home
/
Articles
/
How to place an IV at home for a patient with “bad” veins?
An IV is considered a simple medical procedure, but requires certain knowledge and experience. It is strictly not recommended to carry out the procedure of intravenous infusions on your own due to the high risk of complications.
To install an IV at home with the help of a nurse, you don’t need a lot of money: a specialist will do everything professionally, in compliance with the rules. True, it is not always possible to avoid difficulties during infusion, especially if the patient has inconspicuous, thin and fragile veins that are not easy to reach.
Content
- Why are IVs placed in the veins in the arms?
- What is poor venous access?
- Causes of “bad” veins in the arms
- 5 proven ways to find a vein Physical activity
- Squeezing
- Warming
- Gravity
- Fluid replacement
- Tools and accessories
Causes of pathology
The main reasons for the development of vein thrombosis are:
- Damage to the walls of blood vessels. Injury can be caused by infections, atherosclerotic plaques, childbirth, surgery, poor nutrition, and excessive physical activity.
- Blood clotting disorder. The problem occurs due to metabolic disorders or hormone balance in the body.
- Stagnation of blood. Occurs as a result of a sedentary lifestyle.
- Infectious diseases, pathologies of internal organs (heart failure, diabetes mellitus).
- Oncology and its treatment (hormones, chemotherapy, radiotherapy).
Indirect risk factors that influence the likelihood of pathology occurring are bad habits, wearing tight clothing, and adverse effects of the external environment.
Why are IVs placed in the veins in the arms?
It is no coincidence that the veins in the arms are chosen for medical procedures, since they have the most suitable structure for this. On the upper limbs there are deep and superficial vessels. The latter lie close to the surface of the skin, making it easy to draw blood from them.
The pressure in them is only 5-10 mmHg (in the arteries in the arms it can be 139 mm), the venous wall contains a small number of muscle cells, is pliable and stretches well. In addition, the skin on the hands is much thinner than on the feet, so it can be pierced without causing severe pain to the person.
After a puncture, a small scar appears on the wall of the vein - the same as after damage to the skin in any other place. It can persist for a long time - months and even years. The integrity of damaged venous walls is never completely restored, but changes (if there are not too many of them) do not have a significant impact on the functioning of the body.
What is poor venous access?
The situation when a nurse cannot get into a vein is familiar to about a third of patients who have received intravenous injections or an IV at home or in a hospital setting at least once in their lives. The reason is not always the inexperience of the medical worker. Sometimes even specialists with extensive experience do not get to the right place the first time - most often this happens when venous access is difficult.
Normally, the veins should protrude slightly above the skin between the muscles and have a bluish or blue tint. But for some people, they are too thin or almost invisible, making it difficult to insert the needle. In nursing practice, there are cases when a vein is difficult not only to see, but also to palpate. Then experienced specialists use proven methods to find a vein and place an IV in the place where this is easiest to do.
Course of the disease
The course of the disease is divided into two stages: acute (lasts about three weeks; at the initial stage, symptoms appear during physical activity) and chronic (symptoms last for more than two months).
The acute phase is characterized by increasing swelling of the arm, pain, and a feeling of fullness. The patient's ability to work decreases. Gradually, tense saphenous veins develop, which take on the function of outflow of venous blood and contribute to the subsidence of the process.
The chronic phase is the consequences of thrombosis. With inadequate treatment, occlusion of the subclavian vein persists and chronic Paget-Schroetter syndrome develops. It is characterized by the development of a powerful collateral network of saphenous veins around the shoulder joint. Patients are concerned about the increase in volume of the sore arm, sometimes there is pain and increased fatigue.
Causes of “bad” veins in the arms
Inconspicuous, thin or fragile veins are a serious problem for those who perform medical procedures. There can be several reasons for this phenomenon, ranging from natural causes to taking medications and frequent injections:
- Features of the body. The pattern and location of the veins are individual for each person, therefore they are the same unique biometric characteristic as a fingerprint or iris pattern. Accordingly, “hidden” vessels may be a feature of the body.
- Genetic predisposition. The strength of venous valves is genetically determined. According to statistics, if both parents suffer from varicose veins, the probability of their children inheriting it is about 80%. The same goes for fragile or thin veins - they are often a family problem.
