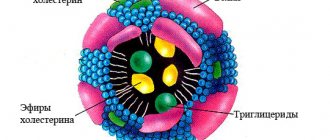
Triglycerides or triacylglycerides (TG) are ether compounds of the trihydric alcohol glycerol and fatty acids. Essentially, these are the same fats from food that fill the body with energy and are included in complex lipid metabolism.
Along with proteins and carbohydrates, TG are considered the main nutrient, but with a very unsteady limit of normal. An increase in triglycerides in the blood signals developing problems, and fat deposits are the most “innocent” part of them. It’s worse if the heart starts acting up and the blood vessels become clogged. This is where the level of triglycerides in the blood plasma must be reduced immediately.
Reasons for elevated levels
Hypertriglyceridemia (HTG) is the medical name for an increase in the content of TG lipid compounds in the blood. A high level of TIG does not immediately indicate a dangerous pathology.
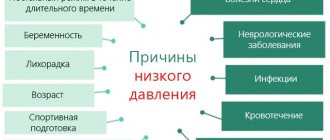
Initially, the reasons for violation of the norm are one or more lifestyle factors:
- overeating and/or predominance of fatty, fried foods, lack of coarse fiber in the diet;
- excess alcohol, smoking;
- sedentary lifestyle (when calorie intake exceeds calorie expenditure);
- stress, psychological overload;
- uncontrolled or long-term use of corticosteroids, first generation hormonal contraceptives, beta blockers.
If we talk about elevated TG and diseases, the connection here is secondary. That is, initially there was a failure of lipid metabolism, but certain diseases go “hand in hand” with high triglycerides and cholesterol:
- renal pathologies (chronic failure, nephrosyndrome, inflammatory processes);
- obesity;
- diabetes;
- atherosclerosis;
- hypothyroidism;
- prakreatitis;
- gouty disease;
- postoperative condition;
- coronary heart disease, stroke, heart attack;
- periodic increases in blood pressure from 140/90 mm. Hg pillar and above;
- hereditary disorders of fat metabolism.
Even completely healthy people over 50 years of age fall into the potential risk group.
In what cases is high triglyceride levels dangerous for the patient?
Lipid “jumps” occur frequently in healthy people (holidays, roast beef or fried chicken for lunch, and milk porridge with butter and cheese in the evening). If a person moves enough, is young and healthy, the body copes with the lipid load.
But control is necessary. Its task is to track the nature of the “fat” picture in the blood. There is no separate analysis for TG. The test is carried out using a lipid profile (lipid spectrum of a biochemical blood test), during which the content of several parameters in the blood is determined at once:
- total cholesterol value;
- triglyceride parameters;
- bad cholesterol - LDL;
- good cholesterol - HDL.
High TG is always accompanied by excess cholesterol, but how far the problem has gone depends on its type. Hypertriglyceridemia in combination with high LDL cholesterol poses a health hazard. If the “good” one has increased, then everything is not so bad. Although it won’t hurt to adjust your habits and diet.
Lipid standards - what are they:
What are triglycerides and what is their biological role?
Triglycerides are a type of fat found in the blood.
It is the body's largest energy reserve, allowing for mobility and availability of energy at any time, especially in conditions of starvation and food shortages.
When you exceed your intake of fats and carbohydrates, the excess calories are stored as triglycerides in the body's fat cells.
Features of hypertriglyceridemia in men
In men, elevated triglyceride levels quickly cause serious problems. And the older a man gets, the greater the likelihood of a dark development of the situation.
The fact is that increased TG in the plasma of the stronger half correlates with bad cholesterol, which causes an increase in cardiovascular pathologies, the formation of blood clots, cholesterol plaques with all the attendant risks.
And the reasons in most situations lie in the wrong lifestyle:
- smoking, alcohol addiction and everyday drunkenness;
- prolonged stress;
- excess flour and fatty foods in the diet against the background of a lack of protein foods;
- lack of physical activity;
- taking steroids and androgens to build muscle mass.
The last reason from the list is typical for bodybuilders and weightlifters. Like any hormones, lipids are involved in steroid metabolism. And the more an athlete uses anabolic steroids, the more dangerous the consequences.
