Normally, labor begins 38 weeks after conception, but a full-term baby can be born at 36 or 42 weeks. The date of planned birth is counted in different ways: from the date of possible conception or from the first day of the last menstruation, so the gestation period may vary.
The first signs of labor may appear 2-3 weeks before the onset of labor. But it is better to go to the maternity hospital directly during regular true contractions with an interval of 5-7 minutes in order to avoid medical stimulation and give birth naturally.
What does a woman most often experience before giving birth?
- irritability, fear and anxiety, which is caused by hormonal changes in a woman’s body;
- nausea, loss of appetite or, conversely, increased appetite, vomiting, upset stomach, as well as weight loss of 1-2 kg, which can occur several weeks or days before birth and is associated with the functioning of the hormonal system;
- a slight increase in body temperature and chills very often accompany the onset of labor;
- pain in the lower abdomen, lower back or sacrum, which are pulling or spasmodic in nature and are provoked by displacement of the vertebrae in the sacrum and increased excitability of the nervous system;
- excitability of the uterus, which is manifested by increased sensitivity and tension of this organ, this happens periodically, first 1-2 times a week, then several times a day;
- false contractions are training contractions of the uterus that begin to bother a woman several weeks before giving birth and differ from true contractions in that they do not have a strict frequency and can be eliminated with the help of relaxing procedures, walking, and a warm bath;
- true contractions are regular, cramping pain that occurs before childbirth and is accompanied by dilatation of the cervix.
Signs of the onset of labor are also brown discharge from the genital tract and prolapse of the abdomen before childbirth.
Harbingers of childbirth
The harbingers of childbirth are those “news” that the body sends us so that the expectant mother understands that the long-awaited meeting is approaching.
It is impossible to know the day “X” in advance, since these signs can appear both a few hours and several weeks before the start of regular labor.
But, the closer the date of birth, the more carefully the expectant mother should listen to the sensations in her body.
In the last weeks of pregnancy, the hormonal levels of the expectant mother change. As the placenta ages, the production of the pregnancy hormone progesterone decreases and the level of estrogen increases, under the influence of which the pregnant woman’s body prepares for the upcoming birth.
In the cerebral cortex, the center of labor is formed - the dominant of labor.
The appearance of precursors of labor is a normal reaction of the body to changes in hormonal levels, which does not require any correction. For some women, the body’s preparation occurs unnoticed, and this is also absolutely normal.
Precursors of childbirth include such signs as:
- prolapse of the abdomen;
- weight loss;
- discharge of the mucus plug;
- discomfort in the lower abdomen and back;
- change in appetite;
- emotional instability;
- training contractions.
Let's look at each sign in more detail.
1. Abdominal prolapse
In 10-14 days, the fetus takes the most convenient position for childbirth - the presenting part of the fetus is pressed against the entrance to the pelvis, so the fundus of the uterus moves down. The pressure on the diaphragm and stomach is reduced, it becomes easier for the expectant mother to breathe, heartburn and the feeling of heaviness after eating disappear. However, moving lower, the uterus puts pressure on the bladder and rectum, so urination and stool become noticeably more frequent.
2. Losing body weight.
During pregnancy, the main hormone is progesterone, one of its actions is to retain fluid in the tissues. On the eve of childbirth, when its level decreases and the level of estrogen in the blood increases, excess fluid is removed from the body of a pregnant woman. This explains the weight loss.
3. Removal of the mucus plug.
A mucus plug is a thick mucus that fills the cervical canal during pregnancy and serves as a barrier to any infection entering the baby. The release of the mucus plug usually occurs 1-2 days before the onset of labor, although it may take two to three weeks.
On the eve of childbirth, the cervix begins to change: it softens, shortens, centers (is located in the center) and opens slightly. As a result, the mucus plug comes out.
Some women may notice a plug in their underwear (a lump of dense mucus, colored brown or with a small admixture of blood), and some pregnant women do not notice this process at all, since their mucus plug can only come out during the birth of the child.
The release of the mucus plug is the most significant sign in terms of information content.
4. Discomfort in the lower abdomen and back.
Discomfort in the lower back (sacrum) and lower abdomen can be caused by sprained ligaments and increased blood flow to the pelvic organs. These sensations can be aching or pulling.
5. Change in appetite.
Decreased appetite may appear 5-7 days before birth. This is due to changes in the autonomic nervous system and hormonal levels.
6. Emotional instability.
Hormonal changes before childbirth in a woman’s body lead to emotional instability, which is manifested by frequent mood swings, fatigue, lethargy, and can suddenly change to vigorous activity.