- Aging. Venous access worsens with age - this is due to a decrease in elastin and collagen content, as well as thinning of subcutaneous fat. The skin becomes thin, “papery”, and the veins become thin and fragile, which increases the risk of injury and bleeding.
- Excess weight. In people with a high BMI (body mass index), the veins are hidden under fat. With obesity, it is difficult to perform not only intravenous injections and drips, but also some diagnostic procedures - ultrasound, MRI.
- Frequent injections. Any injection represents an injury, and if there were too many of them, scars form in place of healthy tissue. The veins “hide” and harden, so it becomes more difficult to place an IV or give an injection.
- Regular drug administration. In addition to frequent injuries, venous access in drug addicts deteriorates due to the administration of caustic, aggressive drugs. They literally burn the venous walls, making it extremely difficult for long-time drug addicts to carry out medical procedures.
- Exposure to ultraviolet radiation. Ultraviolet rays can also destroy elastin and collagen, which is why venous access is often difficult in people who are frequently exposed to the sun.
- Taking medications. Some drugs worsen the condition of the veins and increase the risk of complications during catheterization. Corticosteroids cause atrophy of the epidermis, and anticoagulants increase the risk of bleeding.
Poor venous access may be a transient phenomenon. If a person is stressed (for example, afraid of injections) or is cold, finding a vein to place an IV can be difficult.
Prevention
The development of venous thrombosis can be prevented. There are a number of generally accepted recommendations, adherence to which will help avoid problems with the cardiovascular system:
- Use elastic bandages as prescribed by a doctor. They help maintain blood vessels in tone and prevent congestion in the limbs.
- Quitting smoking and alcohol. Bad habits have a sharply negative impact on all body systems, being a major risk factor for the development of cardiovascular diseases.
- Rational, proper nutrition. Refusal of fatty, fried, salty, smoked, flour, and sweet foods is the key to a healthy heart and blood vessels. The diet should be complete and varied. Eat more vegetables and fruits, whole grain cereals, poultry, fish, and dairy products. Limit your pork consumption. Try to eat more greens, add natural seasonings and spices to your dishes. Avoid sausages, hot dogs, and processed foods.
- Taking vitamins and microelements. It is necessary to visit a doctor and get tested for a lack of certain vitamins in the body. Based on the results of the study, the specialist will prescribe the most suitable medications for your case.
- Optimal physical activity. Stagnation in the bloodstream should not be allowed. Doctors recommend walking for at least half an hour every day. If you have a sedentary job, you should spend 3-5 minutes exercising every hour. It is also necessary to monitor your posture and stretch regularly to restore normal blood flow.
- Adequate fluid intake. Water is vital for the body to function properly. Make it a habit to drink a glass of clean water in the morning, before bed and before every meal.
- Refusal to visit the bathhouse, sauna, or take hot baths. Exposure to high temperatures does not have the best effect on the heart and blood vessels. And if there is a genetic predisposition to varicose veins and thrombus formation, bath procedures significantly increase the likelihood of developing vascular bed pathologies.
- Normalization of weight. Obesity negatively affects the condition of the cardiovascular system. Fatty deposits in tissues and internal organs compress veins and arteries, which impairs blood circulation and significantly impairs the delivery of vital substances to the tissues.
- Timely treatment of concomitant diseases. Malignant and benign tumors, inflammatory processes in internal organs - all this negatively affects blood circulation, which can lead to blockage of blood vessels.
- Control of cholesterol and blood glucose levels. These are vital signs that need to be monitored constantly. Controlling cholesterol levels will help avoid the development of atherosclerosis, which is one of the most common causes of varicose veins. Sugar levels must be monitored in order to promptly notice negative changes that can lead to diabetes.
- Regularly undergoing comprehensive examinations. This is especially true if your closest relatives have cardiovascular pathologies. These diseases are classified as hereditary. Therefore, “keeping your finger on the pulse”, you will be able to detect in time even the slightest changes in the functioning of the heart or the condition of the blood vessels.
The state of a person’s cardiovascular system directly depends on his lifestyle. Serious pathologies can be prevented by following the above recommendations. If the problem already exists, do not put off visiting a doctor. Contact trusted, reliable specialists, undergo a comprehensive examination, consult a doctor about available treatment methods. Don't risk your health. Thrombosis is very dangerous!