Features of hypertriglyceridemia in women
Women are more likely to have elevated cholesterol and triglyceride levels. The fact is that adipose tissue plays a hormonal role for the fair sex and is responsible for many female functions. In addition, triglycerides are involved in the construction of estrogens. But even here there are limits beyond which lipids cause problems.
Pathological causes of increased TG in women:
- violations of estrogen-based oral contraceptive regimens;
- hormonal disorders;
- infertility;
- polycystic ovary syndrome;
- premenopause, menopause.
During pregnancy, women experience physiological hypertriglyceridemia. Moreover, cholesterol levels also increase significantly. The reasons lie in the most complex hormonal changes in the pregnant woman’s body.
Medium chain triglycerides[edit | edit code]
Medium Chain Triglycerides or MCTs
is a type of synthetic dietary fat first produced by the pharmaceutical industry from coconut oil in the 1950s to treat patients who were unable to digest regular fats. Still used for medicinal purposes, MCT oil has also become a popular fitness supplement, touted as a fat burner, muscle growth booster, and energy source.
Medium chain triglycerides are composed primarily of 8- and 10-carbon fatty acids (medium chain fatty acids, MCFAs). There are anecdotal reports that medium chain triglycerides
metabolized faster than long-chain triglycerides, with little or no deposition of medium-chain fatty acids in tissues, partially oxidized independently of carnitine and having perhaps the least impact on the functioning of the reticuloendothelial system.
The clinical effects of using a physical mixture of medium-chain and long-chain triglycerides do not differ from fat emulsions based on long-chain triglycerides. It is noted that when using high doses of the physical mixture, there is a risk of developing ketoacidosis and toxic effects on the central nervous system, due to the high amount of octaenoic (C8) acid. Structured triglycerides contain a balanced - equimolar ratio of medium-chain and long-chain triglycerides and a relatively smaller amount of octaenoic acid, therefore they are safer than physical mixtures. Physical mixtures of medium- and long-chain triglyceride emulsions have been available on the market since the 1980s, and structured triglycerides since the 1990s. Physical mixtures of medium- and long-chain triglyceride emulsions are not FDA approved and are not used in the United States.
Medium chain triglycerides in sports nutrition[edit | edit code]
Studies have shown that medium chain triglycerides can speed up the process of burning calories, which means reducing fat mass. However, half of all calories in the diet should come from these triglycerides, so in fact, medium chain triglycerides present in sports nutrition do not have a significant effect on metabolism
.[1].
JISSN Scientific Review[edit | edit code]
At the moment, the ability of MCT to improve athletic performance is not clearly supported by research: data vary significantly.[2][3][4][5][6] An experiment conducted in 2001 showed that taking MCT oil (60 g/day) for 2 weeks had no significant effect on athletic performance.[7] In addition, Goedecke found that MCT not only did not have a positive effect on athletic performance, but even had a negative effect in the case of trained cyclists.[8] This has been confirmed in other studies - without improving athletic performance, MCTs often cause gastric upsets.[9][10] However, an experiment conducted in 2009 noted a positive effect of MCT on individual perceived exertion (RPE) and lactic acid elimination.[11] It seems unlikely that medium chain triglycerides have a positive effect on athletic performance. However, further research in this direction is desirable.
How to control neutral fats
There are no specific signs of excess TIG, so regular lipid scanning is the basis for prevention. Starting from the age of 20, a healthy person only needs one lipid profile for 5 years.
Regardless of age, indirect signs should alert you:
- periodic heaviness and pulling sensations in the right side,
- frequent attacks of high blood pressure;
- shortness of breath, angina, heart compression and palpitations;
- noticeable increase in body weight.
Unscheduled checks are carried out in the presence of metabolic disorders, diabetes, and cardiovascular pathologies. Here on the recommendation of the attending physician. Upon reaching the age of 45 for men and 55 for women - at least one examination every 1-2 years.
How to prepare and take a blood triglyceride test
The analysis is submitted in a healthy state. After surgical interventions, acute infectious diseases or exacerbation of chronic diseases, examination should be postponed for 4-6 weeks.
What to consider:
- biomaterial for research – blood from a vein;
- before the examination, do not eat for 12 hours, do not drink for 3 hours;
- do not smoke for 30 minutes;
- Avoid physical and cognitive stress and stressful situations for 24 hours.