7. Training contractions.
Most women feel training contractions on the eve of childbirth - these are also harbingers of labor. Regular pulling sensations appear in the lower abdomen, but such contractions, unlike labor contractions, are short-term, not painful and do not lead to structural changes in the cervix. If training contractions occur, then you just need to wait: lie down, rest, you can take a warm bath, try to take a nap. The training contractions will gradually end, and the real ones will intensify.
Medical help is needed if you experience:
- severe abdominal pain;
- bright scarlet discharge from the genital tract;
- increased blood pressure to 140/90 mmHg and higher;
- severe headache, nausea, vomiting, blurred vision, convulsions;
- absence of fetal movements for 6 hours or more;
- rupture of amniotic fluid;
- regular labor activity.
Be alert to the signs described above.
about the author
- Sytova Valentina Ivanovna
- Obstetrician-gynecologist of the first category
- All publications by the author
How does the plug come out before childbirth?
A few days before the onset of labor, a woman begins to experience discharge from the genital tract, reminiscent of the onset of menstrual bleeding. This is the release of mucus, which protected the uterus and the fetus in it from infection from the vagina.
The discharge of the mucus plug before childbirth can occur quickly, as if the plug had actually popped out (this is typical if the fetus is heavy), or it can flow out slowly over several days. This process signals the dilation of the cervix and the onset of labor.
How a woman's body changes before childbirth
From week 36, estrogen begins to be synthesized in large quantities, and progesterone, on the contrary, decreases. These are symptoms of aging of the placenta, which are accompanied by the fact that contractile proteins begin to be produced in the uterus, and oxytocin, a stimulant of labor, begins to be produced in the pituitary gland.
And at 38 weeks, increased electrical activity is observed in those parts of a pregnant woman’s brain that are responsible for labor. This is called "generic dominance".
As for the baby, due to increased growth at the end of pregnancy, the uterus encloses it too tightly: this is due to a decrease in amniotic fluid. For the fetus, this is stress, and its adrenal glands produce large quantities of the stress hormone - cortisol. Since baby and mother are bonded, the release of cortisol stimulates the production of prostaglandins in the mother's body. When this hormone and oxytocin accumulate in the required quantities, labor will begin.
In addition, the cervix ripens: its structure changes, it becomes soft, pliable, shortened and smoothed.
When does your stomach drop?
3-4 weeks before the planned date of birth, the pregnant woman’s belly seems to slide down, this happens gradually and slowly. At the same time, the stomach changes somewhat in shape and decreases in size.
As the abdomen lowers, it becomes easier for a woman to breathe and eat as the diaphragm is released.
When symptoms of impending labor appear, a woman should rest more and save her strength for the main period of pregnancy - the birth of the baby.
Symptoms of near birth
But all this happens in a woman’s body without her conscious participation. These processes are expressed externally in a number of symptoms that a woman can track on her own. Shortly before birth, the “stomach drops” - the bottom of the uterus drops, as the baby takes a more comfortable position before birth closer to the vagina. In first-time mothers, the abdomen may drop 2 weeks before birth, and in second-time mothers - 2 hours before birth. In addition, the shape of the abdomen changes, and the woman even begins to feel some relief: the stomach does not put pressure on the diaphragm, there is no longer shortness of breath or belching after eating.
But at the same time, the drooping stomach puts pressure on the bladder and rectum, so the woman visits the toilet more often. In addition, due to the active production of estrogen and the body’s desire to get rid of excess fluid before childbirth, the stool is often liquid, and diarrhea may even occur.
Specialists
Makatsaria Alexander Davidovich
Obstetrician-gynecologist, famous scientist, founder of clinical hemostasiology.
It will help you plan and maintain your pregnancy if you have had cases of fetal loss, thrombosis, obstetric complications or blood coagulation disorders. You can also contact your doctor for a transcript of hemostasis tests.
Egorova Elena Borisovna
Obstetrician-gynecologist of the highest qualification category.
Specializes in peritoneal factor of infertility in women and management of problematic pregnancies.
It will provide effective help if, before conception, you were diagnosed with adhesions, endometriosis, erosion or other pathologies of the cervix.
Akinshina Svetlana Vladimirovna
Obstetrician-gynecologist, hemostasiologist with an academic degree.
Pregnancy management S.V. Akinshina will help avoid severe complications: gestosis, placental insufficiency, fetal loss syndrome.
The doctor's expertise includes hemostasis disorders and immunological infertility.
Bitsadze Victoria Omarovna
Gynecologist-hemostasiologist, professor, doctor of medical sciences.
The doctor's profile is management of high-risk pregnancies, including in women with genetic thrombophilia and a tendency to spontaneous bleeding. Develops effective treatment regimens for infertility associated with autoimmune pathologies and hemostasis disorders.
How labor begins: signs and sensations.