Still have questions about vein thrombosis?
Free consultation with AngioClinic specialists
Author
Salmina Daria Vladimirovna
Geneticist. Graduated from the Chelyabinsk State Medical Academy. She completed an internship at the Northwestern State Medical University named after I.I. Mechnikov.
How to properly place an IV: procedure algorithm
In order to administer an intravenous infusion, appropriate knowledge, experience and strict adherence to technique are required. Correct placement of a drip is not only about inserting a needle without consequences for the patient, but also about choosing a system, infusion rate, etc.
Tools and accessories
To carry out the infusion, it is necessary to prepare the medications prescribed by the doctor (check the expiration date, volume and other important indicators), as well as instruments and consumables:
- Dropper stand. It is a portable stand with hooks onto which containers with solutions are placed. Its height is 1.5-2 m, which provides sufficient pressure for insertion.
- Infusion system. Droppers differ in the diameter of needles, tubes and the speed of infusion of drugs. It is very important to decide on the size of the needle, which is inversely proportional to the number: twenty-second is the thinnest, fourteen is the thickest. It depends on the anatomical features of the patient and the characteristics of the drug.
- Related accessories. In addition to a tripod and a system for placing an IV, you will need a tourniquet (it helps to find the vein), a patch to fix the needle and cotton wool.
In addition to the prescribed medications, you need to prepare an antiseptic liquid. Most often, alcohol is used; if a person has allergies, they take alcohol-free solutions (for example, Chlorhexidine).
Preparation for the procedure
Before manipulations, be sure to wash your hands and wipe them with an antiseptic. Failure to comply with hygiene rules can lead to infection and sepsis, even if the health worker has perfect infusion technique.
- Connect the system to the container or package with the drug. To do this, you need to wipe the needle with alcohol and pierce the cork - this is not difficult, since they are made of soft rubber or other materials.
- Hang the containers on the racks and secure them well. Be sure to check that there is no air in the system - fill the tubes and drip chamber about a third with liquid. Small bubbles are usually not dangerous - they will stick to the walls of the container and will not enter the bloodstream.
If sterility is violated at one of the stages, infusion is strictly prohibited. This can lead to blood poisoning and other dangerous consequences.
Placement of the IV
Before the procedure, it is necessary to familiarize the patient with the features of its implementation. Each drug has a special effect on the body, and some sensations may frighten a person. It is important to distinguish the side effects of drugs from the alarming symptoms that develop when infusions are performed incorrectly. Pain, dizziness, nausea, weakness and other discomfort should be reported to a healthcare professional immediately. The procedure algorithm is as follows:
- the patient takes a comfortable position - it is best to do the IV while lying down, but it is also possible in a semi-sitting or sitting position;
- the arm in the biceps area is tied with a tourniquet, the needle insertion site is thoroughly disinfected;
- the needle is inserted into the darkest, well-filled vein parallel to the surface of the arm at an angle of 35-45 degrees;
- after blood appears in the catheter, it is positioned as parallel to the limb as possible and fixed with an adhesive tape;
- connect the system tube to the catheter, make sure the connection is tight, and additionally secure it with a bandage;
- The rate of supply of the solution is adjusted using a dial with a wheel - sometimes the number of drops is marked on it to make counting easier.
During the procedure, it is necessary to monitor the patient and the needle insertion site. If the fluid flows too quickly, the person may become dizzy. In such a situation, it is better to simply reduce the infusion rate by turning the wheel in the desired direction.
After completing the procedure, it is necessary to close the system, carefully remove it, apply cotton wool soaked in alcohol to the injection site and press well. You need to keep it for at least 10-15 minutes, and preferably 20-25 minutes. During this time, a blood clot will form, which will clog the wound. If you remove the cotton too quickly, drops of blood will get under the skin, resulting in a bruise or bruise. Do not rub or touch the injection site, as this can also lead to the accumulation of blood clots.
Complications from improper infusion
When carrying out the procedure, it is necessary to strictly follow all the rules - placement technique and asepsis. An incorrectly placed IV carries the risk of complications, which include:
- bruise or hematoma at the injection site;
- vessel damage;
- bumps under the skin due to the accumulation of the drug;
- unintentional introduction of a small (infiltration) or significant (extravasation) amount of solution into surrounding tissues;
- vein spasm;
- inflammation of the vein with the formation of a blood clot;
- tissue infection;
- air embolism.
