before medical care is provided. Mortality in the first month in patients with SAH reaches 30%. In coma, mortality is about 80%, in repeated SAH - 70%. Patients who survive often have residual neurological deficits. The prognosis is most favorable in cases where angiography fails to identify the source of bleeding. Apparently, in such cases, spontaneous closure of the vascular defect occurs due to its small size.
The probability of repeated hemorrhage every day of the first month remains at 1-2%. Subarachnoid hemorrhage of aneurysmal origin recurs in 17-26% of cases, with AVM - in 5% of cases, with SAH of other etiology - much less frequently. Prevention of SAH involves treatment of cerebrovascular pathologies, TBI and elimination of risk factors.
You can share your medical history of what helped you in the treatment of subarachnoid hemorrhage.