Childbirth in primiparous and multiparous women begins with contractions - involuntary, rhythmic contractions of the uterine muscles with a frequency of at least 1 every 10 minutes, remotely comparable to very severe menstrual pain. The rupture of amniotic fluid does not mark the beginning of labor. It happens that labor occurs independently or does not occur at all when the waters break.
Only contractions provide gradual opening of the uterine pharynx and are assessed according to the following indicators: frequency, duration, strength and pain. At the very beginning of the “path”, contractions are rare and short: 10-20 seconds every 10 minutes. Further, the pauses between contractions are shortened, and the duration increases and reaches 50-60 seconds at the end of the first stage of labor.
It is very important at this time to be under the supervision of a doctor, since only a doctor will be able to determine the pathological process - weakness of labor forces, discoordinated labor, begin drug induction of labor when amniotic fluid has leaked, offer adequate and modern anesthesia at the very start and make adjustments for the further smooth course of labor .
In addition to the dynamics and pain of contractions, the doctor also evaluates the fetal heartbeat, cervical dilatation and the general condition of the woman - he always measures temperature, pulse and blood pressure.
Childbirth is one of the critical periods in the life of not only a child, but also a woman, therefore a progressive, but at the same time careful approach in the “do no harm” concept, which can only be implemented in medical institutions, is the key to the health of the expectant mother and baby.
The beginning of labor. Preliminary stage
They are needed to ensure that the cervix is fully prepared for childbirth.
For the first birth, such preliminary contractions are more typical; they can last for five days or even more. A woman often mistakes them for the beginning of real contractions, but there are several signs by which preliminary contractions can be distinguished from labor contractions.
Preliminary contractions are not regular, do not become more frequent or intensify, they are usually less intense than labor contractions, although a woman giving birth for the first time has nothing to compare with, and the pain may seem quite noticeable. In order to cope with pain, sometimes it is enough to walk around or change your body position.
At this time, it is best to rest, get enough sleep if possible, in order to gain strength before giving birth.
But when contractions become regular, this indicates the beginning of the labor process. The beginning of contractions is indicated by something like this: 40 seconds contraction - 20 minutes pause - 40 seconds contraction - 15 minutes pause - 40 seconds contraction - 15 minutes pause - 40 seconds contraction - 15 minutes pause.
Primiparous women often fear that they will not be able to detect the onset of contractions. In fact, contractions are such a unique process that it is simply impossible to confuse it with something else. During contractions, it seems that the pain rolls in like a wave, originates in the middle of the back, then spreads to the hips and seems to unite in the abdominal area.
During a real contraction, the uterus becomes toned, and the pregnant woman can feel its tension by placing her hand on her stomach. Contractions gradually intensify and become more frequent.
At this time, you need to call the doctor and get ready for the maternity hospital. If a woman is going to give birth at home, then it’s time to call the midwife and get ready for the active process to begin.
It is very important at the beginning of labor not to be scared or tense. It is important to breathe correctly - that is, deeply and slowly, you can try to sing - the correct sound is taught in many schools and in childbirth preparation courses.
Proper breathing is important so that the baby receives a sufficient amount of oxygen, and the mother’s body is relaxed and does not interfere with the birth process.
When the pain approaches, you need to breathe deeply, taking full inhalations and exhalations. After the contraction begins, you need to completely relax and breathe shallowly, taking quick and rhythmic inhalations and exhalations. The contraction has passed - you can take a full breath into your stomach and chest and exhale slowly.
In between contractions, rest and breathe normally. In addition to proper breathing, pain can be relieved by massage of the sacral region and lower back, and sometimes simply by stroking the abdomen.
It’s good when a mother talks to her baby - this will calm not only her, but also him - since now the baby is experiencing no less difficult sensations than his mother.
In the intervals between contractions, you can do household chores: according to popular belief, at this time it is good to prepare food for the husband who remains at home, and iron children's things.
During preliminary contractions, you need to complete all preparations for the maternity hospital: shave and give an enema. However, it must be taken into account that an enema, as a rule, also stimulates labor and after this procedure, contractions become more frequent and intense.
In some countries, it is believed that it is good to have sex during the onset of contractions - this helps stimulate labor, and the hormones released into the blood can have an analgesic effect.
In general, lying down during contractions is not necessary - in fact, it can be even more painful. Contractions often go easier if a woman stands, leans against a wall, the back of a chair, or hugs her husband, or walks around the room.
The main thing is to listen to your body and do what you really want to do. And you definitely need to tune in to the fact that labor is just beginning and there is still an endlessly long road ahead.
Gradually, contractions become more frequent and become longer and more intense. When the interval between contractions is 3-5 minutes, and the duration of the contraction reaches 1 minute, it is time to go to the maternity hospital.
During the first birth, you can wait quite a long time for such dilation, because the cervix must smooth out, if there is a bend in the uterus, it must “unbend,” etc.