General interpretation of the results:
| Result(mmol/l) | Level rating | Risks |
| Less than 1.7 | Fine | low risk of developing cardiovascular disease |
| 1,7-2,4 | borderline content | in the absence of other factors - at an average level |
| 2,5 – 5,5 | high | There is a high probability that there are cholesterol plaques in the vessels, small/medium blood clots are possible, there are risks of heart problems or cerebrovascular accidents |
| from 5.6 | very tall | In addition to the problems described above, there is a risk of blood clots breaking off and developing acute pancreatitis |
When a high level of TG in the blood is reached, correction of the condition and clinical observation of the patient is required.
Velkov V.V.
The relationship between elevated triglyceride concentrations and cardiovascular risk is not simple. The reason is a complex system of connections between cardiovascular risks and disturbances in the levels of other lipids, especially those associated with cholesterol, and with other metabolic pathologies. Moreover, in some cases, hypertriglyceridemia (or hyperglyceridemia) does not have a noticeable effect on atherosclerotic vascular diseases, and this makes it difficult to accurately determine whether triglycerides are really a risk factor for them. However, it is considered well established that the risks of nonfatal myocardial infarction and the risks of sudden death from heart attacks increase with increasing triglyceride up to 800 mg/dL (9.01 mmol/L) but decrease sharply at higher triglyceride levels.
The association of elevated triglycerides with cerebrovascular disease is less certain. In general, elevated triglycerides often (but not always) lead to cardiovascular disease, and the quantification of this risk is highly dependent on the type of lipoproteins in which they are packaged. On the other hand, different causes of glyceridemia (genetic or caused by an unhealthy lifestyle) lead to different profiles of the ratio of different lipoproteins, and this, in turn, leads to different types of complications.
The combination of 1) high triglyceride levels, 2) low HDL-C , and 3) small dense LDL-C is commonly referred to as the lipid triad , resulting in diabetic dyslipidemia and atherogenic dyslipidemia. The lipid triad, in turn, is strongly associated with conditions of insulin resistance such as metabolic syndrome, polycystic ovary syndrome, and type 2 diabetes and, in general, is an important risk factor for early atherosclerosis. According to current US practice, elevated triglyceride levels are:
- marker of atherogenic lipoproteins,
- metabolic syndrome marker ,
and a very high level of triglycerides (more than 1000 mg/dL, 11.2 mmol/L) is a risk factor for pancreatitis .
1. The risk associated with elevated triglycerides depends on what lipoproteins they are packaged into. In the blood, triglycerides are packaged into five types of different lipoproteins: 1) chylomicrons - contain 85-90% triglycerides, 2) very low density lipoproteins X-VLDL - 50-60%, 3) intermediate density lipoproteins X-LDL - 20-25%; 4) low-density lipoproteins C-VLDL ≤10%: 5) high-density lipoproteins C-HDL ≤10%. Chylomicrons and VLDL-C are the richest in triglycerides. They are synthesized in the intestinal epithelium from fats that we get from food. Long chains of fatty acids are converted into triglycerides with the help of microsomal transfer protein and then combined with: cholesterol (exogenous, also obtained from food), with proteins (apolipoprotein B-48), and phospholipids, which ultimately forms chylomicrons. Then chylomicrons enter the bloodstream, where they interact with lipoprotein lipase, which is located in the capillary endothelial cells of muscle and adipose tissues. Lipoprotein lipase activates apolipoprotein Apo C-II, located on the surface of chylimicrons, and breaks down triglycerides packaged in chylomicrons, which then either enter the muscles, where they are utilized for energy needs, or are stored in adipose cells “in reserve.”
