What do drugs have in common?
To understand what the difference is and which drug is better - Rosuvastatin or Atorvastatin, it is necessary to conduct a comparative analysis. Both drugs under consideration are representatives of the new generation of statins. It is necessary to select one that, along with a noticeable therapeutic effect, has minimal side effects.
Their mechanism of action is approximately the same, but there are slight differences. If you understand the difference between them, you can adjust the treatment of a particular patient, which will significantly improve the prognosis for his recovery. The commonality between Rosuvastatin and Atorvastatin is that both drugs have a dual effect - they reduce the level of bad cholesterol and increase the content of good cholesterol.
Also common to these two drugs is that they:
- improve the condition of the inner lining of blood vessels during its dysfunction;
- improve blood flow through vessels;
- have a beneficial effect on the vascular wall.
Both drugs have common indications for use. Since they belong to the latest generation of statins, they can be prescribed not only for the treatment of diseases, but also for their prevention, which was difficult with the first and second generation statins due to the many side effects from them.
Therefore, the drugs in question are recommended for use in patients who have an increased risk of developing coronary heart disease. Factors that increase this risk include:
- age over 55 years;
- a history of diabetes mellitus;
- addiction to smoking;
- high blood pressure;
- hereditary predisposition to high cholesterol;
- reduced levels of high-density lipoproteins in the blood.
Atorvastatin and Rosuvastatin are not prescribed for the treatment of children and adolescents, during breastfeeding and pregnancy, or in the acute stage of liver disease. They are used with caution if the patient suffers from alcoholism, is predisposed to myopathy, or has a history of renal failure.
The maximum therapeutic effect from taking new generation statins is achieved after 4 weeks from the start of treatment. If the medicine is taken by a woman who has retained reproductive capabilities, then she is recommended to take care of reliable contraception along with statins.
Both drugs have minimal side effects and are therefore well tolerated by patients. They can be taken regardless of food intake and without reference to a specific time of day.
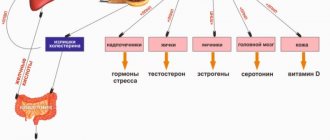
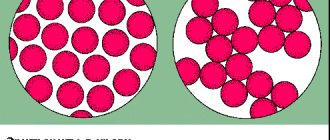
High levels of “bad” cholesterol lead to blockage of blood vessels
Arterial hypertension (AH) remains one of the most common pathologies in the population, contributing to the structure of disability and mortality from cardiovascular diseases (CVD) [18]. The course of hypertension is influenced by both external and internal factors. Hypertension is often associated with metabolic disorders: obesity, including abdominal obesity, impaired glucose tolerance, dyslipidemia, etc. [6]. According to the literature [13], dyslipidemia with increased levels of atherogenic lipid fractions is more common in hypertension.
A number of studies [11, 14] conducted in recent years have confirmed the prognostic value of arterial stiffness in different groups of patients. The spectrum of vascular disorders in hypertension is wider and includes non-atheromatous restructuring of the arteries, accompanied by a violation of their damping function with changes in left ventricular afterload and coronary perfusion. Currently, the concept of endothelial dysfunction (ED), which regulates the balance of processes such as maintaining vascular tone and permeability, hemostasis and local inflammation, including in hypertension, is being considered. Apparently, DE in combination with existing risk factors for the development of CVD contribute to its development and progression. In addition, a number of researchers [2, 7, 17, 28] believe that decreased endothelial function acts as a prognostic factor for unfavorable outcome in CVD. Cardiovascular complications (CVC) are not only the result of various interrelated processes called atherosclerosis, arteriosclerosis, DE, but also, as numerous studies have shown, the result of structural and functional restructuring of the heart, which can also worsen the prognosis of the underlying disease [4, 12, 15, 29].
Despite the fact that progress has now been made in studying the cardiovascular system in a number of pathological conditions, studies of these processes in women with dyslipidemia, suffering from hypertension at various periods of her “hormonal” life, are few in number and are extremely fragmented and often contradictory. At the same time, the study of these issues is of undoubted scientific and practical interest, as it allows us to develop recommendations aimed at improving the quality of examination of women with hypertension during the premenopausal period (PMP) in order to prevent cardiovascular complications in subsequent periods of a woman’s life - in menopause and postmenopause.
