In order to talk about why a low pulse occurs (bradycardia), it is necessary to recall a little the anatomy and electrophysiology of the heart.
The heart has two atria and two ventricles. First, the atria contract, driving blood into the ventricles of the heart, then the ventricles contract, throwing blood into the largest vessel, the aorta, and through it the blood is distributed to all organs and tissues.
What makes the heart beat?
Like any organ, the heart has a conducting system, in other words, wires through which “current” flows to its various parts. The “electric current” originates spontaneously in the sinus node (a small point in the wall of the right atrium). This node is necessary for generating an impulse and adjusting the frequency of contractions depending on the needs of the body, for example, when we run it speeds up the heart, and when we sleep it slows it down.
From the sinus node, the impulse first goes to the atria, causing them to contract. Then the “wires” merge into one so-called “switch” or AV node (it is located in the middle of the heart between the atria and ventricles, in this node there is a slight delay in the passing “current” for the full contraction of the atria), then the impulse passes to the ventricles. In the ventricles, the “wires” branch and are called the bundle branches (left and right; the left, in turn, is further divided into the anterior branch and the posterior branch) with their help, the impulse causes contraction of the ventricles of the heart.
Age-related changes in heart rate
Typically, heart rate changes with age due to degenerative disorders in the circulatory system. In older people, the pulse becomes less frequent, which indicates stretching of the walls of blood vessels and a decrease in their blood supply.
At the beginning of life, the heart rate is unstable and very often irregular, but by the age of seven the pulse parameters become stable. This feature is associated with the functional imperfection of the neurohumoral activity of the myocardium. In emotional and physical rest in children 7-12 years old, heart contractions do not tend to slow down. In addition, during puberty, the heart rate increases. And only from the age of 13-14, processes are activated that help slow down heart contractions.
In childhood, the heart rate is higher than in adults, which is associated with rapid metabolism and high tone of the parasympathetic nervous system. An accelerated pulse plays a major role in ensuring minute blood volume, which guarantees the necessary blood flow to tissues and organs.
Why might your heart rate drop?
Unfortunately, this entire system can break down at different stages and lead either to a decrease and/or cessation of the flow of “current” (blockade) or to incorrect conduction of the impulse in various parts of the heart:
- The first “breakage” may be at the level of the sinus node itself. For various reasons, organic or functional, it loses the ability to produce the required number of impulses. For example, no matter how much a person runs or climbs the stairs, the sinus node cannot rise above a hundred beats, which may result in increased shortness of breath or weakness.
- The second “breakage” may be at the level of the atrioventricular (AV) node. Let me remind you that it is located between the atria and ventricles, an impulse passes through it from the atria to the ventricles; it is needed in order to create a short physiological pause for a more complete contraction of the atria. At this level, all kinds of blockades (AV blocks) can occur. They come in different degrees, 1st, 2nd or 3rd degree depending on the severity of the condition. From the name it is clear that they block the impulse at this stage, as a result the ventricles of the heart cannot contract, this leads to pauses, sometimes significant ones (3 or more seconds); for example, depending on the body’s reserves and concomitant pathology, starting from a 3-second delay in heart contraction, a person may begin to briefly lose consciousness; as these blockades progress, consciousness, sometimes, may not return. Let us reassure you a little: nature has come up with life-saving “(emergency) stations” for generating backup impulses; they are located at all stages of the conduction system, but the “lower” they are located, the less “current” they are able to reproduce. So, in case of this breakdown, the “backup generator” is already in the ventricles and is capable of delivering a maximum of 40 beats or less, so that this can allow one to “hold out” to the resuscitation ambulance team.
- The third “breakdown” can occur below the atrioventricular (AV) node at the level of the bundle branches (these are “wires” that extend from the atrioventricular node and excite the ventricles; we will talk about them in more detail in another article).
