Minor anomalies of cardiac development (MADC) include anatomical changes in the architecture of the heart and great vessels that do not lead to gross impairment of the function of the cardiovascular system. The etiological cause of minor anomalies in cardiac development is hereditarily determined connective tissue dysplasia, which has various clinical manifestations depending on the degree of gene penetrance. A number of minor anomalies may be dysembryogenetic in nature. The influence of various environmental factors cannot be excluded: physical, chemical exposure, disruption of microelement homeostasis, influence of geopathogenic zones.
Minor anomalies of the cardiovascular system, with a high genetic predisposition, include:
- mitral valve prolapse;
- additional trabeculae of the left ventricle;
The latter are characterized by an autosomal dominant type of inheritance.
MARS can disappear during ontogenetic development. These include:
- open oval window;
- elongated Eustachian valve;
The latter, after the neonatal period, usually decreases significantly in length and undergoes reverse development. The syndrome of prolapse of the mitral and tricuspid valves is also unstable.
To avoid subjectivity and subsequent overdiagnosis of MARS, their objectification is necessary through quantitative assessment. In cardiological practice, quantitative assessment is widely used to study the depth of mitral valve prolapse. Also, a quantitative approach is used to determine the length of the elongated Eustachian valve, dilatation of the great vessels, atrioventricular openings, and the number of additional trabeculae.
When it comes to classifying any structural defect in the heart as MARS, it must be remembered that the principle of assessment by functional significance is conditional. A bicuspid aortic valve usually does not lead to disruption of aortic blood flow, however, it is with this developmental anomaly that the incidence of sudden death is higher than in the population. It is well known that no matter what the heart tumor is: malignant, benign, it is malignant in its localization. For this reason, considering MARS only from the point of view of changes in organ structure is dangerous and extremely harmful. On the other hand, exaggeration of the functional significance of stigma in the heart is also not justified. In each specific case, the structural abnormality in the heart must be assessed prognostically.
Treatment of eustachitis
Treatment methods for eustachitis depend on the severity of the disease and the causes that provoked it. In this regard, it is imperative to inform the doctor about previous diseases and a tendency to allergies. Therapeutic measures to combat this disease have six main areas:
- Relieving swelling of the Eustachian tube. To reduce swelling of the mucous membrane of the nasopharynx and tube, respectively, doctors prescribe the use of vasoconstrictor drops: Sanorin, Vibrocil, Tizin, Nazol, Nazivin, etc. Mucolytic agents help eliminate the thick liquid that clogs the passage: Ambroskol, Sinupret and others.
- Relief of allergic reactions if they caused inflammation. For this purpose, they resort to the following drugs: Claritin, Desporatadine, Suprastin, Zodak, Citrine, etc.
- Elimination of the inflammatory process. To do this, use a solution of penicillin in ephedrine, which is instilled into the nose. This procedure helps restore the functions of the auditory tube and destroy the infectious pathogen, and has a bactericidal effect. Sometimes they resort to local hormonal agents: Nasonex, Avamys, etc., which have pronounced anti-inflammatory properties.
- Restoring the patency of the Eustachian tube involves blowing the ears using the Politzer method or using catheterization. They also resort to physical procedures (UHF, ultraviolet radiation), pneumomassage of the eardrum and laser therapy in the area of the mouth of the Eustachian tube. These measures are most often used in the stage when inflammation is eliminated, but hearing is not restored.
- Strengthening the overall immune system, because it is much more difficult for a weakened body to cope with the inflammatory process. Vitamins and immunomodulators are excellent helpers in the fight against any infection.
- Eliminating the cause of the disease. If necessary, foci of chronic infection are sanitized: removal of tonsils or adenoids, therapy with antibiotics, etc.
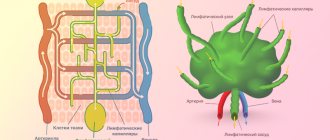
Tubular Duct Diagram
The narrow diagram of the eustachian tubes is part of a continuous system that includes the nose, palate, and nasopharynx. The nasopharynx is proximal to the eustachian tube, and the middle ear and mastoid deposits are located at its distal end. Directing inferiorly, anteriorly, and medially from the middle ear, the Eustachian tube opens approximately 25 cm posterior to and just below the posterior end of the inferior turbine. The Eustachian tube of an adult is at an angle of 45°, and in infants it is about 10°. Additionally, an infant's eustachian tube is approximately 18 mm long; The tube grows rapidly during childhood, reaching an adult size of 3–4 cm at the age of 7 years.
Only a doctor can identify the original cause of the disease, determine the path to recovery and the correct treatment methods. A lot, in turn, also depends on the patient: it is necessary to contact a specialist in time and follow all his recommendations.
Functionally narrow aorta
EchoCG criteria:
- Aortic diameter value corresponding to the 3rd to 10th percentile of the normal population distribution.
- No significant pressure gradient between the aorta and left ventricle.
When studying the diameter of the aorta in children from 3 to 15 years old in the population, we found a wide range of variations in this size. In this segment of ontogenetic development, the lumen of the aorta increases 1.5-2 times. A comparison of echometric indicators of the aortic root in 1800 children aged 3-15 years revealed a relationship between aortic diameter and anthropometric indicators. Correlation analysis made it possible to detect a relationship between diameter and child height (r=0.872 for boys, r=0.634 for girls) and, to a lesser extent, with body weight (r=0.574 for boys, r=0.532 for girls) and body surface area. The aortic diameter value corresponding to the 3rd - 10th percentile was found in 5.6% of children; no dependence on the age of the children was identified. This fact excludes the influence of physiological periods of intensive growth in ontogenesis on the representation of this trait in the population under study. Our data allows us to conclude that a narrow aorta is a genetically determined or congenital minor anomaly of the heart. None of the children showed clinical and/or hemodynamic signs of stenosis. According to Doppler examination of blood flow in the ascending aorta, there was no diagnostically significant increase in the pressure gradient, which averaged 1.3+0.07 m/sec. Children with a functionally narrow aorta have a characteristic functional-structural organization of intracardiac hemodynamics, so in 91.2% of boys and 95.4% of girls, borderline values of the diameter of the right ventricle were identified, corresponding to the 90th - 97th percentile. Left ventricular end-diastolic diameter tended to increase (90-97 percentile) in children under 7 years of age, while in older children it corresponded to the 25 percentile. On the contrary, the transverse diameter of the left atrium in children under 7 years of age usually corresponded to the 25-75 percentile; at older ages it increased and, in most cases, exceeded the 75 percentile.
In most cases, in children with a functionally narrow aorta, an increase in the muscle mass of the left ventricle was detected, as evidenced by the values of the diastolic thickness of the posterior wall of the left ventricle and the interventricular septum, corresponding to the 90-97 percentile. Thickening of the interventricular septum was observed in 35.1% of boys and 34.1% of girls, and thickening of the posterior wall of the left ventricle in 80.7% of boys and 88.6% of girls. A combination of a functionally narrow aorta with other cardiac anomalies—mitral valve dysfunction (25.7%), mitral valve prolapse (8.9%), and additional trabeculae in the left ventricular cavity (10.8%)—was noted.
Children with borderline low values of aortic diameter are predisposed to the occurrence of supraventricular and ventricular arrhythmias, as well as insufficient performance and exercise tolerance.