1.1. Initially “good” chylomicrons can become “bad”: a decrease in size leads to atherogenicity. Chylomicrons themselves are not atherogenic - they are too large to penetrate the vascular epithelium and lead to endothelial dysfunction. But when their triglyceride “filling” is consumed and goes either for cellular needs or for storage, chylomicrons, or rather their remnants (remnants) greatly decrease in size and are freed from lipoprotein lipase. Such already small and already rhamnant chylomicrons contain almost no triglycerides - but what remains in them becomes atherogenic - cholesterol, originally obtained from food (besides it, B-48 and apo E remain in the rhamnant particles). It is the small size of rhamnant chylomicrons that allows them to penetrate arterial walls and/or bind to specific sites on macrophages and stimulate their transformation into foam cells. Of course, such atherogenic chylomicron remnants must be removed from the bloodstream. Apolipoprotein E (Apo E), located on the surface of rhamnant particles, binds to LDL-C receptors in the liver and then is utilized in the liver. But before this moment she can have time to do her “dirty atherogenic deed”. So triglycerides themselves are not atherogenic, they make chylomicrons atherogenic when they leave them. Elevated triglycerides are a marker, but not a factor of atherogenesis. A normal fasting triglyceride level is less than or equal to 150 mg/dL (1.69 mmol/L).
1. 2. VLDL-C: increasing density “turns” them into “bad” LDL-C. VLDL-Cs are smaller in size than chylomicrons, but higher in density. VLDL-C are formed not where chylomicrons are and not in the same way as they are. VLDL-C are formed in the liver from endogenous triglycerides and cholesterol, which are synthesized there in the liver; VLDL-C are formed thanks to the microsomal transport protein. Then VLDL-C acquires apolipoprotein Apo B-100. When VLDL-C enters the bloodstream, apolipoproteins C and E are attached to their surface; the source of these apolipoproteins is other lipoproteins, in particular LDL-C. Like chylomicrons, VLDL-C are captured by lipoprotein lipases located on muscle and adipose tissues, which in this case also break down their triglyceride “filling”. Once the VLDL-C core is freed from triglycerides, lipoprotein lipase is no longer needed and dissociates from the VLDL-C remnants, which continue to contain cholesterol. These rhamnant VLDL-C are also called intermediate-density lipoproteins. Normally, they should also be catabolized by liver receptors, the activity of which is provided by Apo E. But this does not always occur to the proper extent, in the bloodstream due to hepatic lipase. rhamnate VLDL-C can “convert” into highly atherogenic LDL-C. In general, it is the release of triglycerides from chylomicrons and VLDL-C and the subsequent ineffective utilization of the remnants of chylomicrons and VLDL-C that leads to cardiovascular risk.
1.3. The appearance of plasma alone may indicate hyperglyceridemia. Indeed, by the appearance of plasma or serum, one can roughly estimate the concentration of triglycerides and establish the presence of chylomicrons: 1) plasma is transparent - the concentration of triglycerides is usually normal; 2) the plasma is turbid or slightly opalescent – the concentration of triglycerides is increased; 3) plasma is opaque and resembles milk - the concentration of triglycerides exceeds 500 mg/dL (5.63 mmol/L). To visually identify chylomicrons, the plasma is kept for several hours at 4°C. Chylomicrons form a superficial creamy layer or film. Important note: excess chylomicrons can also be found in the plasma of healthy people if the blood was not taken on an empty stomach (especially after eating a meal rich in triglycerides).
2. Triglycerides and the risks of cardiovascular disease. The limit beyond which elevated triglycerides begin is 150–199 mg/dL (1.69–2.24 mmol/L). Patients with borderline triglyceride values should be tested for metabolic syndrome, an easily overlooked condition that can lead to atherosclerosis. The diagnosis of hyperglyceridemia is made when triglyceride concentrations are higher than 200 mg/dL (2.25 mmol/L). Important note: if triglyceride levels exceed 400 mg/dL (4.5 mmol/L), the LDL-C concentration cannot be calculated; it must be determined directly. High triglycerides ≥ 500 mg/dL (≥ 5.63 mmol/L). In this case, the first goal of therapy is to reduce triglycerides themselves, since they are no longer only a marker, but also a risk factor. For patients at risk of atherosclerosis, the second goal of therapy in this case is to lower LDL-C levels. Ultra-high triglycerides - above 1000 mg/dL (11.2 mmol/L). This is a high risk of pancreatitis. In these cases, triglyceride concentrations should be reduced. Patients with triglyceride levels above 2000 mg/dL (22.4 mmol/L) require emergency care.