A decrease in estrogen levels in women in primary care leads to the development of metabolic disorders. Estrogens have a protective effect on lipid metabolism. Most authors point to the beneficial effect of estrogens on the content of cholesterol (C) and lipoproteins in the blood plasma - a decrease in the fraction of low-density lipoproteins (LDL) and an increase in high-density lipoproteins (HDL) (N.A. Gratsiansky, 1994; Walsh et al., 1991; Samsioe, 1993; Chow, 1995). Thanks to estrogens, the processes of cholesterol uptake and degradation in the vascular wall are inhibited (Hough, Zilversmit, 1986; Haarbo et al., 1991; Wagner et al., 1991; Clarkson et al., 1994). Due to estrogens, the production of very low density lipoproteins (VLDL) increases, which is accompanied by an increase in the level of triglycerides (TG) in the blood, and the LDL content decreases by increasing the number of liver receptors for LDL, which leads to increased catabolism. Estrogens inhibit the activity of hepatic triglyceride lipase, causing an increase in HDL levels due to a delay in their clearance [1, 23].
Antihypertensive therapy significantly reduces the risk of disease and death from cardiovascular complications [3, 9]. However, most studies concerning the problems of hypertension in middle-aged and older women cover mainly primary care [10, 16], paying much less attention to the premenopausal period. There is very little data that allows us to develop standards for the diagnosis and treatment of hypertension in women with dyslipidemia in this period. The information available in the literature on the course of hypertension in perimenopause and PMP is ambiguous regarding the relationship with the level of sex hormones in the blood and dyslipidemia, while there is a consensus on the increased manifestations of hypertension in women at this age.
Currently, the doctor has at his disposal a large number of pharmacological agents that, during long-term treatment, cause a decrease in blood pressure (BP), reverse development of left ventricular hypertrophy, and peripheral artery DE [20, 24]. It seems to us that it is justified to try in this situation to use mertenil and diroton, which affect the level of blood pressure, the process of remodeling of the vascular bed and left chambers of the heart, and DE.
Material and methods
The study included 52 women with stage II hypertension in primary care at the age of 45.0±3.5 years with changes in the rhythm and nature of menstruation, a decrease in estradiol levels (average 0.34±0. 04 pg/ml) and an increase in the level of follicle-stimulating hormone (FSH) in the blood serum (average 17.84±1.15 IU/ml). Lipid metabolism indicators were as follows: total cholesterol level - 5.43±1.50 mmol/l, LDL cholesterol - 4.1±1.8 mmol/l, HDL cholesterol - 1.31±1.60 mmol/l, TG - 1.71±1.50 mmol/l, atherogenic coefficient - 4.1±1.4.
The duration of hypertension disease averaged 4.8±2.2 years. The average level of systolic blood pressure (SBP) was 148±8 mm Hg, diastolic blood pressure (DBP) was 98±6 mm Hg. The study did not include patients with coronary heart disease, chronic heart failure, diabetes mellitus, or renovascular pathology.
The studied parameters were studied before treatment, during treatment and after 4-6 months of treatment. Additionally, the women kept diaries in which they recorded blood pressure and heart rate (HR) in the morning and evening.
The patients were divided into two groups. Patients of group 1 (n=22) received monotherapy with lisinopril (Diroton) at a dose of 10 mg for 6 months. Patients of group 2 (n=30) received combination therapy with lisinopril (Diroton) at a dose of 10 mg and rosuvastatin (Mertenil) at a dose of 10 mg/day for 4 months. A decrease in DBP by 10% or 10 mmHg was taken as a criterion for the effectiveness of antihypertensive therapy. and SBP by 15 mm Hg. from the initial level. The target blood pressure during therapy was considered to be less than 140/90 mmHg.
To assess the structural and functional state of the vascular bed before and after treatment, duplex scanning of the common carotid arteries (CAA) was performed using an Acuson 128 XP/10 device. When scanning the CCA, the intima-media thickness was measured at a distance of 1 cm proximal to the bifurcation along the posterior wall. Blood pressure on the brachial artery (BA) was measured twice according to the standard method; the average SBP and DBP and pulse pressure from two measurements were taken into account. In M-mode with synchronous ECG recording, the lumen of the CCA was measured in systole and diastole. For comparison between groups, a mean value equal to half the sum of the systolic and diastolic diameters was used. To assess the elasticity of the CCA, the elongation coefficient (CR) and the stiffness index (SI) were used. CR was calculated using the formula: CR = 2·ΔD/ΔPD/D{10-3 kPa}, where D is the diameter of the artery, ΔD is the change in artery diameter during the cardiac cycle, ΔPD is the change in pulse arterial pressure. IL was calculated using the formula: IL = log(SBP/DBP) / (ΔD /D), where D is the artery diameter, ΔD is the change in artery diameter during the cardiac cycle.
From the hemodynamic parameters of intravascular blood flow, the maximum systolic blood flow velocity (cm/s) and resistance index (units) were analyzed.
Statistical processing of data was carried out using the Statistica 6.0 program. Differences were considered statistically significant at p<0.05.