Characteristic functions of the organ
The throat and the body as a whole come under attack. That is why, in case of any viral or infectious pathologies, the doctor always tries to avoid further spread of the disease. This can be done taking into account the main functions that the auditory tube performs:
- Ventilation - the formation of balanced pressure on both sides of the eardrum. Even a minor change can have a negative impact on hearing acuity. In a healthy person, the process is regulated automatically by moving air flows from the tympanic cavity to the nasopharynx.
- Drainage - in a person without pathologies, the auditory tube removes excess accumulated edematous fluid.
- Protective is the most important of all the functional responsibilities of the body that guards human health. Throughout life, the Eustachian tube secretes mucus that has bactericidal characteristics. The immunoglobulin it contains acts as a natural barrier to infections or viruses. If the body is weakened under the influence of external or internal factors, the production of protective mucus is reduced.
All of the above speaks about the importance of the organ for a full human life. In this regard, even during a preventive visit to the doctor, she is examined. For this purpose, a special procedure is used - salpingoscopy. A painless examination allows the doctor to make sure that there are no pathological changes in the structure of the auditory tube.
If a patient is diagnosed with an ENT pathology of an infectious nature, then tympanomanometry is mandatory - measuring the pressure in the eardrum. A simple procedure will show whether the auditory tube has undergone pathological changes. Based on the material collected during diagnosis, a decision is made on the need for a therapeutic course.
The Eustachian tube, being an organ sensitive to various infectious viral agents, requires immediate treatment if there is a focus of inflammation. Any delay will give the disease the opportunity to spread further, causing pathologies of the throat, ears, nose and lungs. The activity of the spread of the disease depends on the ability of the immune system to resist.
Treatment of acute eustachitis
When the Eustachian tube becomes inflamed, it requires complex therapy. The treatment regimen depends on the results obtained after the diagnosis.
The otolaryngologist takes into account the patient’s condition, the degree of development of the inflammatory process, where the pathological focus is located and selects the most effective means. Treatment is carried out using traditional means; in the absence of serious contraindications, folk remedies can be used.
Drug therapy helps relieve tissue swelling, eliminate allergic reactions and inflammation, and also restore the patency of the auditory tube.
Patients are prescribed the following medications:
| Group of drugs | Name | Application |
| Vasoconstrictor nasal agents | Sanorin, Tizin | Medicines help to quickly relieve swelling. Adult patients are prescribed 1-3 drops in each nasal passage 3-4 times a day. The course of treatment depends on the severity of symptoms, on average it lasts 3-7 days. |
| Antihistamines | Fenistil, Loratadine | The products reduce the allergic reaction. It is recommended to take medications internally. The adult dosage is 2 drops per 1 kg of body weight per day, it should be divided into 3 doses. |
| Nasal saline solutions | Humer, AquaMaris | Medicines clear the mucous membrane of the eardrum of accumulated mucus. Prevent infection from entering the ear cavity. Reduce swelling of the mucous membrane. Sprays are recommended to be used 4-8 times a day. Inject the product 2-3 times into each nostril. The course of treatment lasts 2-4 weeks. |
| Antiviral agents | Derinat, Nazoferon | The drugs increase the body's immunity and slow down the proliferation of pathogenic flora. They also reduce inflammation, swelling and the risk of complications. The medicine is used 3-6 times a day. It is recommended to drop 3-5 drops into each nasal passage. The duration of therapy is 1-2 weeks. |
| Antibacterial drugs | Azithromycin, Ampicillin | Medicines are prescribed to patients in case of infection of the Eustachian tube. The drug should be taken before meals or after meals 1 time per day. The recommended dosage for an adult patient is 0.5 g for 3 days. |
| Hormonal agents | Nasonex, Avamis | The therapeutic dosage is 2 inhalations into each nasal passage once a day. |
Treatment of acute eustachitis lasts on average 3-7 days. The chronic form requires more time for therapy
It is important to strictly adhere to the recommendations and prescriptions of your doctor to prevent serious complications.
What are the dangers of having a damper in adults?
All minor anomalies in the development of the cardiovascular system do not cause significant hemodynamic (circulatory) disturbances. The increase in the frequency of detection of such pathology is associated with the spread of ultrasound diagnostics for children and adults, which makes it possible to identify deviations at an early stage.
According to recent studies in cardiology and general therapy, elongation of the eustachian valve by more than 1 centimeter is detected in 0.25% -0.50% of the population. In most cases, this occurs against the background of a state of complete health.
The presence of such a valve increases the risk of developing certain complications, since the main source of electrical impulses of cardiac contractility is located in the right atrium.
Reflex irritation of pacemaker (rhythm-introducing) cells can cause the following types of arrhythmia:
- Single extrasystoles. The most favorable option, which is not clinically manifested and does not require drug treatment.
- Tachycardia with a pulse rate of more than 90 beats per minute. Feels like frequent loud heartbeat, trembling and discomfort. Requires examination to identify the cause of the disorder and prescribe treatment.
- Intraatrial or interatrial disturbance of impulse conduction, blockade. Therapy is considered depending on the severity of symptoms.
- Paroxysmal rhythm disturbances are a variant of an unstable form of arrhythmia that occurs spontaneously in the form of attacks. Increases the risk of acute coronary complications and heart failure.
- Fluttering or flickering (fibrillation). The most dangerous type of disorder in which irregular irregular contractions can provoke thrombosis or cardiac arrest. Develops against the background of concomitant pathology.
Clinical symptoms occur only when several developmental anomalies are combined, or against the background of concomitant pathology that worsens the condition. Characteristic symptoms are: shortness of breath with difficulty breathing on exertion, weakness and pallor of the face, cyanosis around the nasolabial triangle, swelling.
Diagnostics
Laboratory tests reveal the presence of dysbacteriosis, as well as nonspecific bacteremia. Taken together, the phenomena indicate that the intestine has become the entry point for infection. Due to the transition of the pathology to a chronic form, lymphoid tissue throughout the gastrointestinal tract is also subject to negative effects. A blood test can detect deficiency of immunoglobulins A and M.
Of the instrumental diagnostic methods, irrigoscopy and manometry
. Normally, the pressure inside the colon is no higher than 10-20 mmHg. Art., during defecation it rises to 200 mm Hg. Art.
From the editor: Infarction of the anterior wall of the heart: types, symptoms, treatment consequences
In gastroenterology, they focus on the classification of ileocecal valve dysfunction.
The system is compiled taking into account the results of irrigoscopy:
• 1st degree - the reflux of the contrast suspension is visualized only into the terminal loop of the ileum. The stage is characterized by valve enlargement and pain on palpation. Emptying the colon from the contrast mass does not increase retrograde reflux.
• 2nd degree - the reflux of the contrast mixture into the ileum occurs simultaneously with the contrasting of 2-3 loops. There is a painful reaction to palpation. Increased pressure inside the lumen does not cause an increase in reflux.
• 3rd degree - the reflux of a large volume of contrast suspension into the ileum is visualized. It fills several loops at once and is combined with an enlargement of the lips of the ileocecal valve and deformation of both frenulums.
The disadvantages of irrigoscopy are significant radiation exposure to the patient, the lack of clear evaluation criteria and objective indicators of the disorder in question. Cases of false positive results are common. This diagnostic outcome is caused by the peculiarities of the procedure. The dome of the cecum is densely filled with a contrast mixture. As a result, there is a natural opening of the natural shutter. Excessive distension of the cecum is the result of deep palpation, massage and contraction during defecation. There is an assumption that dysfunction of the natural shutter is associated with connective tissue dysplasia. Therefore, we cannot exclude the possibility of developing oncology with insufficiency of the bauhinium valve.