3. Hyperglyceridemia: hereditary and ill-acquired. The main sign by which hyperglyceridemia is classified is whether it is primary (genetically congenital), or secondary - caused by an unhealthy lifestyle and unhealthy diet. Primary - familial hyperglyceredemias - are more severe than acquired ones and require drug treatment; changes in diet and exercise cannot get rid of them.
3.1. Familial hypertriglyceridemia (hyperlipoproteinemia type IV). This is what is most often encountered in general practice. Triglyceride concentrations are usually between 250 and 1000 mg/dL (2.8 – 11.2 mmol/L), and VLDL-C levels are often elevated. Chylomicronemia can increase triglyceride levels even further. If Apo E is also elevated, this pathology can be diagnosed as familial combined hyperlipidemia. It is exacerbated by frequent alcohol consumption and sometimes leads to early cardiovascular disease. Familial hypertriglyceridemia is usually associated with insulin resistance.
3.2. Familial hypertriglyceridemia with chylomicronemia (hypertriglyceridemia type V). It is observed in adults and is considered a rare case of familial hyperglyceridemia. Triglyceride levels above 1000 mg/dL (11.2 mmol/L) are at high risk for pancreatitis. As with familial hypertriglyceridemia, such patients have elevated VLDL-C levels and markedly elevated chylomicron levels. This pathology is associated with insulin resistance, obesity and other secondary (non-hereditary) causes of hypertriglyceridemia. Such patients should reduce their weight, reduce the amount of fat and simple carbohydrates in their diet, and begin taking medications if triglyceride levels persist above 1000 mg/dL (11.2 mmol/L).
3.3. Familial chylomicronemia (a form of hyperlipoproteinemia type I). This is a very rare pathology. From birth, triglyceride levels are extremely high - 1000 - 10,000 mg/dL (11.2 - 112.0 mmol/L). Reason: Due to genetic defects, excess chylomicrons are not utilized by the liver. Mutations leading to this impair the function of lipoprotein lipase or, less commonly, its cofactor Apo C-II. Often in such patients, recurrent pancreatitis is observed already in childhood, but early atherosclerosis usually does not develop. Such patients should be evaluated by a lipid specialist. Extremely high triglyceride concentrations can usually be reduced by a strict diet that limits fat intake and, in some cases, by consuming fish oil.
3.4. Familial hyperlipoproteinemia with phenotype V. Its main manifestation is severe hypertriglyceridemia caused by an increase in chylomicrons and VLDL-C. Triglyceride levels are usually 1000–2000 mg/dL (11.2–22.4 mmol/L), but can vary widely under the influence of alcohol, diet, glucocorticoids, estrogens, as well as concomitant diseases (obesity, diabetes mellitus) . In families with this disease, the risk of atherosclerosis is usually not increased, although total cholesterol levels may be increased. The lipoprotein profile in the same patient can change under the influence of environmental factors (for example, diet) and concomitant diseases.
3.5. Familial lipoprotein lipase deficiency (hyperlipoproteinemia type I). This rare disease, characterized by the absence of lipoprotein lipase activity and severe hypertriglyceridemia, typically presents in childhood. Few patients live to age 50, although their risk of atherosclerosis is not increased.
3.6. Familial mixed hyperlipoproteinemia. Due to excessive accumulation of apolipoprotein B-100 (hyperapobetalipoproteinemia), many patients have an increased risk of atherosclerosis. In 30-35% of patients and their relatives with dyslipoproteinemia, hypercholesterolemia is observed, in another 30-35% of cases hypertriglyceridemia is observed. In other cases, hypercholesterolemia is combined with hypertriglyceridemia. In some patients, with normal LDL-C, HDL-C is reduced; Small LDL-C may also be observed. The most common comorbidities are endogenous obesity, insulin resistance and diabetes mellitus.