Complications also include allergic reactions to the drug. They can be minor (itching and rash in the area where the solution was administered) or severe - Quincke's edema and anaphylactic shock. In any case, the patient should be left under the supervision of a doctor - sometimes minor allergic reactions lead to serious consequences.
What to do if complications develop?
The most dangerous complication of an incorrectly placed IV is an air embolism, or air bubbles entering the bloodstream. It rarely causes death - according to experts, in order to cause death, at least 200 ml of air must be injected into the vein. A small bubble simply dissolves in the cells, but sometimes it can impair the functioning of vital organs, so it is better not to take risks.
Symptoms of an air embolism depend on the size of the vessel affected and the amount of air trapped. The affected area swells, becomes painful, the skin turns blue or red, after which trophic ulcers and necrotic areas form. Tachycardia is possible, as well as manifestations from the affected organs. With pulmonary embolism, hemoptysis and pulmonary edema are observed, if the coronary or cerebral arteries are affected, heart attacks and strokes are possible with all the ensuing consequences. If signs of embolism appear, the patient should be hospitalized immediately.
Dangerous complications when intravenous infusion technique is violated include infiltration and extravasation, which can lead to unpleasant consequences. Injecting large amounts of medication past the veins can lead to severe tissue damage and necrosis. Treatment is carried out in a hospital under medical supervision.
The appearance of hematomas and bruises does not always depend on the experience or qualifications of the nurse. In some patients, the vessels are so fragile that they burst when the needle is inserted, resulting in a bruise. Such complications are not dangerous to health, but can sometimes lead to unpleasant consequences requiring medical intervention. You should consult a doctor if you have the following symptoms:
- painful sensations that increase and do not disappear for 2-3 days;
- increase in size of the bruise;
- muscle spasms;
- difficulty moving your hand;
- deterioration in general health (weakness, fever, headache);
- increased temperature at the site of the bruise.
Such signs indicate that an infection has entered the body, and sometimes the onset of necrotic processes. Normally, bruises disappear within 2-3 weeks, gradually changing color from bluish-purple to greenish and yellow. A bruise that does not go away for a long time is also a reason to consult a doctor, even if it is not accompanied by pain or malaise.
Phlebitis, or inflammation of the venous walls, usually develops after prolonged treatment with intravenous infusions, but when infected or administered caustic, irritating drugs, it can develop after several procedures. The vein area becomes dense and painful, body temperature rises to 38-39 degrees. Phlebitis is treated conservatively (anticoagulants, anti-inflammatory drugs) in combination with physiotherapy.
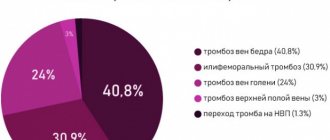
Where does thrombosis most often occur?
70% of diagnosed cases of venous thrombosis are localized in the lower extremities. The remaining 30% comes from the upper body. Let's consider the areas of the torso and upper extremities where pathology occurs most often.
Subclavian region
Thrombosis of the subclavian vein develops as a result of excessive physical activity and stress. Signs of pathology appear in influxes - sometimes intensify, sometimes disappear. This is due to the absence of serious consequences from thrombosis of the subclavian vein - blood circulation is replaced by other vessels. However, this blood is not enough to fully nourish the tissues of the upper extremities, as a result of which degenerative processes are inevitable.
The main signs of subclavian vein thrombosis are:
- pain in the arm area;
- transillumination of the venous pattern through the skin;
- swelling of the hand, the appearance of a glossy shine;
- numbness of the limb, twitching and other signs of a neurological disorder.
In the absence of correct treatment, the pathology can enter the chronic phase. Then the clinical picture of the disease becomes blurred, and the reaction of the injured limb to external stimuli is significantly reduced. The motor activity of the hand is limited, and muscle atrophy develops. Any physical activity is accompanied by acute pain. In some cases, the patient may even be assigned a disability.
Hands
The pathology has pronounced symptoms. Accompanied by redness in the area of blood clot formation, a feeling of pulsation, and pain. Neurological symptoms may also be present - twitching of the limb on the problematic side, numbness, significant limitation of motor activity. Pain in case of thrombosis can radiate to the lower back, spine, and sternum area.
