What is important to know about jugular vein thrombosis
- Inflammatory etiology is becoming less common
- Usually iatrogenic causes (insertion of a catheter, pacemaker, radiation therapy)
- Jugular vein thrombosis accounts for 5% of all thromboses
- Men and women get sick equally often
- The disease occurs in all age groups
- Acute, subacute or chronic occlusion of the internal jugular vein by a thrombus
- Three groups of reasons (Virchow’s triad):
— Endothelial defect (for example, due to prolonged catheterization or injection drug addiction).
- Slowing or stopping blood flow (for example, due to compression or invasion by a tumor).
- Blood clotting disorders (for example, caused by a tumor process).
Causes of thrombosis
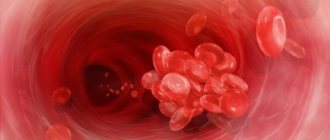
In order for a blood clot to form in a vein, a number of conditions or factors are necessary. In the classical version, there are three factors that contribute to thrombus formation (Virchow’s triad).
- hypercoagulable state (increased coagulability). There are many reasons for increased blood clotting - surgery on any part of the body, pregnancy, childbirth, diabetes, excess dietary fat, oral contraceptives, dehydration, genetic factors (rare), etc.
- injury to the inner wall of the vessel (endothelium). The vascular wall can be injured during the installation of a venous catheter, injection into a vein (due to this, thrombosis is very common in drug addicts who inject into the veins of the legs, in the groin), injuries, during radiation therapy, chemotherapy, etc.
- slowing down blood flow. It can be observed in various conditions - varicose veins, pregnancy, obesity, immobilization of a limb (for example, when wearing a cast after fractures), heart failure, forced sedentary position of the body (for example, during long air travel), compression of veins by tumors, etc.
Thrombosis can occur due to the action of one factor or a combination of them. For example, in case of a fracture of the leg bones, all three factors can be involved - increased coagulability in the case of extensive hemorrhages in the area of injury, damage to the vascular wall as a result of a mechanical shock, and a slowdown in blood flow as a result of wearing a cast.
Most often, thrombosis occurs in the veins of the lower extremities. This is due to the fact that stagnation most often occurs in these veins (obesity, varicose veins, edema, etc.).
Clinical manifestations
A typical picture of symptoms of jugular vein thrombosis:
— Random find:
- Swelling of the neck
- Located in the lateral sections of the neck, below the hyoid bone or in the supraclavicular region.
— Paraneoplastic syndrome (Trousseau syndrome).
— Compression or infiltration associated with the tumor process.
— Acute thrombophlebitis:
- Increased body temperature
- Soft, painless swelling (differential diagnosis with abscess)
- Gentle head position
- Rarely - fulminant sepsis.
— Chronic jugular vein thrombosis: Dense, sometimes painless swelling (differential diagnosis with a tumor).
Anatomical features
In order to better understand the mechanisms of occurrence and possible localization of pathology, one should turn to anatomy.
In the human body there are 3 main pairs of jugular veins susceptible to thrombosis:
- Internal . The largest among the listed vessels, responsible for the drainage of blood from the skull and normal metabolism in the brain. The venous line begins from the jugular foramen, descends to the area of the sternoclavicular junction, and merges with the subclavian artery. In medical practice, it is most often used for the purpose of catheterization for hemodialysis, plasmapheresis, and long-term infusion therapy.
- Outdoor _ In terms of its size, it ranks second among the vessels of this system and is responsible for draining blood saturated with carbon dioxide from the external parts of the cervical spine and head. It is located close enough to the surface that it can be seen and felt.
- Front . The pair is located under the chin and is part of the venous arch.
Each of these pairs is susceptible to thrombosis, but as statistics show, it is the outer vessel that most often clogs the thrombus.
Which method of diagnosing jugular vein thrombosis to choose: ultrasound, MRI, CT, angiography
Selection Methods
- CT, MRI.
Is MSCT of the jugular vein informative for thrombosis?
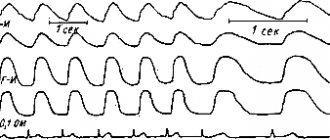
- In acute and subacute cases, there is usually an increase in the lumen of the jugular vein with a decrease in density in the center of the vessel (thrombus in the lumen of the vein)
- After intravenous administration of a contrast agent, the contrasted blood creates a ring around the thrombus
- With chronic progressive obliteration, complete occlusion of the vein occurs or blood outflow occurs through collateral vessels
- Strengthening of the vein wall indicates the presence of thrombophlebitis
- Possible abscess formation.
Is MRI effective for jugular vein thrombosis?
- Acute, subacute:
- Space-occupying formation with characteristic properties of the blood-thrombus signal
- Increased signal intensity around the thrombus on T2-weighted image.
— Chronic:
- Increased signal intensity in the vein on T1-weighted image
- Decrease in signal intensity on a T1-weighted image (disintegration of blood in a thrombus).
— MR angiography: Lack of signal from moving blood or filling defect in the lumen of the vein.
Sample normal values
- The normal diameter of the internal jugular vein is highly variable
- Right side: 12 mm (6 to 23 mm)
- Left side: 10.5 mm (5 to 19 mm).