Unfortunately, these legs can also be partially or completely blocked due to various reasons, thereby preventing the full contraction of the ventricles of the heart.
general characteristics
Arterial pulse is a rhythmic contraction of the arterial wall caused by the release of blood during contraction of the heart muscle. Pulse waves are formed at the mouth of the aortic valve during the period of blood ejection from the left ventricle. The stroke volume of blood occurs at the moment of increase in systolic pressure, when the diameter of the vessels expands, and during diastole, the dimensions of the vascular walls are restored to their original parameters. Consequently, during the period of cyclic contractions of the myocardium, a rhythmic oscillation of the aortic walls occurs, which causes a mechanical pulse wave that spreads to large and then to smaller arteries, reaching the capillaries.
The mechanism of pulse wave formation in blood vessels
The further the vessels and arteries are located from the heart, the lower the blood and pulse pressure becomes. In the capillaries, pulse fluctuations are reduced to zero, which makes it impossible to feel the pulse at the level of the arterioles. In vessels of this diameter, blood flows smoothly and evenly.
What causes these “breakdowns” in the conduction of impulses?
- Diseases leading to overload and hypertrophy of the ventricles such as cor pulmonale, congenital and/or acquired heart defects with increased load on the right and/or ventricles (for example, mitral and aortic stenosis/insufficiency or septal defects), arterial hypertension, myocardial infarction various localizations, cardiomyoptia, myocardial dystrophy, etc.
- Various congenital anomalies of the development of the cardiac conduction system (Brugada syndrome)
- Age-related changes (cardiosclerosis)
- Idiopathic (acting as a separate disease, causeless) calcification or sclerosis of the cardiac conduction system
- Also, a low heart rate in itself can be normal in trained athletes (it can reach up to 35 beats per minute)
- changes in the electrolyte composition of the heart (hyperkalemia or hypercalcemia)
- Non-cardiac causes (increased intracranial pressure, decreased body temperature, hypothyroidism, etc.)
How to measure your pulse correctly
Wave-like fluctuations in the blood are clearly noticeable when touching certain parts of the body. Those under the skin of which large arterial vessels are located. To measure the frequency and assess the rhythm of the pulse, you should apply your fingers: fixing them at one point quite tightly, but without strong pressure. Areas to check for pulsation:
- carotid artery: a point on the front surface of the neck, on the right, under the jaw;
- radial artery: on the inside of the wrist of the left or right hand;
- temporal artery: on the side of the left or right temples;
- brachial artery: on the inner surface of the elbow;
- popliteal: in the area of the popliteal folds of the legs;
- femoral: at the junction of the pelvis and lower limbs.
The measurement accuracy is the same for all methods. The most popular methods remain recording the pulse on the wrist or neck. To calculate its frequency, it is important to use a stopwatch or electronic timer. Applicable time interval: 1 minute. It is necessary to measure at rest, preferably before eating: for example, after waking up or during a period of rest.
The rhythm and force of the beats cannot be assessed without the use of special instruments. But with the manual method, sudden changes in the nature of the pulsation are noticeable. Normally, it is measured, at equal intervals, without acceleration or fading. If the blood impulses are poorly palpable, too weak or uneven, this is an unfavorable sign. You should undergo a detailed diagnosis.
Therapy methods
To treat pulse deficiency in the absence of complications, drug therapy is prescribed; it is selected under the control of ECG and blood pressure. During an attack, Cordarone or Novocainamide is administered intravenously, then switched to tablets. With a permanent form of atrial fibrillation, Propanorm (Ritmonorm) for oral administration may be recommended.
If a pulse deficiency occurs against the background of sinus or paroxysmal tachycardia, extrasystole, then Verapamil, Concor, Norvasc helps. For heart failure, Digoxin and Strophanthin are used. They are usually combined with anticoagulants (Warfarin, Aspirin).
If drugs fail to normalize the rhythm, then the method of electrical cardioversion is used. It involves applying a pulsed electric discharge to the heart area. This gives results in 90% of cases.
To radically eliminate arrhythmia, cauterization of the focus is carried out using radio waves, in which frequent pulses are formed using radiofrequency ablation. The second method is to create a complete blockade of impulse transmission, then the atrioventricular node is destroyed with an electrode. Then the conduction of impulses completely stops, and a permanent pacemaker is installed to stimulate contractions.