Manifestations of the disease make themselves felt sharply and disappear just as quickly. Many patients confuse the symptoms of thrombosis of the veins of the arm with a pinched nerve, ignoring a trip to the doctor. However, at the first signs of circulatory problems or the appearance of acute pain, it is necessary to urgently consult a specialist.
Brachial vein
A fairly rare condition, most often occurring in young patients. It is diagnosed mainly in men. It is called Paget-Schroetter syndrome. The main signs of brachial vein thrombosis are:
- sudden pain in the shoulder area;
- feeling of warmth, burning in the affected area;
- swelling, swelling in the shoulder area;
- redness, and after 2-3 hours the skin in the problem area turns blue.
The pathology almost completely blocks the blood supply to the upper limb. Needs immediate treatment. Ignoring signs of the disease can lead to pulmonary embolism. This condition involves a blockage of the lung by a blood clot. Without emergency medical attention, this complication of thrombosis can be fatal.
Cervical veins
Jugular vein thrombosis is also diagnosed quite rarely. This is a dangerous condition - with the slightest physical exertion, a blood clot can migrate to the heart, leading to thromboembolism. The main symptoms of the pathology are:
- the appearance of edema in the jugular vein;
- tension, noticeable swelling of the vein;
- a feeling of itching and heaviness in the affected area, redness of the skin;
- weakness in the body, dizziness;
- a more pronounced manifestation of the venous pattern in the neck.
The main reasons for the development of the disease are excessive blood viscosity, problems with blood flow speed in the presence of malignant neoplasms, and concomitant cardiovascular pathologies.
Axillary area
Thrombosis of the axillary vein occurs three times more often on the right, often occurring on both sides. Pathology in this area develops as a result of repeated repeated injury to the veins due to their compression. The main symptoms of the disease are:
- swelling of the upper limb;
- intense pain syndrome, significantly intensifying after physical activity;
- in some cases, the pathology is accompanied by cyanosis of the hand;
- visual expansion of the vein, visible to the naked eye;
- redness of the skin in the affected area.
Signs of thrombosis appear suddenly and disappear just as suddenly. Ignoring the symptoms of the disease is fraught with the development of venous hypertension, detachment and migration of a blood clot under the influence of the slightest physical exertion.
How to safely place an IV in case of “difficult” veins?
When inserting a needle into a person with thin, fragile, or hard-to-see veins, additional precautions must be taken. They allow you to avoid unpleasant consequences in the form of injuries, hematomas and bruises, and also make the procedure as painless as possible:
- Do not stretch the skin excessively. If the veins are pronounced enough to get to the right place, you can do without a tourniquet. Otherwise, it is better to take a soft tourniquet and not tighten it too much - this is especially true for older people, as well as patients with thin skin and fragile veins.
- Reduce the number of procedures. If possible, it is necessary to reduce the number of vein punctures - administer several drugs in one dropper or one after another. Do not forget that mixing medications yourself can lead to undesirable consequences - this issue should be discussed with your doctor.
- Use a needle with a small diameter. To administer most solutions, a needle with a minimum diameter is sufficient. Exceptions include viscous, thick preparations; extreme caution should be exercised when administering them.
- Do not press the needle too hard. If the needle is sharp enough, there is no need to press too hard. For insertion, a smooth, gentle movement with slight pressure is sufficient.
- Insert the needle parallel to the skin. This is done in order to reduce the risk of through vein puncture. The skin over the vessel should be slightly stretched and secured so that it does not slip.
- Do not rush. When placing an IV, haste can lead to unpleasant consequences - you need to act slowly and carefully.
When the needle is inserted correctly, the patient feels slight discomfort when applying a tourniquet and performing a puncture. Unpleasant sensations during the infusion of the solution, including dizziness, nausea, weakness and darkening of the eyes, indicate that the infusion is not going properly.
Treatment with surgery
If the blood clot threatens the patient's life, surgery is indicated. The surgical technique is selected by the doctor based on the results of a comprehensive examination. There are several ways to surgically treat thrombosis.
Bypass surgery
The operation involves removing the affected section of the vein along with the blood clot and replacing it with a natural vascular implant taken from another part of the patient’s body. In some cases, an artificial vessel prosthesis can be used. The intervention is performed through abdominal access. After the operation, the patient will have a long rehabilitation period.