Why is pathology dangerous?
The failure of the pylorus causes the reflux of more than a billion microbes from the large intestine into the small intestine. The phenomenon is extremely unfavorable for the condition of the body. There is a dense placement of foreign microflora on the walls of the small intestine. This creates convenient conditions for the progression of the process of rotting and fermentation inside it. The waste products of pathogens have a detrimental effect on the mucous membrane of the small intestine. These substances include phenol, cresol, carbolic acid, hydrogen sulfide, ethane. Immediately after absorption into the blood, the products provoke the phenomenon of autointoxication.
It is quite difficult for the body to remove them completely; the detoxification process becomes more complicated if a person has liver pathologies. As a result, the intestinal wall undergoes toxic, invasive, destructive changes. But most of all, microbes are predisposed to tissue death. In the absence of diagnosis and adequate treatment for a long time, the likelihood of degenerative and even necrotic processes within the mucous membrane is high. The intestinal wall loses its barrier function. The body becomes defenseless against microbial aggression.
Treatment
Therapy begins with nutritional correction - giving up fried, hard-to-digest foods, sour, spicy, smoked foods. Coffee, alcohol, carbonated drinks are contraindicated. Follow the regime - eat at the same time, at least 4 times a day, in portions of up to 400 g (depending on the type of food).
Limit exposure to stress factors, eliminate neurological disorders if present.
Drug treatment is aimed at eliminating primary valve dysfunction.
1. Magnesium orotate
– a drug that is a combination of magnesium and the non-steroidal anabolic orotic acid. The effect of the medicine is aimed at normalizing the absorption of this microelement by tissues. Magnesium orotate is prescribed orally: dosage – 1.0 g three times a day for 3 months. Then the prescription is adjusted - take 0.5 g 3 times a day for the next 3 months. Contraindications to the use of the drug are the presence of renal failure in the patient.
2. Drug therapy involves the administration of Proserin, Coordinax
– to stimulate motor skills by improving the tone of the digestive organs.
3. To relieve nausea (and, accordingly, the urge to vomit), intramuscular administration is prescribed Tserukala
.
4. Normalization of intestinal microflora occurs through the use of probiotics
.
5. Vitamins (C, B6, B2)
more often prescribed parenterally (the injection route allows for faster relief of hypovitaminosis).
Absolute insufficiency of the bauhinium valve is an indication for a surgical approach. Operations to normalize the condition of the ileocecal valve in case of its dysfunction are technically simple and safe. Modern surgeons perform them without opening the lumen of the digestive tract, thereby reducing the risk of postoperative complications.
A common technique for normalizing the diameter of the ileocecal valve is the application of staples to the lips of the valve during colonoscopy. In 99% of cases, complete clinical recovery occurs. The advantages of this method are that there is no need for heavy anesthesia, and there are no postoperative scars. Frequent anesthesia for the patient is not required (after traditional operations, an analgesic is administered at least once every 2 hours).
Conclusion
Insufficiency of the Bauginian valve is a condition that is difficult to identify without the use of diagnostic methods. It is at a doctor’s appointment, during an examination, that the presence of a disorder is confirmed. Signs of the disease resemble the manifestations of many other pathologies. The specialist conducts differential diagnostics, prescribes treatment, and gives recommendations regarding nutrition. The success of therapy largely depends on the professionalism of the gastroenterologist, but the timeliness of seeking medical help plays an important role.
The intestinal valve is a tightly closed fold of natural origin formed at the junction of the small and large intestines. Its functional purpose is to ensure the movement of intestinal contents in the direction from the ileum to the cecum. Insufficiency of the ileocecal valve (another name for this organ) causes the reflux of food masses in the opposite direction. The Bauginian valve, when its functionality is impaired, leads to congestion of the small intestine with the microflora of the large intestine and, as a consequence, its inflammation. Regular manifestation of this pathology causes a disease called chronic enteritis.
Traditional medicine and homeopathy for inflammation of the Eustachian tube
Often, unconventional methods lead to very good results, but before using them you should definitely consult a doctor. If the cause of eustachitis is an allergic reaction, the use of herbal remedies can be significantly harmful. There are also individual intolerances and side effects; only a competent doctor can take into account all the nuances and characteristics of the body.
The lumen of the tube will also increase with physical maturity. The Eustachian tube drains or clears secretions from the middle ear into the nasopharynx, protects the middle ear from changes and secretions in nasopharyngeal pressure, and ventilates the middle ear so that the pressure inside is equal to atmospheric pressure. Drainage of normal secretions from the middle ear to the nasopharynx through the eustachian tube is accompanied by mucociliary transport and repeated active opening and closing of the tubes. The four muscles associated with the eustachian tube are all directly or indirectly related to tubal function.
The most popular traditional medicine for inflammation of the auditory tube:
- Herbal decoctions. Use calendula, chamomile, oak bark. These potions are quite easy to prepare: two tablespoons of the dry mixture are brewed with a glass of boiling water and infused for two hours. The slightly heated mixture is dripped into the nostril or ear. These plants are considered excellent antiseptics and will help relieve inflammation faster.
- Aloe and agave juices diluted with a small amount of warm boiled water are recommended to be dripped into the nose and used to rinse the ears.
- Boiled potatoes are a well-known remedy for colds, and they are also effective for eustachitis. Application: boil the potatoes and breathe over the steam, covered with a towel for several minutes.
- Garlic. This is an excellent remedy in the fight against infection; you need to grind it to a paste consistency, add vegetable oil and leave for two weeks. The resulting infusion is dripped into the ears and nose.
- Wrap chopped onions into porridge in a piece of gauze and insert into the affected ear for 10 minutes. Repeat the procedure for one to two weeks, once a day.
- Among homeopathic medicines for inflammation of the eustachian tubes, Phytolyacca, Silicea and Damask rose are widely used.
Editorial: Amyloidosis
Traditional recipes are recommended to be used in conjunction with conservative therapy; you should not rely entirely on them, neglecting the doctor’s prescriptions. Yes, and it is unlikely that you will be able to establish the original cause of inflammation on your own; therefore, there is a high probability that you will suppress the disease, but not get rid of it completely.
Normally closed at rest, the eustachian tube opens when we yawn, sneeze, swallow or chew, allowing air to enter the middle ear and mucus. It also promotes proper function of the tympanic membrane, allowing the middle ear and atmospheric pressure to equalize. The fatty lining of Ostmann, located in the inferolateral aspect of the eustachian tube, is thought to play a role in sealing the tube to prevent backflow of nasopharyngeal secretions and likely helps protect the tube.
This results in higher air pressure outside the eardrum than in the middle ear, which can cause long-term damage to the tube. Anatomical abnormalities such as cleft palate and other craniofacial abnormalities can lead to inflammation of the eustachian tube venting pattern.
The auditory, or Eustachian, tube (ST) is part of the middle ear system, the connecting link between the tympanic cavity, the nasopharynx and the nasal cavity. Representing a single system of the middle ear, the TA itself plays an important role in aeration, regulation of pressure in the tympanic cavity, drainage function and in the sound conduction system [1].
According to 2021 WHO data, approximately 32 million children suffer from disabling hearing loss. About a third of patients with hearing loss have problems with CT function. The prevalence of eustachian tube dysfunction (ETD) is about 40% among children under 10 years of age [2], and in adults it ranges from 1 to 5% [3].