Pulse deficiency is a symptom typical of the heart contracting ineffectively and not pumping out enough blood. In most patients, it occurs against the background of atrial fibrillation, which complicates the course of coronary heart disease. With a small difference between heart contractions and pulse, there may be no symptoms, but a pronounced deficiency in pulse leads to cardiac weakness and poor circulation.
How dangerous is the condition?
Pulse deficiency leads to insufficient blood flow into the aorta, which is accompanied by shortness of breath, which worsens with little physical activity. Patients feel palpitations, pain and interruptions in heart rhythm, pulsation of the vessels of the neck. Possible sweating, weakness, trembling of limbs, lightheadedness or loss of consciousness.
Such symptoms are most often difficult to tolerate during attacks, but with a permanent form, the body adapts over time, and patients no longer feel the irregular heartbeat. But at the same time, the heart muscle weakens, which leads to severe heart failure with blood stagnation in all organs. An acute form is possible in the form of cardiac asthma and pulmonary edema, as well as a chronic form with expansion of the cavities of the heart.
Due to too frequent but ineffective contraction of the heart and lack of coordination between its parts, blood clots form inside the cavities. They can block the flow of blood, which can cause cardiac arrest. Smaller clots enter the brain vessels and cause acute cerebrovascular accident (stroke). The low volume of blood entering the aorta leads to a drop in pressure and the development of arrhythmogenic shock with loss of consciousness. It is very difficult to treat and has a high mortality rate.
If the pulse deficit does not exceed 10 beats and occurs periodically, then its occurrence does not disrupt intracardiac and systemic (general) circulation. Typically, patients have no complaints and remain in satisfactory health. Sometimes you may experience slight dizziness or weakness during intense physical activity. This variant of pulse deficiency is considered harmless.
Symptoms
If the pulse decreases significantly, the person experiences:
- weakness of the body as a whole;
- headache of varying strength;
- numbness in the limbs and a decrease in their temperature;
- problems with vision, attention, concentration.
Once again, it is worth emphasizing that symptoms are not always immediately visible, so it is worth, especially in old age, to measure your pulse immediately after waking up.
Actions when your heart rate is low
Bradycardia can be dangerous, because with rare contractions of the myocardium and slow blood circulation, hypoxia develops. Oxygen starvation has an extremely negative effect on the brain and causes loss of consciousness. If a person is not given prompt assistance, breathing may stop. This is why it is important to know exactly what to do when your heart rate is low.
Help with a decrease in heart rate depends on the reasons that cause it. If we are not talking about heart disease, you can cope with the problem on your own:
- Take Corvalol;
- Drink 20 drops of motherwort twice a day;
- Take Zelenin drops until the pulse is completely restored (the drug has contraindications: organic damage to the heart, pancreas, vision).
If the pulse decreases due to heart disease or other pathologies, you must call an ambulance. Before the doctor arrives, the person must be positioned so that the legs are higher than the heart. For breast tenderness, you can give nitroglycerin, a fast-acting drug that provides relief in just 5 minutes. Belladonna extract can help with the first attacks of bradycardia, but its effect takes about half an hour.
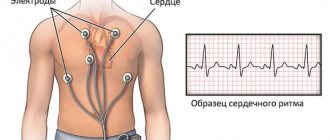
Determination methods
The study of the arterial pulse is carried out on the main (carotid) and peripheral (wrist) arteries. The main point for determining heart contractions is the wrist, where the radial artery is located. For an accurate examination, it is necessary to palpate both hands, since situations are possible when the lumen of one of the vessels may be compressed by a thrombus. After a comparative analysis of both hands, the one on which the pulse is better palpated is selected. When examining pulse impulses, it is important to place your fingers so that 4 fingers are on the artery at the same time, with the exception of the thumb.
Determination of pulse fluctuations on the radial artery
Other ways to determine your pulse:
- Thigh area. The study of pulse impulses on the femoral artery is carried out in a horizontal position. To do this, you need to place your index and middle fingers in the pubic area, where the inguinal folds are located.
- Cervical region. The carotid artery is examined using two or three fingers. They should be placed on the left or right side of the neck, 2-3 cm away from the lower jaw. It is recommended to carry out palpation from the inside of the neck in the area of the thyroid cartilage.