Thrombectomy
It involves surgical intervention aimed at removing a blood clot from the vessels. Depending on the location of the thrombus and its size, the following may be used:
- Traditional technique. To remove the blood clot, abdominal access is provided. The patient is put into medicated sleep. The operation lasts several hours, the rehabilitation period is 3-4 weeks. This is a serious intervention that is prescribed only in extreme cases.
- Endovascular technique. It involves removing a blood clot through a femoral approach using modern instruments. It is used in case of a small blood clot.
The main indications for thrombectomy are:
- closure of a large vessel with a thrombus;
- During the diagnosis, a large blood clot was discovered that interfered with normal blood flow in the vessels;
- the appearance of a floating thrombus;
- pregnancy;
- a critical health condition of the patient in which a blood clot threatens the patient’s life.
It is important to understand: none of the above methods provides a guarantee that a blood clot will not form again. To avoid the recurrence of thrombosis, the patient must strictly follow all the doctor’s recommendations, as well as radically change his lifestyle.
How can you tell if the medicine is going past the veins?
To prevent infiltration and extravasation, the patient must be closely monitored during the procedure. List of warning signs:
- unnaturally shiny, dense, stretched skin at the site of needle insertion;
- tension and the appearance of swelling (rapidly growing swelling is especially dangerous);
- change in the shade and temperature of the hand - redness, blueness, too cold skin;
- self-slowing or stopping the flow of medication;
- continuation of the infusion after applying a tourniquet to the vein;
- leakage of solution around the injection site;
- burning or discomfort in the area where the needle is located.
If such symptoms occur, stop the infusion immediately and remove the needle. The injection site must be carefully examined, and if a large amount of solution is injected past a vein (especially if it is viscous or caustic), you must immediately consult a doctor. To eliminate the consequences in such cases, the introduction of an antidote is required.
If the amount of the drug that gets into the tissue is small, you need to monitor the affected area for 2-3 days. At the first manifestations of necrosis, immediately contact a medical facility.
If a vein is damaged, it is necessary to press it for a few minutes, and then apply a dry sterile bandage; if a hematoma appears, apply a compress. If the patient's condition has not worsened, the IV can be reinserted into another vein.
Diagnosis of thrombosis
When visiting a medical facility, the doctor diagnoses the pathology and prescribes treatment. The main methods used to detect thrombosis are:
- coagulogram - blood test for clotting;
- magnetic resonance venography;
- duplex\triplex scanning of the veins of the upper extremities;
- ascending venography using a contrast agent;
- radionuclide scanning of the location of the thrombus;
- thromboelastography.
Ultrasonography
Ultrasound duplex scanning of veins is the “gold standard” for diagnosing thrombosis localized in the upper extremities. The technique allows you to quickly, highly informatively and non-invasively obtain information about the state of venous blood flow. The method is ideal for visualizing the veins of the extremities, neck, axillary and subclavian areas.
CT scan
Another popular method for diagnosing thrombosis. It is used mainly urgently, in case of suspected dangerous complication of deep vein thrombosis - pulmonary embolism. CT allows you to quickly assess the extent of the problem and select the most appropriate method of providing emergency medical care.
Where do they put an IV if the veins in the arms are bad?
If it is not possible to place a drip into a vein in the bend of the elbow, the nurse chooses another location. Inserting a needle into small vessels is strictly not recommended. It is extremely difficult to get into them, and problems subsequently arise much more often - hematomas and phlebitis are possible. The examination begins from the back of the hand, where the vessels are also quite large and well defined. A catheter is usually placed there - the bend of the elbow is not suitable for this purpose, since the device can be easily damaged when bending the arm.
Next, the veins of the forearm are examined, and a place is chosen as low as possible. The vessels that run along the outside of the forearm near the wrist are rarely used - they run close to nerves, so there is a high risk of damage. IVs are also practically not placed in the veins of the inner part of the arm below the elbow (the so-called antecubital fossa). When the solution gets into nearby tissues, compression of important anatomical structures occurs, which threatens damage to the veins and necrosis.