3.7. Familial dysbetalipoproteinemia is a form of hyperlipoproteinemia type III. This is the result of a homozygous mutation in the Apo E gene (the mutation is contained in both Apo E genes located on both homologous chromosomes), weakening the binding of rhamnant lipoproteins to lipoprotein receptors, which impairs their catabolism and leads to an excess of unutilized chylomicrons and rhamnant VLDL-C. Such patients often experience early cardiovascular disease. Typically, this pathology is mild until other risk factors are added to it: alcohol consumption, hyperthyroidism, obesity, diabetes or kidney disease. In this case, triglycerides and total cholesterol often increase to the same extent as with hyperglyceridemia. The HDL-C concentration is typically normal. How then to distinguish dysbetalipoproteinemia from hyperglyceridemia? For a more accurate diagnosis of familial dysbetalipoproteinemia, ultracentrifugation is necessary (which is difficult in routine practice). The ratio of the concentrations of VLDL-C and triglycerides greater than 0.3 clearly indicates an enrichment of VLDL-C and, thereby, dysbetalipoproteinemia. Although most laboratories use the Freudwald equation (LDL C = total cholesterol - minus - [triglycerides/5) to determine LDL-C, this equation cannot be used for the clinical diagnosis of familial dysbetalipoproteinemia. In such patients, LDL-C concentrations must be determined directly. Most patients patients suffering from dysbetalipoproteinemia require drug therapy.
3.8. Secondary hyperglyceridemia. They are caused by poor diet and lifestyle. Their main reason is an “atherogenic” lifestyle: excess calories, excess alcohol consumption, lack of physical activity. Over time, this leads to obesity, insulin resistance, diabetes and cardiovascular disease. It is this kind of life that is the reason for the massive spread of metabolic syndrome in industrialized countries. Excess calories stimulate the synthesis of VLDL-C in the liver. This in turn increases triglycerides and decreases HDL-C and stimulates the formation of highly atherogenic small LDL-C. Moreover, excessive intake of saturated fat and cholesterol may decrease LDL-C receptor activity in the liver, thereby increasing LDL-C levels independent of changes in triglyceride concentrations.
Help Five factors of metabolic syndrome :
1) high triglycerides >150 mg/dl or 1.69 mmol/l, 2) low HDL-C <50 mg/dl or 1.29 mmol/l – for women; <40 mg/dL or 1.03 mmol/L for men; 3) high pressure - from 130/85 mm and above; 4) high blood glucose (from 110 mg/dL or 6.1 mmol/L and above); 5) waist size – more than 88 cm for women and more than 102 cm for men.
To make a diagnosis of metabolic syndrome, the presence of any three factors is sufficient.
Alcohol and Triglycerides Although alcohol increases lipid levels in most people, the effects of regular consumption can vary greatly. Alcohol has a greater impact on triglyceride levels than on HDL-C and LDL-C levels. Alcohol, as already mentioned, stimulates the synthesis of VLDL-C. This occurs because ethanol inhibits the oxidation of free fatty acids and thereby leaves more substrate available for the formation of VLDL-C. And then, excess VLDL-C is “converted” into atheroeic LDL-C (see # 1.2). And if an “atherogenic” life leads to insulin resistance, the likelihood of triglyceridemia increases. Insulin resistance reduces the activity of lipoprotein lipase, and this impairs the catabolism of both chylomicrons and VLDL-C.
Diabetes mellitus and triglycerides The predominant lipid metabolic disorder in diabetes mellitus is hypertriglyceridemia, caused by increased levels of VLDL-C and chylomicrons. The main reasons: 1) insulin deficiency in insulin-dependent diabetes mellitus: in some patients with insulin-dependent diabetes mellitus, the utilization of chylomicrons and VLDL-C is reduced, since insulin is necessary for the synthesis of lipoprotein lipase in adipocytes; 2) in patients with non- -dependent diabetes, excess insulin stimulates lipogenesis and the secretion of VLDL-C from the liver, 3) in patients with insulin- dependent and non -dependent diabetes mellitus without insulin resistance, hyperglycemia also enhances lipogenesis and the secretion of VLDL-C in the liver. In non -dependent diabetes mellitus, HDL-C often decreases, partly due to obesity. In general, the main disorders of lipoprotein metabolism in diabetes mellitus are as follows: accumulation of VLDL-C, small LDL-C, LDLP-C and rhamnate chylomicrons, as well as non-enzymatic glycosylation of apolipoproteins; lipoprotein(a) accumulation. In general, it is hyperglyceridemia, increased VLDL-C, decreased HDL-C and non-enzymatic glycosylation of apolipoproteins (due to excess glucose in the blood) that are the main risk factors for atherosclerosis in diabetes mellitus. Non-enzymatic glosylation of apolipoproteins leads to the fact that lipoproteins associated with cholesterol become “modified”, which induces an inflammatory process leading to endothelial dysfunction, which is the main factor of atherosclerosis. Therapy aimed at maintaining normal glucose levels can prevent or reduce the risk of atherosclerosis and reduce the severity of dyslipoproteinemia.