Labor can begin not only with the onset of contractions, but also with the breaking of amniotic fluid - then you need to go to the maternity hospital earlier, because after the water breaks you need to give birth within 24 hours to avoid the risk of infection.
The water may break during contractions - and this is also a signal that you need to hurry to the maternity hospital. To prevent infection from spreading to the fetus, the expectant mother needs to put on fresh underwear and a clean pad.
By the way, after your water breaks, you should definitely pay attention to its color and inform your doctor about it. Normal waters are odorless, transparent, yellowish in color, and may contain a very small amount of blood.
At the end of the preliminary stage of labor, you need to go to the maternity hospital by taxi or ambulance. You must take with you your passport, observation card at the antenatal clinic (exchange card), and health insurance policy. Things you need are slippers, personal hygiene items, a clean robe and nightgown.
However, now in many maternity hospitals the list can be expanded and include a player with cassettes or a disk, a book, paper for writing notes to relatives, and a pen. You need to talk to your doctor about what you can take with you during your acquaintance with the maternity hospital, which, of course, should happen before the birth. If the birth takes place at home, then the midwife should also arrive by this time.
At the medical center, you can undergo a full medical examination before conceiving a child, during pregnancy and until childbirth. Under the guidance of an obstetrician-gynecologist at our center, you will be able to monitor the development of your baby and prepare for his birth.
Publications in the media
Childbirth is a complex physiological process of expulsion of the contents of the uterine cavity (fetus, amniotic fluid, membranes and placenta) through the natural birth canal.
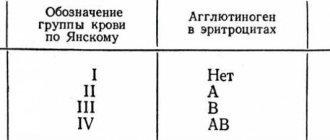
Reasons for the onset of labor • The placental clock is a hypothetical mechanism that determines the duration of pregnancy and the date of birth. When studying the content of placental corticoliberin in the blood of 485 pregnant women (McLean et al., 1995), it was found that already at 18 weeks of pregnancy, groups with normal, premature and late births can be distinguished. By the time predicted for these groups, the blood level of corticoliberin increases sharply. Perhaps this placental hormone is a signal of the onset of labor. • PGs promote the entry of Ca2+ into the myoplasm of SMCs, which leads to their contraction and the development of contractions. Reflex irritations (for example, manipulation of the cervix, rupture of membranes) lead to stimulation of Pg synthesis. • Oxytocin, synthesized both in the body of the pregnant woman and in the fetus, ensures the release of Pg and the release of a large number of other substances that stimulate myometrial contraction (serotonin, catecholamines, etc.). • Decreased progesterone levels. Labor is a process accompanied by contractions that occur with increasing frequency and intensity and lead to dilation of the cervix, the birth of the fetus and placenta. A distinction is made between the preparatory period (harbingers of childbirth) and true childbirth. • Precursors of labor include increased urination, the appearance of bloody-mucous discharge from the vagina, painless irregular contractions of the uterus (Braxton Hicks). The preparatory period for childbirth normally begins at 38 weeks. At this time, a number of changes occur in the pregnant woman’s body •• Formation of a generic dominant in the central nervous system - a stagnant focus of excitation that regulates preparation for childbirth and the process of childbirth itself. Clinically accompanied by drowsiness, calm behavior, a decrease in the pregnant woman’s body weight 7–10 days before birth by 800–1000 g •• Change in the ratio of estrogen and progesterone due to an increase in the level of estrogen, especially estriol, which provides the formation of receptors for Pg, oxytocin, serotonin, kinins and other biologically active substances that increase the excitability of the uterus •• The predominance of the influence of the adrenergic (sympatho-adrenal) nervous system •• Structural changes in the cervix. The mature cervix is located along the pelvic axis. The cervix is shortened to 1–1.5 cm, completely softened, the internal os is soft, smoothly passes into the lower segment of the uterus. The cervical canal freely allows a finger to pass through (opened by 2–3 cm), the length of the vaginal part of the cervix corresponds to the length of the cervical canal •• Tight pressing of the presenting part of the fetus to the entrance to the pelvis •• Detachment of the lower part of the amniotic sac from the walls of the uterus •• Appearance of mucous - bloody vaginal discharge (discharge of the mucous plug of the cervix).