Droppers are placed in the veins of the legs extremely rarely - only when it is impossible to administer the drug in any other way. The vessels are more prone to inflammation and phlebitis, and the procedure is extremely painful - the skin on the lower extremities is rough, so it is much more difficult to pierce it. There are no large veins other than the central femoral ones, and the popliteal ones are inconvenient due to their location.
In the absence of other options, doctors choose the “veins of last resort” for infusions, that is, the central ones. These include:
- subclavian (under the right or left collarbone);
- internal jugular on the sides of the neck;
- femoral, which are located in the groin, are used extremely rarely due to the high risk of complications.
Such intravenous infusions are a minor surgical operation - first, catheterization is performed, after which medicinal solutions are administered. Catheterization is carried out under anesthesia and ultrasound control - some vessels are invisible to the eye, so it is impossible to determine without appropriate landmarks.
It is especially difficult to give IVs to newborns or infants. The veins in their arms are very thin, so not every experienced nurse can get into them. In addition, young children are unable to lie completely still for long periods of time, which increases the risk of injury. For such patients, IVs are often placed in the legs or veins in the head - such a procedure often shocks parents, but significantly reduces the risk of complications.
Carrying out the procedure on your own can lead to serious complications, so it is better to consult an experienced healthcare professional. To install an IV in Moscow at prices lower than in commercial clinics, you need to call a qualified nurse by calling the phone number on our website. An experienced specialist will perform the procedure quickly, painlessly and absolutely safely!
Treatment of thrombosis
If you suspect thrombosis, you should consult a doctor as soon as possible. The sooner you do this, the higher the likelihood that you will be able to avoid irreversible consequences of the pathology and a significant deterioration in the quality of life.
Depending on the condition of the affected vein, treatment can be carried out using several methods.
Conservative treatment
Involves the use of blood thinning medications. Anticoagulants are available in the form of tablets and injection solutions. The minimum duration of therapy is 3 months. In some cases, anticoagulants are indicated for many months or even years. The treatment period is determined by the doctor in each case individually, depending on the size and flotation of the blood clot, and the presence of concomitant diseases.
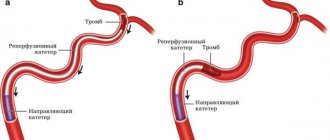
Minimally invasive techniques
If a mobile thrombus is detected in a patient’s vein, the patient is advised to undergo strict bed rest. In this case, implantation of a vena cava filter is necessary. The operation involves inserting a catheter with an umbrella-shaped device through the femoral vein to the affected area. When the conductor reaches the desired location, the filter is opened and the catheter is removed. The device is necessary to catch pieces of a blood clot if it migrates. In this way, it is possible to prevent deadly complications of thrombosis - pulmonary embolism, thrombophilia.
The operation is performed under local anesthesia and takes a maximum of an hour. The patient can go home the very next day after the intervention. Within a week after surgery, it is necessary to carry out X-ray monitoring of the position of the vena cava filter. The patient is also advised to undergo dynamic monitoring - every six months he needs to visit a doctor to assess the current state of the cardiovascular system.
Another way to solve the problem of thrombosis is stenting. It is used in case of a small blood clot. A special guide is inserted through the femoral access, with the help of which a metal stent is delivered to the damaged area. It expands, pressing the blood clot into the wall of the vessel and thus fixing it. The stent ensures normal patency of the vessel and eliminates the blood clot. The operation is performed under local anesthesia. The patient remains in the hospital for 24 hours after the intervention, after which he can go home. Stenting is one of the most modern methods of endovascular treatment of thrombosis and atherosclerosis.
Bibliography
- Mukhina S. A., Tarnovskaya I. I. Practical guide to the subject “Fundamentals of Nursing”: textbook. - M.: Rodnik, 2005.
- www.who.int World Health Organization Publications WHO WHO/GSBI: Injection Safety and Related Procedures Toolkit.
- Savelyev N. “Injections, IVs, dressings and other medical procedures and manipulations”: - M.: AST, 2021.
- Bikkulova D.Sh. Venous access protocols are a comprehensive solution to CVC problems. //Journal Polyclinic 1(2)/2014
- Briko N.I., Bikkulova D.Sh., Brusina E.B., et al., Prevention of catheter-associated bloodstream infections and care of the central venous catheter (CVC). //Clinical recommendations. — M.: “Remedium Privolzhye”, 2021