Features
- Partially occlusive thrombus in the lumen of the internal jugular vein.
Drug treatment
The basis of therapy for the formation of blood clots in the circulatory system is the use of direct and indirect anticoagulant drugs. They are aimed at thinning the blood by reducing the level of fibrinogen, a substance whose concentration increases to form clots.
Direct anticoagulants include:
- Fibrinolysin,
- Fraxiparine,
- Heparin.
After a decrease in the prothrombin index, they switch to medications with an indirect anticoagulant effect, such as Curantil or Aspirin.
Another important aspect in complex therapy is the prescription of phlebotonics, whose action is aimed at improving metabolic processes and eliminating inflammation.
Remember! The dosage of any medications and the method of their use are prescribed exclusively by a competent medical professional.
If necessary, antispasmodics are prescribed to reduce the tone of the vascular walls and relieve pain. The addition of sepsis indicates the need for antibacterial therapy.
You can find out what varifort for varicose veins is and the opinion of Elena Malysheva from our article.
What diseases have symptoms similar to jugular vein thrombosis
Abscess
— Rarely tubular in shape
— Marked enhancement after administration of contrast agent
— May be adjacent to a vein or occur elsewhere
Tumor (with necrosis)
— Almost never has a tubular shape
— There is usually a lower signal intensity on T1-weighted image than that of the thrombus
— May be adjacent to a vein or occur elsewhere
Enlarged lymph nodes (inflammation or tumor)
— Usually multiple lesions or conglomerate
— Enhancement after contrast administration
— Located along the vein, the image of which is often normal.
Prevention
To prevent the development of pathology, you first need to be attentive to your own health and undergo regular medical examinations. If a person is at risk, it is necessary to systematically conduct a study such as coagulometry - a blood test for clotting. Thus, it is possible to promptly detect hypercoagulation leading to the formation of blood clots in the vascular system.
Particular attention should be paid to the choice of clothing. It should not hinder movement or squeeze the body. For everyday wear, preference should be given to loose items made from natural fabrics and of appropriate size. We described how to avoid varicose veins on the legs in our article.
Compliance with the drinking regime will prevent dehydration of the body and, as a result, thickening of the blood. Therefore, the minimum amount of clean water consumption should be 2 liters per day.
Giving up bad habits, adjusting your diet and diet, and daily moderate physical activity have a beneficial effect on the general condition of the body. Excluding fried and fatty foods from the menu reduces the chances of developing thrombosis, both of the superior jugular vein and similar pathologies everywhere.
We talked about whether an exercise bike will help with varicose veins here.
Principles of treatment of jugular vein thrombosis
- Broad-spectrum antibacterial agents (active against aerobes and anaerobes) for the treatment and prevention of infectious processes
- Anticoagulant therapy (heparin 30,000 units/day for 10 days)
- Resection or ligation of the vein is indicated in rare cases, since cases of pulmonary embolism from the head and neck vessels are very rare
- In most cases, spontaneous recovery occurs due to recanalization of the thrombus or outflow of blood through collateral vessels.
Surgical intervention
If conservative therapy does not bring the desired result, minimally invasive surgical procedures can be used to eliminate the blood clot. The frequency of surgical treatment for this disease is significantly inferior to classical therapy.
The most common methods are:
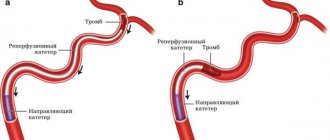
- Aspiration thrombectomy is the mechanical removal of thrombolytic mass through a puncture made through the skin.
- Endovascular thrombolysis is the delivery of a thrombolytic drug directly to the site of a vascular lesion by subcutaneous insertion of a special catheter. Thus, its patency is partially or completely restored.
Read about the manifestations and methods of treating varicocele on both sides in our material.
Possible complications and consequences
Jugular vein thrombosis has dangerous consequences:
- Sepsis
- Pulmonary embolism
- Papilledema
Jugular vein thrombosis. CT scan with contrast: complete occlusion of the left internal jugular vein by an old thrombus. The diameter of the vein is not changed in comparison with the opposite side. The lumen is not filled with contrast material and has a density slightly lower than the surrounding muscles. There is a noticeable increase in the lumen of the external jugular vein, which functions as a collateral vessel on the affected side.
CT with contrast, horizontal projection: fresh thrombosis of the right internal jugular vein (a). The diameter of the vein is increased in comparison with the opposite side, the thrombus has a density significantly lower than the surrounding muscles. A section taken at a slightly higher level (b) reveals a thin crescent-shaped ring around the thrombus.
Features of the disease and ICD classification
This disease is a pathological condition caused by blockage of the vessel cavity with a blood clot, which causes blood flow disturbances and, as a result, some organs and systems suffer. The lack of adequate therapy can cause the development of a number of rather dangerous complications, so it is extremely important to stop not only its manifestations, but also the cause itself.
It is impossible to unambiguously answer the question about the age category of patients suffering from this disease. Both young people and elderly people are susceptible to it, but in the latter the disease is somewhat more common. Doctors also note that gender may be a risk factor. Thus, among patients who come to medical institutions with a similar problem, the majority are men.
According to the international classification of diseases, created to systematize the statistical information obtained, this pathology has ICD 10 code I82.