• Characteristics of uterine contractions during childbirth . Labor contractions differ from preparatory contractions in the frequency (at least 1-2 times per 10 minutes) and strength of contractions, as well as in the sequential anatomical changes of the cervix (shortening, smoothing and opening). Periods of labor • The first period (dilation) begins with the first contraction. During the first stage of labor, contractions become quite frequent, intense, prolonged and cause smoothing and dilation of the cervix. The period of dilation ends with the transition of contractions to pushing and the discharge of amniotic fluid • The second period (expulsion). In the second stage of labor, the fetus is expelled. This period begins with the full dilatation of the cervix, the transition of contractions to attempts and ends with the birth of the child • The third period (successional). The beginning is the moment of the birth of the child, the end is the separation of the placenta and the birth of the placenta. Birth in occipital presentation . Occipital (parietal) presentation is observed in 95% of all births. It is necessary to distinguish between positions and types of fetal positions. Position determines the location of a randomly selected part of the fetus (in this case, the occiput of the fetus) in relation to the right and left sides of the birth canal. More strictly, the position is defined as the location of the fetal back in relation to the right and left sides of the uterus. The type of position is defined as the ratio of the fetal back to the anterior or posterior side of the uterus. • Positions for occipital presentation •• First (left) position. In occipital presentation and the first position, the fetal back is turned to the left, the small fontanel is located closer to the left side of the uterus, and the large fontanel is closer to the right •• Second (right) position. With occipital presentation and the second position, the location is reversed (i.e., the back of the fetus is facing to the right, the small fontanelle is located closer to the right side of the uterus). • Types of positions for occipital presentation •• Anterior view. The sagittal suture of the fetal head forms an angle of 45° with the transverse size of the pelvis, the back of the head is turned anteriorly and faces to the right or left •• Posterior view. Posterior breech births account for approximately 1% of all occipital breech births. The diagnosis of posterior view is made only in cases where the back of the fetal head remains facing the sacrum of the woman in labor in the plane of the pelvic outlet. The second (right) position is observed much more often than the first (left). The posterior view is often combined with a narrowing of the entrance to the pelvis. Seven main fetal movements during childbirth. The process of adjusting the position of the fetal head to pass through various planes of the pelvis is necessary for the birth of a child. These changes in the position of the presenting part constitute the biomechanism of labor and include 7 sequential movements. The domestic school of obstetricians in the anterior form of occipital presentation identifies four moments of the mechanism of labor, corresponding to 3, 4, 5 and 6 fetal movements during labor according to the American classification. • Insertion of the head - the position of the fetal head at the moment of crossing the plane of the entrance to the pelvis. The insertion is considered normal if the vertical axis of the head is perpendicular to the plane of the entrance to the pelvis, and the sagittal suture is approximately the same distance from the promontory and the pubic symphysis. Normal insertion is called axial or synclitic. For any deviation, the insertion is considered asynclitic. • Promotion. The first condition for the birth of a child is the movement of the fetus through the birth canal. If insertion of the fetal head has already occurred at the onset of labor (in primigravidas), progress can be observed before the start of the second stage of labor. In multiparous women, advancement usually begins simultaneously with insertion. • Flexion of the head. When the descending fetal head encounters resistance from the cervix, pelvic walls and pelvic floor, the head normally flexes. This is the first moment of the labor mechanism according to the domestic classification •• The chin approaches the chest •• As a result of flexion, the fetal head is presented at its smallest size, equal to the small oblique size (9.5 cm). • Internal rotation of the head is accompanied by descent of the presenting part and is completed when the head reaches the level of the ischial spines. The movement involves a gradual rotation of the occiput anteriorly towards the symphysis pubis. This is the second moment of the mechanism of childbirth according to the domestic classification. • Extension of the head. Extension of the fetal head occurs after the area of the suboccipital fossa (fixation point) approaches the pubic arch; the back of the head is in direct contact with the lower edge of the pubic symphysis (fulcrum). The head extends around this fulcrum. This is the third moment of the mechanism of labor according to the domestic classification •• During extension, the parietal region, forehead, face and chin appear successively from the genital fissure. •• The expelling forces of contractions and abdominal muscles, together with the resistance of the pelvic floor muscles, contribute to the unfolding of the crown in the direction of the genital fissure. • External rotation of the head and internal rotation of the body. The born head returns to its original position. The back of the head returns first to an oblique position, and then to a transverse position (left or right). This movement is accompanied by a rotation of the fetal body, the shoulders are installed in the anteroposterior size of the pelvic outlet. This is the fourth moment of the mechanism of childbirth according to the domestic classification. • Expulsion of the fetus. After external rotation of the head, the anterior shoulder (fixation point) appears under the symphysis (fulcrum) and is then born. The perineum is soon stretched by the back shoulder. After the birth of the shoulders, the baby is born quickly.