Determining the pulse on the radial artery can be difficult in case of weak cardiac activity, therefore it is recommended to measure the heart rate on the main artery.
First aid for bradycardia
The selection of medications for the correction of pathological changes is carried out by the attending physician, taking into account the etiological factor of the condition. If the relationship between pulse and pressure is abnormal, it is contraindicated to take drugs from the group of beta blockers and calcium antagonists, as they cause a sharp decrease in blood pressure and inhibition of the activity of the sinus node. The drugs of choice are drugs from the class of ACE inhibitors, which have a smooth mechanism of action. However, if there is a sharp deterioration in the condition, every hypertensive patient should know what to do at home to stabilize the indicators.
During an attack, the following measures should be taken:
- Take a horizontal position on your back, while your torso should be slightly raised.
- Wrap the lower limbs in a blanket, apply a heating pad or mustard plasters to the feet.
- Take medicine (Losartan, Lasix, Amlodipine, Captopress).
In cases where an increase in blood pressure occurs even with a slight decrease in heart rate, but is accompanied by a sharp deterioration in condition, it is necessary to call an ambulance or transport the patient to a hospital.
More often, pulse deficiency is typical for those
Pulse deficiency in the vast majority of cases is associated with heart disease; it is typical for patients with diagnoses:
- coronary heart disease – myocardial infarction, angina pectoris;
- cardiosclerosis after a heart attack or inflammation of the heart muscle (myocarditis);
- heart disease;
- extensive myocarditis, rheumatic carditis;
- cardiomyopathy (myocardial damage without inflammation due to metabolic disorders or high blood pressure);
- severe course of heart failure, hypertension.
Atrial fibrillation can also occur as an independent disease when its cause cannot be determined. Such patients are diagnosed with idiopathic atrial fibrillation.
Predisposing factors include:
- increased thyroid function (hyperthyroidism, thyrotoxicosis);
- abuse of alcohol, caffeinated drinks;
- overdose of cardiac glycosides or heart stimulants (for example, Adrenaline, Dopamine);
- frequent stressful conditions, overwork, lack of sleep;
- deficiency of potassium in the blood (use of diuretics, loss through sweat, diarrhea, vomiting);
- diabetes;
- obesity;
- smoking;
- chronic, long-term diseases of the kidneys and lungs.
What affects a sleeper's heart rate?
Pulse is one of the types of biomarkers, relying on its indicators to determine the general condition of the human body. At the time of sleep, jerky oscillations in the artery decrease, the functions of the cardiovascular system slow down, and metabolic processes weaken. Cells require less oxygen.
This process regulates the activity between organs, some are stimulated, others, on the contrary, arrive in complete relaxation. Heart rate and intensity are affected by:
- gender identity;
- age;
- physical state.
The more trained a person is, the lower the heart rate reduction. For men, the difference is considered to be in the range of minus 5-10 beats. In children, compared to the older generation, pulsation increases by 25-30 beats/minute.
Pulse deficiency is observed under what conditions, the reasons for its occurrence
The most common causes of pulse deficiency are associated with the release of a small volume of blood into the aorta, this is possible in the following conditions:
- atrial fibrillation (uncoordinated contractions of the atria with insufficient filling of the ventricles);
- extraordinary contraction (extrasystole), which occurs after the usual one, the ventricle does not have time to receive the full volume of blood;
- an attack of tachycardia (a rare cause), when contractions are so frequent that in some cases there is no full flow of blood into the aorta.
If the filling of the ventricles with blood is below normal, but the internal pressure on the aortic valve is sufficient, then ejection occurs, and with a very small amount, the heart contracts, but the valves are completely closed. In the first case, a weak pulse wave occurs, it quickly subsides, and in the second, there is no blood flow into the arterial network at all.
With atrial fibrillation with tachysystole (frequent contractions), the pulse deficit is constantly present. In such patients, the heart works at an increased rate, wears out faster, and the blood supply is not enough to nourish the internal organs, the brain and the heart muscle itself.
With extrasystole and paroxysmal (attack-like) tachycardia, pulse deficiency usually occurs periodically; it is rarely detected during a routine examination of the patient; daily monitoring (control) of two indicators is required.