TS develops from the pharyngeal pouch of the first gill cleft [4]. The pharyngeal pouch is an endoderm surrounded by a mesenchymal base. Blood vessels and nerves gradually grow through the mesenchymal base, providing a framework for the further development of muscles and the cartilaginous skeleton. The first gill cleft remains undifferentiated until the 6th-8th week of embryonic development. Subsequently, its sections are separated into a slit-like tympanic cavity and a more elongated part that opens into the pharyngeal cavity—ST [5]. By the 6th month of gestation, the bone part of the CT begins to form. By the end of the third trimester of pregnancy, the CT is fully formed and is divided into 2 sections - bone and cartilaginous. In the period from the 35th week of pregnancy to the moment of birth, the CT increases in length by approximately 2 times. In a newborn, the length of the CT is about 20.5 mm, the length of the bone and cartilage sections is 6.8 and 13.6 mm, respectively [6]. Prosvet S.T. averages 2 mm in the fetus for 5 months and remains the same at the time of birth. From the moment of birth to 12 months, the lumen increases towards the pharyngeal and tympanic openings, forming the isthmus of the auditory tube - isthmus tubae autivae
.
The CT is an elongated cone, open medially and downward, consisting of two sections: bone and cartilaginous. One end of the CT opens on the anterior wall of the tympanic cavity, the other on the lateral wall of the nasopharynx. Both sections form an obtuse angle with each other and connect to form the narrowest part of the CT - the isthmus. The area of the isthmus at birth is about 0.9 mm2 in diameter, increasing to 1.6 mm2 in an adult. It controls air flow, similar to a valve.
In children, the length of the tuba auditiva
varies depending on age. According to A.G. Nikhinson [7], the length of the CT at the age of 0 to 3 months is 23.6 mm, from 3 to 6 months - 25 mm, from 6 to 9 months - 26.5 mm, from 3 to 12 months - 27 mm, from 1 year to 2 years - 30.8 mm, from 2 to 3 years - 34.3 mm, from 3 to 5 years - 36 mm, from 5 to 10 years - 36.8 mm and from 10 to 14 years - 39, 5 mm. According to N.A. Yakutkina [6], M.Yu. Boboshko and A.I. Lopotko [8], the length of the CT uniformly increases with age, corresponding to the growth of the skull. Length S.T. in adults it is about 36 mm, of which 12 mm is the bone part, and about 24 mm is the cartilaginous part.
According to its shape, the CT is divided into 3 main types: straight, S-shaped and S-shaped with a downward slope. In children under 2 years of age, the form of TS is in most cases direct [6, 7]. A.G. Nihinson [7] noted the difference in the length, size of the lumen and shape of the CT in one person on the right and left. These studies may indirectly explain the predominant localization of otitis on the side where the narrowing of the lumen of the VT is noted.
The CT in an adult is directed downwards and medially, forming an angle with the horizontal plane of 30-40° [8, 9], in children this angle does not exceed 10° [6].
The ratios of the lengths of the bone and cartilaginous parts also change: in children the cartilaginous part grows more intensively [6], while at the same time K. Ishijima et al. note more active growth of the bone part [10]. The bony part of the Eustachian tube opens into the tympanic orifice into the cavity of the middle ear. The height of the orifice is about 4.5 mm, the width is 3.3 mm [11]. The cartilaginous section opens with the pharyngeal orifice on the lateral wall of the nasopharynx at the level of the posterior end of the inferior turbinate. In children, the lumen of the CT in the cross section of the cartilaginous part is slit-like, and in the bone part it is oval. In an adult, the bony part is triangular in shape, and the cartilaginous part is slit-like and is in a collapsed state [11]. The cartilaginous part is a groove curved in the shape of a hook. The anterior outer wall of the cartilaginous section serves as the attachment point for the tensor soft palate muscle.
At the pharyngeal mouth of the ST there is a tubar cushion - torus tubarius
, represented by the edge of the tubar cartilage.
The tubar ridge is movable and surrounds the orifice from behind and above. Anteriorly, the opening is limited by a fold of mucous membrane ( plica salpingopalatina
), called the fold of Tortual [12]. Posterior to the tubar ridge on the lateral wall of the nasopharynx there is a depression - the pharyngeal pocket, or Rosenmüllerian fossa, in which there is an accumulation of lymphadenoid tissue - the tubar tonsils. Tubar tonsils are formed in utero and are finally formed by the age of 3 years [12].
CT in its cartilaginous part correlates with 4 muscles: tensor soft palate ( m. tensor veli palatini
), levator soft palate (
m. levator veli palatini
), tubopharyngeal (
m. salpingo-pharyngeus
) and tubopalatine (
m. salpingo-palatini
).
The muscles of the lateral wall of the nasopharynx and soft palate can change the size of the pharyngeal orifice of the CT and affect the aeration of the middle ear cavity. So the muscle that tenses the soft palate ( m. tensor veli palatini
), with its deep fibers, expands the lumen of the CT [13].
V.T. Palchun and N.A. Preobrazhensky in 1978 [14] noted the antagonistic effect of m .
tensor veli palatini : when the soft palate is tensed and stretched to the sides, the mouth of the ST expands and the upper third of the lumen opens, but in the rest of the tube the lumen narrows.
The muscle that lifts the soft palate ( m. levator veli palatini
) “presses” the lower edge of the posterosuperior wall of the tube, which also expands the lumen of the cartilaginous part.
The tubopharyngeal muscle ( m. salpingo-pharyngeus
) pulls the pharyngeal opening somewhat posteriorly and downward [14].
Innervation m . tensor veli palatini
comes from the mandibular branch of the trigeminal nerve, and
m.
levator veli palatini - from the pharyngeal branch of the vagus nerve [14]. The trigeminal, vagus, glossopharyngeal and facial nerves take part in the sensitive innervation of the CT. According to a study by J. Terracol et al. [12], dissection of the glossopharyngeal nerve leads to complete anesthesia of the mucous membrane of the ST, which indicates the predominant sensory innervation of the ST by the IX pair of cranial nerves.
Autonomic innervation has been studied by many researchers [15]. Sympathetic branches to the ST come from the pterygopalatine and auricular ganglia, glossopharyngeal, tympanic and carotid-tympanic nerves. Parasympathetic innervation is carried out through the tympanic branch of the glossopharyngeal nerve. There is a correlation between the sympathetic and parasympathetic nervous systems. So, T.V. Klimantseva [16] assessed the vegetative status of patients with chronic tubular dysfunction, and 70.8% of patients with vasmotor tubopathies had parasympathicotonia.
The blood supply to the CT is provided by the deep auricular branches of the internal maxillary artery, the ascending pharyngeal and ascending palatine arteries.
The main functions of the CT are ventilation, protective, drainage and acoustic.
The ventilation function allows you to maintain pressure in the middle ear that is optimal for sound transmission to the structures of the inner ear. This regulation occurs through the opening and closing of the ST. At rest it is closed and opens only during swallowing, yawning, sneezing, blowing the nose, but not every time [12,17]. Closing S.T. occurs passively, due to elastic traction. Compliance S.T. due to the condition of the cartilaginous structures and the condition of the mucous membrane lining its inner wall. The mucous membrane seems to “stick together” throughout. The tone of the tubar muscles, the condition of the peritubar tissues and the level of venous pressure play a certain role [17].