MANAGEMENT OF LABOR Rupture of the membranes can occur at any stage of pregnancy • Signs - sudden release or leakage of clear fluid from the vagina. In a full-term pregnancy, delivery usually occurs within 24 hours after rupture of the membranes • There is a real danger of intrauterine infection (chorioamnionitis) with an anhydrous interval exceeding 12 hours, regardless of the time of labor. First stage of labor. On average, the first period lasts about 12 hours for primiparous women and about 7 hours for multiparous women. • Constant monitoring of the fetal heart rate begins immediately after the onset of contractions, because a sudden slowdown (less than 120 per minute) or increase in heart rate (more than 140 per minute) may indicate threatening or incipient fetal hypoxia. • Amniotomy is an artificial violation of the integrity of the membranes. Amniotomy is performed strictly according to indications: polyhydramnios, flat amniotic sac, marginal placenta previa, premature placental abruption, etc. • Labor is divided into two phases •• The latent phase of labor is the period of time from the onset of regular contractions until the appearance of structural changes in the cervix (3-4 cm dilation). The duration of this phase in primiparous women is 6.5 hours, and in multiparous women it is about 5 hours. •• The active phase of labor begins after the latent phase. The cervix quickly opens from 3 to 8 cm at a rate of 1.5–2 cm/hour in primiparous women and 2–2.5 cm/hour in multiparous women. In the active phase, there is an initial acceleration, maximum rise and deceleration (cervical dilatation from 8 to 10 cm). • Discoordination of labor during any dilatation of the cervix is manifested by the absence of further dilatation of the cervix (the main indicator of normal labor is progressive dilatation) •• Weakness of labor. The myometrial contraction curve is normal, but intrauterine pressure rises during contractions to less than 15 mmHg. Correction of this type of dysfunction is usually carried out by stimulating labor. Below are several schemes for labor stimulation (other schemes for stimulating labor are widely used in obstetric practice) ••• Intravenous administration of oxytocin - 1 ml (5 units) diluted in 500 ml of 5% glucose solution or 0.9% sodium solution chloride Begin administration at a rate of 6–8 drops/min, gradually accelerating by 5 drops every 5–10 minutes (but not more than 40 drops/min) ••• Intravenous administration of Pg is carried out using the same method ••• Combined administration of oxytocin and Pg. 2.5 IU of oxytocin and 2.5 mg of Pg are diluted in 500 ml of 5% glucose solution and administered intravenously, gradually increasing the rate of administration from 6–8 to 40 drops per minute •• Excessively strong labor is manifested by extremely strong and very frequent contractions and increased uterine tone. It occurs more often in women with increased general excitability of the nervous system. In such cases, labor lasts 1–3 hours. Such labor is called rapid. Oxytocin is not recommended for use in cases of uterine hypertonicity. Sedative therapy relieves pain, relaxes the mother's muscles and usually leads to normal labor. Second stage of labor. The second period lasts on average about 50 minutes for primiparous women and about 20 minutes for multiparous women. However, the second period can often extend to 2 hours, especially in primigravidas. Attempts arise during this period. • Delivery through the vaginal canal •• Birth of the head. With each attempt, the genital slit is stretched by the fetal head. At first, the head appears in the genital slit only during pushing, disappearing when it stops. This is called head cutting. Then the head protrudes more and more and does not go back in the intervals between attempts, the vulva does not close, the head erupts, which is accompanied by stretching of the vulvar ring. The forehead, face and chin emerge successively through the perineum •• The birth of the shoulders. In most cases, the shoulders appear immediately after external rotation of the head and are born independently. The anterior shoulder is born, retained under the symphysis, and the posterior shoulder rolls out over the perineum, and then the entire shoulder girdle is born. If it is difficult to remove the shoulders, insert the index finger from the back into the armpit of the front shoulder and tighten the shoulder, then release the back shoulder. Excessive traction with stretching of the fetal neck can lead to injury to the brachial plexus or the roots of the fifth and sixth cervical nerves, known as Duchenne-Erb palsy. • Assisting childbirth with cephalic presentation •• Regulating the advancement of the erupting head ••• During pushing, three fingers of the right hand hold the fetal head, preventing its extension ••• With strong pushing, they help with the left hand: carefully bend the fetal head, preventing its rapid advancement •• • In between attempts, the left hand is left on the fetal head, and the so-called “tissue borrowing” is performed with the right hand - the tissue of the labia minora and clitoris is carefully lowered from the fetal head, the stretched tissue of the vulvar ring is brought towards the perineum •• Removal of the head ••• After the birth of the back of the fetal head, the woman in labor is recommended to restrain her efforts, breathing deeply and rhythmically through her mouth ••• At this time, the tissue of the vulvar ring is lowered from the parietal tubercles of the fetus, the head is slowly straightened with the left hand, and the perineal tissue is removed from the fetal face with the right hand ••• When the skin of the perineum turns pale or the appearance of