Kidney disease and triglycerides In nephrotic syndrome, due to increased cholesterol synthesis in the liver, the levels of LDL-C and VLDL-C are increased. LDL-C levels are inversely related to plasma albumin concentrations. Increases in LDL-C and VLDL-C are accompanied by hypertriglyceridemia (due to the accumulation of VLDL-C, VLDL-C, and residual chylomicron components) and a significant decrease in HDL-C. In kidney disease, lipoprotein(a) levels also increase. We also note that hypothyroidism also increases triglycerides, and in the same way as ethanol, indirectly, by reducing the activity of the LDL-C receptor.
4. Different triglyceride levels mean different goals of therapy.
4..1. With moderately elevated triglycerides – a decrease in atherogenic lipoproteins. According to the practice adopted in the USA, when treating patients with hypertriglyceridemia, the first goal should be to reduce LDL-C, and the second - all other “atherogenic” cholesterol, i.e., not related to HDL. In general, “non-HDL-C” or “atherogenic” cholesterol is: total cholesterol minus HDL-C. This convenient single indicator indicates the level of all atherogenic lipoproteins (LDL-C, VLDL-C and ramnate lipoproteins).
4.2. For high triglycerides - urgent reduction of triglycerides. Patients with triglyceride levels of 1000 mg/dL (11.2 mmol/L) or higher are at high risk of acute pancreatitis. Therapy should be aimed at reducing triglyceride levels and changing lifestyle: weight loss, reducing carbohydrate and alcohol consumption. Triglyceride levels respond particularly well to lifestyle changes, and better in men than in women. Losing just 4-5 kg of weight reduces triglyceride levels. Reducing the proportion of carbohydrates in the diet is very useful. In obese patients, a low-carbohydrate diet reduces triglycerides by 20-28%.
5 . Screening for triglyceridemia. US practice requires testing of triglyceride levels in all adults starting at age 20. In this case, the so-called “lipid panel” should be used, measuring 1) triglycerides, 2) total cholesterol, concentrations of 3) LDL-C and 4) HDL-C. If the risk of atherosclerosis is low, tests should be repeated every 5 years. Individuals with multiple risk factors for atherosclerosis should have their triglycerides checked more frequently. It is highly recommended that the patient fast for 9 to 12 hours before screening. In individuals at low risk of atherosclerosis, nonfasting screening may be performed, but if the results are alarming (HDL-C < 40 mg/dL or total cholesterol > 200 mg/dL), repeat measurements are performed on an empty stomach. Patients who have two or more risk factors should always be tested on an empty stomach. The results of lipid panel measurements can be distorted by: acute illnesses, infections, accidents (associated with cerebrovascular disorders), injuries, surgical operations, pregnancy, diet changes, weight loss.
And in conclusion, we emphasize once again that it is necessary to measure triglycerides because there are three reasons for this, namely: elevated triglyceride levels are: 1) a marker of atherogenic lipoproteins; 2) a marker of metabolic syndrome and, 3) extremely high triglyceride levels - a risk factor for pancreatitis.
Literature: Marie R, Grenner D, Mayes P, Rodwell W. Human biochemistry. In 2 volumes. T.1. Translation from English – M.: Mir, 2004.- 381 p., ill. Laboratory diagnostics. Ed. V.V. Dolgov and O.P. Shevchenko. - M.: Publishing house "Reapharm," 2005, 440 p. Dunbar RL, Rader DJ, Demystifying triglycerides: A practical approach for the clinician Cleveland Clinic J Med 2005, 5, N 8, 661-668. Nash DT, Cardiovascular risk beyond LDL-C levels. Other lipids are performers in cholesterol story. Postgrad Med. 2004; 116 (3): 11-15. Ozturk IC , Killeen AA, An Overview of Genetic Factors Influencing Plasma Lipid Levels and Coronary Artery Disease Risk Arch Pathol Lab Med. 1999; 123:1219–1222