The opening of the ST is a complex physiological process carried out by a complex reflex mechanism and depends on the contraction of the pharyngeal muscles. Many studies talk about alternating contraction of the tubar muscles. First, m . tensor veli palatini
, and then
m. levator veli palatini. Musculus levator veli palatini
is responsible for opening the pharyngeal orifice of the ST, displacing it posteriorly and medially, and
m .
tensor veli palatini opens it completely [18]. Normally, the ST opens with a frequency of 1 time per minute during wakefulness, every 5 seconds during chewing and swallowing, and every 5 minutes during sleep [19]. The average time for its opening in an adult is from 0.1 to 0.9 s [19]. In children, the act of swallowing is not so rhythmic and by the age of 11 it reaches the time of opening of the ST in an adult. The active opening of the duct provides a ventilation function, but also plays a protective role in the event of infection from the nasopharynx [20]. An important aspect of the ventilation function is the equalization of pressure in the tympanic cavity. Normal intradrum pressure is considered to be fluctuations from –50 to +50 mm water column. [21].
The ventilation function in children is reduced due to high values of negative pressure in the tympanic cavity. At the ages of 3 to 5 years, the pressure is more negative than at the ages of 9 to 12 years. According to J. Jerger, pressure in the middle ear ranges from 0 to –170 mm water column. [21].
The drainage function ensures the outflow of secretions from the tympanic cavity and is carried out due to mucociliary clearance and contraction of the peritubar muscles [22]. The mucociliary system begins to develop in utero and functions immediately after birth [23]. The mucociliary system is a system of ciliated and goblet cells covered with mucus - mucous blanket
. Mucus consists of sol and gel. Gel - the outer layer of mucus - is more elastic and viscous. The inner layer, the sol, ensures the beating of the cilia of the ciliated epithelium. Mucociliary clearance changes under the influence of cytokines, prostaglandins and leukotrienes, indicating a relationship with inflammatory and allergic components of the mechanism of TS dysfunction [24].
Currently, there are no clear criteria for tubular dysfunction. In 2014 in Amsterdam, at the “Pathology of the Eustachian Tube” forum, acute (up to 3 months), chronic (more than 3 months) and obstructive forms of DST were identified. The latter manifests itself against the background of changes in pressure and gaping of the CT [22]. T.I. Garashchenko et al. There are 3 types of DST: gaping, obstructive and reflux dysfunction [25, 26].
In the ICD 2021 edition, this classification corresponds to: H 69.8 - other specified lesions of TS; H 69.9 - unspecified TS lesions; H 68.1 - compression, stenosis, stricture of the auditory tube, dysfunction due to barotrauma, gaping ST - H 69.0 [22].
The etiological factors contributing to the development of chronic DST are multifaceted and are divided into inflammatory, allergic, vasomotor, congenital malformations, obstruction by lymphadenoid or tumor tissue.
DST often occurs against the background of chronic rhinitis and rhinosinusitis. Research by NF Stoikes, JM Dutton [27] showed that “endoscopic” treatment of the paranasal sinuses brings relief and improvement in the function of the auditory tube.
Allergic rhinitis and allergic inflammation of the upper respiratory tract increase the level of leukotrienes C4 and D4, which inhibit mucociliary clearance of the mucous membrane of not only the upper respiratory tract, but also the Eustachian tube [24], which in turn leads to disruption of the drainage function and changes in the mucociliary activity of the ciliated epithelium. A. Tanaka et al. [28] proved that local and systemic allergic responses increase the rate of ciliary transport, but cause damage to the mucous membrane.
Obstructive dysfunction can be caused by several reasons: anatomical occlusion, hyperplastic lymphadenoid tissue or a tumor process; muscle dysfunction due to neurovegetative disorders; functional obstruction due to allergic or infectious inflammation of the upper respiratory tract. In childhood, one of the common causes of obstructive dysfunction is hypertrophy of the pharyngeal and tubal tonsils [29].
As mentioned above, many researchers note the connection of the autonomic nervous system with the function of TS based on the relationship between the syndrome of autonomic dysfunction and the development of DST [8, 19, 29].
Gastroesophageal reflux can also be one of the causes of DST. Pepsin, hydrochloric acid and other components of gastric juice can enter the CT and tympanic cavity and cause pathological changes, as has been shown in animal experiments [31]. According to M. Crapko et al. [32], detection of Helicobacter pylori
and pepsin in the middle ear correlates with episodes of reflux.
Reflux-DST, according to V.P. Karpova et al. [33], occurs with a low position of the pharyngeal mouth of the duct and hypertrophy of the tubal ridges, is more common in children, and is characterized by pathological reflux of secretions, pathogenic microorganisms, and gastric contents into the duct from the nasopharynx with concomitant gastroesophageal reflux. Confirmation of this type of DST is the detection of gastric enzymes, hydrochloric acid, and Helicobacter pylory
[34, 35].
We must not forget about hereditary diseases. In Pierre Robin and Treacher Collins syndromes, in 79% of cases there are clinical manifestations of DST [36], due to the horizontal position of the CT, underdevelopment of the facial skeleton and improper functioning of the tubar muscles.
DST against the background of changes in pressure, or baric tubootitis, occurs due to changes in atmospheric pressure. Against the background of rapid changes, pressure equalization in the tympanic cavity does not have time to occur, hemorrhages and intratympanic extravasation, swelling and inflammation in the CT and tympanic cavity occur.
Gaping ST is a pathologically open ST. As mentioned above, the CT opens during swallowing and yawning. Constant gaping of the tube (patulous Eustachian tube) can be caused by atrophy of the mucous membrane of the upper respiratory tract, systemic diseases (amyotrophic lateral sclerosis, syphilis), rapidly developing weight loss, tumor growth into the paratubar tissue, hypertonicity of the tubular muscles [17]. A number of authors believe that such dysfunction can contribute to the development of exudative otitis media [14].
You can suspect DST in a patient based on characteristic complaints: ear congestion, sensation of “clicking”, “gurgling”, “being under water”, discomfort, pain in the ear, autophony, muffled sounds and subjective ear noise.
According to M.Yu. Boboshko [30], these complaints occur with the following frequency: hearing loss - in 84% of patients; a feeling of muffled sounds and congestion - in 80.8%; noise in the ear - 78.2%; autophony - in 52.6%; ear pain - 48.7%; changes in hearing depending on the position of the head - in 21.8% of those examined. Often the main and only complaint may be discomfort in the ears during takeoff and landing of an airplane. As a rule, the described symptoms persist for more than 3 months. It is typical that complaints do not go away after swallowing, chewing and yawning [8, 30].
The authors declare no conflict of interest.
The authors declare no conflict of interest.
Information about authors
Ivoilov A.Yu. - e-mail; https://orcid.org/0000-0001-6370-6068
Garov E.V. - e-mail; https://orcid.org/0000-0003-2473-3113
Bodrova I.V. - e-mail; https://orcid.org/0000-0002-0523-2340
Yanovsky V.V. - e-mail; https://orcid.org/0000-0002-1702-4282
Sudarev P.A. - e-mail; https://orcid.org/0000-0001-9085-9879
Morozova Z.N. - e-mail; https://orcid.org/0000-0002-2964-7487
Martirosyan T.G. — e-mail; https://orcid.org/0000-0003-2161-8718
Ibragimova Z.S. — e-mail
Author responsible for correspondence: Morozova Z.N. — e-mail: [email protected]
How to clean the electronic throttle body without removing it from the car
Experts recommend servicing electronically controlled throttle valves at least once a year or every 20 thousand kilometers. It is better to perform the damper cleaning procedure before the onset of autumn rains, for which there is a logical explanation. The fact is that due to the increased humidity of the incoming air, dirt deposits on the drive parts, axle and damper soften. Because of this, the throttle sticks, which makes it impossible to control engine speed and can cause an accident.