cracks, perineotomy or episiotomy is indicated to prevent rupture of the perineum ••• If the umbilical cord is entwined around the fetal neck after the birth of the head, you must try to remove the umbilical cord loop. If this is not possible, the umbilical cord is crossed between two clamps •• Release of the shoulder girdle ••• After the birth of the head, it is turned to face the woman's thigh to the right or left (depending on the position). At the same time, the shoulders rotate and stand in the direct size of the pelvis (internal rotation of the shoulders) ••• First, the front (upper) shoulder is cut through. It is pressed against the symphysis, and then the perineal tissue is lowered from the posterior (lower) shoulder •• Birth of the torso. After releasing the shoulders, the palms of the hands on both sides are placed on the fetal chest and the body is directed upward, and the lower part of the body is born. • Primary treatment of a newborn •• Immediately after birth, the mucus from the mouth and nose is sucked out of the head. After birth, the baby is placed in a tray covered with a sterile diaper. The umbilical cord cannot be pulled. The baby should be positioned at the same level as the mother in labor •• The assessment of the newborn is aimed at determining the adequacy of oxygenation and breathing of the newborn. This is usually done using the abbreviated Apgar score. The Apgar score has been proposed to assess the level of oxygenation, ventilation and degree of asphyxia according to uniform criteria to facilitate the exchange of information between personnel involved in neonatal resuscitation. Apgar assessment is performed 1–5 minutes after birth. Five signs are scored from 0 to 2: heart rate, depth of breathing, muscle tone, state of reflexes and skin color. The total Apgar score at the 5th minute of life is an indicator of the effectiveness of resuscitation measures and the depth of perinatal asphyxia •• The child’s eyelids are wiped with a sterile cotton swab (separate for each eye) and gonoblennorrhea is prevented using the Matveev-Crede method: freshly prepared 30% r is instilled into the eyes -r sulfacetamide (for girls to prevent gonorrhea, also in the genital area). Prevention of gonoblennorrhea is repeated 2 hours after birth •• Primary treatment of the umbilical cord. At a distance of 10–15 cm from the umbilical ring, the umbilical cord is treated with 96° ethyl alcohol, after which two sterile Kocher clamps are placed on it at a distance of 2 cm from each other. The umbilical cord is then cut between the applied clamps, and the baby end of the umbilical cord is wrapped together with the clamp in a sterile gauze pad. After preliminary blood sampling to determine the AB0- and Rh-belonging of the child’s blood, a silk ligature or clamp is applied to the maternal end of the umbilical cord at the genital fissure. •• Secondary processing of the umbilical cord. The baby, wrapped in a sterile diaper, is transferred to a heated changing table ••• Umbilical cord ligation. The umbilical cord is treated with 96° ethyl alcohol and tied with a thick silk ligature at a distance of 1.5–2 cm from the umbilical ring. The ligature is tied on one side of the umbilical cord, and then on the opposite side. The umbilical cord is cut 2–3 cm above the ligation site with sterile scissors. The surface of the incision is wiped with a sterile gauze swab and, after making sure that the ligature is applied correctly (no bleeding), it is treated with 5–10% alcohol solution of iodine or 5% solution of potassium permanganate ••• Instead of a ligature, a Rogovin bracket can be applied to the umbilical cord. Before applying the staple, the umbilical cord is examined under a light source, wiped with a cloth soaked in 96° alcohol, and the Wharton jelly is squeezed out with two fingers. Then a bracket is applied. The umbilical cord is cut off 0.4 cm above the bracket, wiped with a dry gauze swab and, after making sure that the bracket is applied correctly (no bleeding), the umbilical cord remnant is treated with 5% potassium permanganate solution ••• In the future, care of the umbilical cord remnant is carried out in the open way •• • In case of Rh- and A0-incompatibility between the blood of the mother and the child, the umbilical cord is processed differently. After the birth of the child, the umbilical cord is immediately clamped (without waiting for the pulsation of the blood vessels to stop). Since sometimes there is a need for an exchange blood transfusion, it is advisable to leave a piece of the umbilical cord 8–10 cm long, tying it with a silk ligature ••• When giving birth to twins, the maternal end of the umbilical cord must be ligated, because with monozygotic twins, the unborn fetus will lose blood •• To remove the cheese-like lubricant from those places where it especially thickly covers the skin of the fetus (for example, in the inguinal folds and armpits), use sterile cotton wool soaked in sterile petroleum jelly •• Having completed the primary toilet of a newborn, determine its weight, body length, circumference of the head and shoulders. Then they put bracelets made of sterile oilcloth on their hands with the surname, first name and patronymic of the mother in labor, birth history number, gender of the child, body weight and length, and date of birth written on them. The baby is wrapped in warm sterile linen (diapers, vests, blankets) and left on a heated changing table for 2 hours, after which he is transferred to the neonatal ward. • Episiotomy - dissection of the vulvar ring during childbirth, the most common surgical intervention in obstetric practice. After a cut, the perineum heals faster than after a rupture. There are median (in