On most foreign and domestic cars, the electronic gas pedal drive is installed directly in front of the intake manifold. The accessibility of the mechanism and the ease of its maintenance make it possible to carry out preventive maintenance in literally 15-20 minutes.
For this you will need:
- carburetor cleaner (replaced with gasoline, kerosene, diesel fuel, etc.);
- silicone lubricant in the form of a spray;
- rags;
- a screwdriver with a flat or Phillips blade (depending on the type of screws used to secure the air supply pipe);
- a brush with stiff bristles or a toothbrush;
- protective gloves.
It is better to do the work sequentially - this way you will avoid mistakes and be sure that you did everything correctly:
Using a screwdriver, loosen the clamps securing the air supply pipe and disconnect the corrugated hose from the body of the electronic accelerometer.
Press the throttle valve, turn it 90 degrees and conduct an external inspection. Dirt and grime on the walls of the case are sufficient reason to begin cleaning immediately. Tar and soot deposits primarily clog the gap required for the engine to idle. Because of this, the speed becomes unstable or the power unit completely stalls due to the loss of air supply. In addition, touching the valve to a thick layer of carbon deposits causes it to jam and contributes to increased wear of plastic gears and other drive parts.
Lock the throttle in the open position. To do this, place an object made of wood or plastic of suitable thickness between the damper and the inner wall of the case - for example, the handle of the same screwdriver.
When starting to clean the unit, generously moisten the inner walls and damper with detergent.
Pay special attention to those places in the throttle chamber through which the valve axis passes - the tar deposits accumulating there are precisely the reason for the rotation unit jamming. As a result, the throttle turns jerkily and makes driving uncomfortable.
After waiting 10-15 minutes to soften the blockages, they are removed with a brush
If necessary, the process is repeated many times, achieving complete cleaning of the throttle. Keep in mind that on some car models the throttle chamber walls are coated with a special molybdenum coating. The extremely smooth layer promotes laminar air flow in the channel and prevents soot from settling. Do not confuse this coating with carbon deposits and do not try to remove it. On the contrary, use gentle cleaning methods and abandon the hard brush in favor of a soft flannel cloth.
After achieving a soft, even shine from the walls of the inner chamber, clean the front and rear sides of the throttle valve. Wipe parts and surfaces dry with a rag. Additionally, blow out the assembly with compressed air.
After cleaning the throttle body to ensure that the electronic throttle pedal operates smoothly and smoothly, apply silicone lubricant to the axle, the throttle body and the part of the throttle chamber that it connects to.
Attach the air duct and tighten its fastening clamps.
After intervention in the unit, the throttle valve position parameters will change, so in some cases it is trained. If the idle speed begins to change spontaneously (“float”, as auto mechanics say), then reset the volatile memory of the controller by briefly disconnecting the “positive” terminal from the battery.
Something else useful for you:
- Replacing oil seals (valve seals)
- How to remove the cylinder head on an engine
- Installing cylinder heads
And the last thing I would like to remind you: when starting for the first time, do not press the gas pedal until the engine warms up. By ensuring the engine operates at rated speed over a wide temperature range, you will allow the controller to adapt to changing conditions and set the optimal idle settings. In the future, this will make it possible to operate the car without any surprises from the throttle assembly.
Seal
Additional trabeculae in the left ventricular cavity
Can be single or multiple. Additional trabeculae are identified in 16% of autopsies.
EchoCG criteria
Two-dimensional echocardiography
- An echo-dense linear formation, detected in two sectional planes and having no connection with the valve apparatus.
- Using two perpendiculars in the long axis projection, drawn at the level of the papillary muscles and the free edges of the mitral valve, the cavity of the left ventricle is conventionally divided into three sections. The classification of trabeculae is based on the criterion of attachment of their ends to the walls of the left ventricle. If the attachment points are located in one section, then the trabecula is transverse, if in adjacent sections, then diagonal, and when the trabecula passes from the apical to the basal section, it is longitudinal.
Transverse localization of trabeculae of the left ventricle is interpreted as the most arrhythmogenic, since it can be an additional path of impulse conduction, and therefore can provoke premature ventricular excitation syndrome in the form of two variants: WPW syndrome and shortened PQ interval syndrome. Diagonal or longitudinal arrangement does not lead to disruption of the functional characteristics of the left ventricle, but is often accompanied by a systolic heart murmur, simulating a congenital heart defect.
Classification
The disease is classified according to several criteria.
Flow form:
- Acute tubo-otitis. Active inflammation that develops when the infection moves from the nose or throat. Acute tubo-otitis is manifested by severe swelling of the auditory tube and severe symptoms. Timely treatment ensures a quick recovery.
- Chronic turbootitis is a protracted form of the disease, when the symptoms are mild, but atrophic and sclerotic processes in the eustachian tube are noted. The danger of this form of the disease is that it affects the eardrum and cavity. As a rule, in the chronic form, the membrane becomes distorted and becomes cloudy.
Origin of the disease:
- Infectious eustachitis. The disease is associated with the transfer of infection from the throat or nose.
- Consequence of barotrauma. The disease occurs due to injuries from excessive pressure. This category includes mareotite (a consequence of pressure changes when diving to depth or ascent) and aerootite (a consequence of pressure changes during air travel).
- Allergic eustachitis. A consequence of allergic reactions that cause inflammation of the mucous membrane.
Localization of the disease:
- Unilateral eustachitis is a lesion on one side.
- Bilateral eustachitis - if the lesion occurs on both sides, bilateral turbootitis is diagnosed.
Patent foramen ovale
It can be classified as a minor anomaly in the development of the heart, since in this condition there is practically no shunting of blood. In the clinical assessment of a patent foramen ovale, the age factor is important. In newborns, a patent foramen ovale can accompany respiratory distress syndrome, while in adolescents this anomaly occurs latently, subclinically. In primary pulmonary hypertension, the presence of a patent foramen ovale is a prognostically favorable sign, and the life expectancy of such patients is longer than in the absence of this microanomaly. In this case, the resulting shunt relieves the right side of the heart and facilitates the natural course of the disease.
EchoCG criteria
Two-dimensional echocardiography
- Interruption of the echo signal from the interatrial septum in the area of the oval window.
- Unlike a septal defect in the area of the oval window, when the oval window is open, the walls of the septum gradually (wedge-shaped) become thinner, and with a defect, a break in the structure is visible.
- There are no hemodynamic disturbances characteristic of an atrial septal defect (volume overload of the right parts, paradoxical movement of the interventricular septum).
Doppler EchoCG
- Turbulent blood flow in the oval window area.
- Normal blood flow in the right ventricle and pulmonary artery (in the case of an isolated patent foramen ovale).
Causes of eustachitis and preventive measures
The disease occurs due to hypothermia, against the background of weakened immunity, due to infectious inflammation in the nasopharynx. It may manifest itself as complications after influenza, sore throat, pharyngitis, acute or chronic sinusitis, etc.
Symptoms of ear tube dysfunction
Damage to the tube lining may also be directly related to viral infection, which is thought to result in decreased mucociliary clearance. It has been noted that nasopharyngeal pH is lower in some patients with otalgia and adenoiditis. This may cause temporary hearing loss and hearing discomfort.
From the editor: Symptoms, treatment and emergency care for cardiac asthma
Typical presenting complaints include hearing fullness, hearing loss, tinnitus, distress, intermittent sharp pain, fluid sensation in the ear, persistent pain, and difficulty with ear appearance. 6 Symptoms, which can last from several hours to several months, are usually intermittent and may be temporarily relieved by swallowing, yawning, or chewing. In many children, eustachian tube ventilation is less effective due to anatomical differences, making these patients susceptible to middle ear conditions such as otitis media and otitis media with effusion.
Preventing diseases is always easier than curing them. Simple preventive measures will help avoid inflammation of the auditory tube:
- Timely treatment of all viral and infectious diseases
- Hardening and proper nutrition to strengthen the immune system
- Dress for the weather and prevent colds
- Correction of pathologies of the nasopharynx structure (polyps, cysts, etc.)
- Correction of allergic reactions
While watching the video you will learn about the Eustachian tube.
In addition, multiple upper respiratory tract infections and enlarged adenoids and tonsils may also contribute to the increased incidence of middle ear disease in children. Habitual sniffing creates negative pressure in the middle ear. Air travel or scuba diving can cause ear pain secondary to negative middle ear pressure.
For most patients, normal swallowing and chewing gum can equalize the pressure, helping air move through the eustachian tube. Rhinoscopy may reveal a deviated septum with or without turbulatory hypertrophy. Peratubal inflammation or mass may appear on nasopharyngoscopy. In acute otitis media, the eardrum may be erythematous and bulging, whereas in chronic otitis media, the membrane may appear dull. In both cases, the membrane will show a sluggish response to pneumatic otoscopy.
Health is a precious gift. It remains to wish everyone to own this treasure for as long as possible and protect it in every possible way.
Inflammation of the eustachian tube is also called eustachitis or tubootitis. It is regarded as the initial stage of catarrhal otitis and implies an inflammatory process localized in the Eustachian tube, leading to otitis media. As a rule, it occurs as a result of the transition of inflammation during rhinitis, sinusitis, pharyngitis, and tonsillitis.
Inflation of the eustachian tube through the Valsalva maneuver can further disrupt negative pressure. Decongestants, steroids, antihistamines, or leukotriene antagonists may be used to relieve congestion and allow the eustachian tube to open.
To improve compliance, tell the patient that these medications may take time to be fully used
Further attention should be paid to early tachyphylaxis observed with the use of nasal decongestants5. No supplier should be responsible for the development of concomitant drug rhinitis
He or she may perform tympanometry to further evaluate eustachian tube function. Other tests include an audiogram and telescopic examination of the nose.
Echocardiography (causes of cardialgia and heart murmurs) – Rybakova M.K.
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Experience in the treatment and diagnostic center “Art-Med” allows us to divide patients who come for echocardiography into certain groups, depending on the reasons for their visit.
The first category will be pregnant women
, since an echocardiographic examination is considered mandatory and is included in the examination plan.
The second, numerous category will consist of young people
with cardialgia.
The third group will consist of patients with chronic heart pathology
, requiring dynamic observation (congenital and acquired defects, etc.) or clarification of the diagnosis.
The fourth group will consist of patients with new complaints of pain in the heart area
, shortness of breath, manifestations of heart failure. This group of patients is the most serious, because
among them one can find “acute” pathology (aneurysm of the thoracic ascending aorta, thromboembolism in the pulmonary artery system, development of aneurysm of the left ventricle, etc.). The fifth group will consist of patients with a heart murmur
.
We will try to explain the capabilities of echocardiography in diagnosing heart pathology and differential diagnosis. To do this, we will try to analyze the above groups of patients.
Echocardiography during pregnancy
During pregnancy, a healthy woman can experience minor changes in the size of the heart cavities and changes in hemodynamics compared to the baseline. Systolic pressure in the pulmonary artery can increase to 40 mmHg. Art.
The diameter of the aortic root, left atrium and left ventricle may increase by 2–3 mm. The heart rate increases by 25–30%, and already in the first trimester of pregnancy the minute volume of blood flow and stroke volume increase. Blood pressure does not change.
The degree of valve regurgitation increases (on the tricuspid valve and pulmonary artery valve to degree 3, on the mitral valve to degree 2). In rare cases, a reaction of the pericardial layers can be observed - the presence of a small amount of fluid in the pericardium.
The fluid disappears 1 to 3 months after birth in the absence of treatment.
One of the features in pregnant women is dynamic stenosis of the inferior vena cava.
This phenomenon may be accompanied by an auscultatory picture - noise during auscultation and syncope that occurs when the body position in space changes.
In some cases, during pregnancy, the oval window opens and a slight shunt of blood from left to right is noted. All of the above changes usually disappear after childbirth. Dynamics are best carried out 1 – 3 months after birth.
Causes of cardialgia - pain simulating pain in the heart
The most common cause of cardialgia in young people is overwork, stress and hypokalemia (potassium deficiency).
Sometimes in this category of patients one can observe a slight prolapse of the anterior leaflet of the mitral valve into the cavity of the left atrium, which is a variant of the hole for young people and children (Fig. 1).
This prolapse should not be confused with pathological one when there are organic changes in the valves (for example, with myxomatous degeneration - Fig. 2).
Rice. 1.
Minor prolapse of the anterior leaflet of the mitral valve (normal variant).
Rice. 2.
Myxomatous degeneration of the mitral valve leaflets.
A differential diagnosis can be made at an appointment with a cardiologist or therapist. As a rule, after a conversation with the patient and auscultation, the doctor prescribes an ECG and EchoCG examination. If an electrolyte imbalance is suspected, a biochemical blood test is recommended.
In patients with chronic heart disease
, for example, rheumatic heart disease, congenital heart disease, prosthetic heart valve, etc. Echocardiography is performed once a year or once every 2 years.
Echocardiography allows you to assess the condition and structure of the heart valves, the degree of defect, the condition of the prosthesis, the systolic function of the ventricles of the heart, the condition of the aortic walls, the degree of pulmonary hypertension, the condition of the pleural cavities and pericardium, etc. (Fig. 3 and 4).
In some cases, patients come to clarify the degree or nature of the defect.
Rice. 3.
Rheumatic heart disease – mitral valve stenosis.
Rice. 4.
Congenital heart disease – atrial septal defect. Dilation of the right chambers of the heart, shunting blood through the defect in color Doppler mode.
Patients with new complaints of pain in the heart area and clinical manifestations of heart failure
are the most serious group of those examined and often require a more detailed examination (for example, coronary angiography) or consultation with a cardiac or vascular surgeon (Fig. 5).
Rice. 5.
Aneurysm of the ascending aorta.
The causes of heart failure are varied. The echocardiography technique allows for closer verification of the diagnosis, and in some cases, an accurate diagnosis.
Heart murmurs
One of the most common reasons for referral to echocardiography is the presence of a heart murmur.
In the “pre-echocardiographic” era, it was in some cases difficult to distinguish normal functional murmur from pathological one.
Let's try to list the causes of the most common normal functional murmurs in the heart area. They are especially good for children, teenagers and thin people.
Additional chord in the cavities of the ventricles (false chord or false chord)
- a filamentous structure located in the cavity of the left or right ventricle.
Located between the interventricular septum (IVS) and the wall of the heart, the head of the papillary muscle and the wall, etc. The base of the accessory chord does not thicken during systole.