domestic practice - perineotomy) and mid-lateral episiotomy, i.e. dissection of the perineum along the midline or lateral to it. Indications: threat of perineal rupture; the need for fetal-friendly delivery during breech presentation, large fetus, premature birth; acceleration of labor due to obstetric pathology, acute fetal hypoxia; operative vaginal delivery. Third stage of labor (successional). The placenta is usually separated and delivered within 10-15 minutes after the baby is born. • Signs of separation of the placenta •• The uterus becomes spherical and dense •• Bloody discharge appears from the genital tract, flowing down the umbilical cord •• Schroeder’s sign: the fundus of the uterus rises above the navel and deviates to the right, because. the separated placenta descends into the lower segment of the uterus and vagina, pushing the uterus upward •• Alfeld's sign: elongation of the umbilical cord stump, indicating that the placenta has descended. The detached placenta descends into the lower segment of the uterus or into the vagina, while the ligature placed on the umbilical cord at the genital fissure descends along with the umbilical cord by 10–12 cm •• Küstner–Chukalov sign: when pressing with the edge of the palm on the suprapubic region, the umbilical cord is not retracted into the vagina (if the placenta has not separated, the umbilical cord retracts) •• The appearance of a protrusion above the symphysis as a result of the placenta descending into the thin-walled lower segment of the uterus •• Mikulicz’s sign: when the separated placenta descends into the vagina, an urge to push appears (not always) •• Klein’s sign: after After pushing, the umbilical cord stump does not retract into the genital slit. • Before releasing the placenta, the bladder is catheterized and the woman is asked to push. Under the action of the abdominal press, the separated placenta is easily born. • If the placenta is not born, external methods of releasing the placenta are used •• Abuladze's method: after a gentle massage of the uterus with both hands, collect the anterior abdominal wall of the woman in labor into a longitudinal fold, then ask the woman to push •• Genter's method (rarely used): asking the woman in labor to relax, hands, clenched into fists, placed on the bottom of the uterus in the area of the tubal angles and slowly press inward and downward •• Mitlin's method: a hand clenched into a fist is placed on the anterior abdominal wall above the pubis with the back side to the symphysis. The fist is moved upward, pressing it tightly against the anterior abdominal wall of the woman in labor. Having reached the fundus of the uterus, they press towards the spine and ask the woman to push •• The Credet-Lazarevich method is a less gentle technique; it is used when other methods are unsuccessful ••• After emptying the bladder, a gentle massage of the uterus is carried out ••• They cover the fundus of the uterus, placing the thumb on its anterior surface, and the rest on the back ••• Squeezing the uterus and pressing its bottom down along the wire axis of the birth canal, squeeze out the placenta •• If there is no effect, manual separation of the placenta is used. • After the birth of the placenta, it is necessary to check whether the placenta and membranes are damaged, and whether there are missing fragments retained in the uterine cavity •• Inspection of the placenta. Having placed the placenta with the maternal surface facing up, it is carefully examined. If the placenta is not damaged, it has smooth, even edges. There should be no loose, broken vessels •• Inspection of the membranes. The membranes must be intact. If a torn vessel is found between the membranes, it means there was an additional placental lobe remaining in the uterine cavity •• Milk test. Using a Janet syringe, milk is injected into the vessels of the umbilical cord. If there is a rupture in the placenta, milk leaks out through it •• Air sample. The afterbirth is immersed in water, then air is pumped into the umbilical cord vessels using a Janet syringe. If the placenta is damaged, bubbles of escaping air are visible •• Retention of parts of the placenta in the uterus is a complication of childbirth, leading to severe bleeding and septic postpartum complications. If it is determined that placenta particles remain in the uterine cavity, they are removed by hand (less often with a blunt curette). • Prevention of atonic bleeding . Contraction of the myometrium leads to vasoconstriction and stops bleeding. •• Administration of oxytocin (10 units intramuscularly or 20 units per 1000 ml of 0.9% sodium chloride solution intravenously) in the early postpartum period promotes uterine contraction and reduces blood loss. Ergometrine, methylergometrine are also used •• Yakubova's method (prevention of bleeding in the placenta and early postpartum periods): after the birth of the fetus and clamping of the umbilical cord, 0.5 ml of oxytocin is slowly injected intravenously in 20 ml of 40% glucose solution, after the birth of the placenta - 1.5 ml of oxytocin IM •• The use of methylergometrine until the end of the third stage of labor is not recommended, because it also causes contractions of the lower segment of the uterus, which can complicate the release of the placenta from the uterus •• Indications for the prevention of atonic bleeding: complicated obstetric history, overdistension of the uterus (polyhydramnios, multiple pregnancy, large fetus); use of antispasmodics and analgesics during childbirth; age indications (young and primiparous women over 30 years old), labor anomalies, anemia and other cases when bleeding can be expected.
ICD-10 • O80 Singleton labor, spontaneous delivery