The number of chords may vary. Occurs in 98% of cases (Fig. 6).
Rice. 6.
Minor developmental anomaly - an additional chord in the cavity of the left ventricle (normal variant).
Additional muscle trabecula in the ventricular cavity (false trabecula)
- a muscular structure located in the cavity of the left or right ventricle. Often located parallel to the interventricular septum or transversely between the walls of the ventricle. The base of the accessory muscle trabecula thickens during systole. Occurs in 85% of cases (Fig. 7).
Rice. 7.
Minor developmental anomaly - additional muscle trabecula in the cavity of the left ventricle and two additional chords (normal variant).
Eustachian valve of the inferior vena cava
- vestigial valve. Does not play any role in cardiac hemodynamics. Occurs in 20% of cases.
Hiari network
- rudiment, continuation of the Eustachian valve of the inferior vena cava into the coronary sinus. Occurs in 2% of cases.
Aneurysm of the interatrial septum
Atrial septal aneurysm (ASA)
– a congenital feature of the development of the interatrial septum. The membrane of the fossa oval is elongated and bulges to the side (Fig. 8). There are a number of types of atrial septal aneurysm:
- type L – bulging of the membrane of the fossa oval towards the left atrium.
- type R – bulging towards the right atrium (Fig. 9).
- Type R – L – bulging to the right and then to the left.
- Type L - R - bulging to the left and then to the right - occurs in 5% of cases.
Rice. 8.
Aneurysm of the interatrial septum.
Rice. 9.
Aneurysm of the interatrial septum - type R.
If the aneurysm is very large and protrudes significantly into the atrium cavity, it can be regarded as a congenital defect of the interatrial septum (extremely rare). If there is an atrial septal defect in the area of the atrial septal aneurysm, the situation is regarded as a congenital heart defect.
Aneurysm of the membranous part of the interventricular septum
– occurs rarely (0.5 – 1% of cases).
Accessory heads of papillary muscles
– their number can be different and, according to anatomists, can reach 16, the sizes of the heads are also different. The more papillary muscles in the ventricular cavity, the more chordae extend from them.
Non-closure of the oval window
– a variant of the development of the membrane of the fossa oval, occurs in 25% of people. The valve of the fossa ovale membrane covers the oval window. There is no shunting of blood, but it can occur in a number of situations (for example, with a sharp increase in pressure in the cavity of the left or right atrium).
Patent foramen ovale
– occurs less frequently (1 – 2% of people).
Currently, in pediatric practice
there is an overdiagnosis of an open oval window.
In this case, blood shunting occurs from left to right, is intermittent, and the volume of the shunt is small. There is no pulmonary hypertension or dilatation of the right chambers.
Color Doppler allows you to clarify the presence or absence of an open oval window. These patients require observation once every 2-3 years.
Contraindications for diving
The only contraindication for people with a patent oval window is diving (scuba diving). In any case, whether you are going to Egypt or Thailand and want to plunge into the enchanting world of the seabed, or spend time in the city, do not be lazy to go to a cardiologist and undergo an echocardiographic examination. This will avoid tragic consequences.
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Source: https://www.medison.ru/si/art240.htm
What is it and where is it located?
At present, the question of which minor anomalies in the development of the cardiovascular system are considered pathology and which are considered age-related anatomical and physiological characteristics of the child’s body has not been fully resolved. The only exception is the presence of anatomical abnormalities of the heart in adults.
Blood flow in the womb has significant differences. During the first four weeks of development, the main formation of heart structures occurs. The muscular cardiac tissue (myocardium) and connective tissue - the framework of the main coronary vessels, arteries and veins - are formed. Until the moment of birth, the lungs do not participate in the process of saturating the small organism with oxygen and removing carbon dioxide. This role is performed by the placental circulation through the delivery of oxygenated blood through the umbilical vessels.
The Eustachian valve (EK) is a valve in the lumen of the inferior vena cava, which is necessary for blood circulation in the fetus (directing blood from the right atrium to the left through the open foramen ovale). The location of the EC is shown in the photo below:
Due to these communications, the delivery and outflow of blood is carried out in the volume necessary for a small organism. After childbirth and removal of the placenta, the vascular pathways change. With the baby's first cry at birth, the lungs expand and, under increased intracardiac pressure, the fetal openings in the heart begin to close. If the fold of endocardial tissue (inner membrane) is preserved in an adult, they speak of an elongated eustachian valve.
Elongated Eustachian valve
The Eustachian valve in the heart is determined at the level of the arch of the inferior vena cava, along its anterior surface. On average, after birth and the child reaches the age of 5-7 years, its size does not exceed 10 millimeters, or the connective tissue structure is completely absent. Anatomically it is:
- a fold of the endocardium in the shape of a semilunar valve;
- length from 0.2 to 1.0 centimeters;
- an elongated filamentous formation stretching from the axis of the inferior vena cava to the middle of the atrial wall and septum;
- a movable valve that floats freely in the bloodstream;
- on ultrasound it is determined in the area of the lower axis of the vein;
- when large in size, it can reach the region of the tricuspid valve and partially protrude into the cavity of the right ventricle.
Symptoms of insufficiency of the bauhinium valve
With dysfunction of the ileocecal valve, doctors are approached with a variety of complaints. Symptoms are typical for 95% of digestive diseases:
• Pain syndrome – unpleasant sensations are localized in different parts of the abdominal cavity. • Dyspeptic disorders (nausea, vomiting). • Absence of bowel movements for 3 days (in 25% of patients). • Loud intestinal motility, ending with the urge to defecate. • Flatulence, tension in the anterior abdominal wall. • Problems with defecation – 75% of patients with this pathology experience diarrhea. • Bitter taste in the mouth, heartburn, gray or white coating on the tongue.
Additionally, patients are concerned about increased fatigue, weight loss while maintaining the same appetite, and insomnia.
Prevention
Trying to prevent inflammation of the auditory tube, you need to pay a lot of attention to your body:
However, the temperature is only one to two thirds of the time. It usually happens that the eustachian tube from the nasopharynx to the middle ear receives viruses, and once the mucous membrane is weakened, the second phase leads to inflammation caused by bacteria.
Pressure on the drum causes significant pain, and in extreme cases can cause the drum to rupture, which can be dangerous for doctors
This is especially important because the shard doesn't have to make a perfect shard. If you have inflammation of the middle ear, be sure to consult a doctor
There is also a risk of hearing loss or even hearing loss that is minor. “We also have to think that because a child has a hearing loss, their language development may be slower,” she adds.
If you have the slightest suspicion that there is something wrong with your ear, do not diagnose it yourself. Perhaps you do not have inflammation, but a gaping auditory tube - a completely different serious pathology.
Do not delay, but immediately go to. It’s naive to believe that it “will go away on its own.” Such processes need to be treated for a long time, paying attention to the problem. The pathology can be of a different nature, but the result if neglected is the same - hearing loss or complete deafness.
In the medical literature, the Eustachian tube is described as a canal that connects the nasopharyngeal cavity to the tympanic region. It received its name in honor of the Italian who first described it in 1564. Its length is about 35 mm, and its diameter does not exceed 2 mm. Despite its small size, the functions and significance of the auditory tube are truly great.
During each visit to an ENT doctor, you can hear about the need for surgical treatment of any pathological changes in the ears. If this is not done, then the viral agent, using the oblong organ, will spread its negative impact further.