Results and discussion
In patients of both groups, a good antihypertensive effect was obtained after 2 weeks and was maintained for 6 months (Table 1).
A comparative analysis of the parameters of the structural and functional state of the vascular bed is presented in Table. 2.
In a comparative analysis of the diameter of the CCA after treatment, normalization of their average diameter was observed in group 2 (p <0.05). The speed of blood flow in the CCA in group 2 also turned out to be higher after treatment (p <0.05). The resistance index was lower in patients of group 2 who received combination therapy (p <0.001). The elastic properties of the carotid artery wall improved after treatment, the stiffness index decreased after treatment in patients of group 2 (p <0.001). Thus, the data obtained convincingly indicate the positive effect of combination therapy with diroton and mertenil on improving the elasticity of the CCA wall and reducing its stiffness in patients with hypertension with dyslipidemia in primary care hospitals with reduced estradiol levels.
Large arteries perform two main functions in the body: transport and damping. Changes in the vascular wall in hypertension lead to disruption of the damping function of blood vessels, contributing to an increase in pulse pressure and cardiac afterload [8]. The elasticity of the vascular wall is determined by the elastin fibers of the intercellular matrix, and the strength and rigidity are determined by collagen fibers [19, 21]. An increase in blood pressure during hypertension in women with dyslipidemia in a primary care setting with estrogen deficiency causes a change in their ratio with an increase in the total concentration in the vascular wall. As a result, it becomes stiffer and requires higher pressure than before to function properly. A cyclic process is completed, potentiating further progression of the disease. According to the Hagen-Poiseuille formula, a small increase in the radius of the vessel leads to a significant decrease in blood flow, which implies a decrease in the speed in it, and a small speed provides optimal conditions for the delivery of procoagulant factors to the interested area of the vascular wall and promotes the development of intermolecular interaction, aggregation and adhesion of formed elements and, thus, to the progression of atherosclerosis [12, 15, 22, 25]. In our study, we observed an expansion of the lumen of the CCA before treatment and a decrease in blood flow velocity in the carotid arteries associated with the expansion of the lumen of the vessel without hemodynamically significant stenoses, which indicates more pronounced structural and functional changes in the wall in the form of more pronounced arteriosclerosis. Under the influence of combination therapy, an improvement in the elasticity of the CCA wall and a decrease in its rigidity was observed.
According to modern data, DE occupies one of the most important places in the development and progression of CVD.
The endothelium provides regulation of vascular tone, the processes of hypertrophy and proliferation of smooth muscle cells, modulation of blood coagulation and fibrinolysis, as well as the process of inflammation. The main causes of endothelial damage are risk factors for the development of atherosclerosis: arterial hypertension, smoking and elevated levels of LDL in the blood plasma. It is known that modified LDL, subjected to slight oxidation, plays a critical role in the development of DE and the initiation of the atherosclerotic process. Modified LDL induces inflammatory cells to synthesize chemokines with subsequent stimulation of LDL peroxidation processes by activated monocytes and macrophages. Modified lipoproteins and cytokines reduce the formation of endothelial NO synthase. Fully oxidized LDL has pronounced pro-inflammatory and pro-atherogenic properties: they stimulate the synthesis of adhesion molecules, chemokines, growth factors, increase the proliferation of smooth muscle cells, collagen degradation and increase the coagulation capacity of the blood.
Damage to target organs, primarily the vascular bed with the development of arteriosclerosis, suggests a decrease in the vasomotor function of the endothelium in women with hypertension with dyslipidemia in PMP with hypoestrogenemia.
As can be seen from the data presented in table. 3,
When performing a test with post-occlusion reactive hyperemia, patients suffering from hypertension with dyslipidemia in the primary hospital are characterized by an increase in the increase in the diameter of the VA, more pronounced in group 2, in which the percentage of VA dilatation was higher after treatment (p <0.001). It should be noted that when conducting a test of reactive hyperemia against the background of a decrease in the vasomotor function of the VA endothelium, in 48.7% of cases an inertial type of vasomotor reaction was detected, which is characterized by the absence of a reaction within 2 minutes from the start of the test, which may indicate preclinical (initial) ) signs of atherosclerosis. After treatment with diroton, the inertial type of vasomotor reaction was detected only in 24.7% of cases in group 2 and in 31.3% in group 1.
In addition, when assessing the intraluminal diameters of elastic and muscular vessels, it was revealed that in patients the carotid artery was dilated relative to the size of the VA (p <0.001). It seems that arteries with a predominance of elastin structures are exposed to hemodynamic factors to a greater extent than arteries with smooth muscle and collagen fibers, and the identified direct correlation between the level of SBP and an increase in the diameter of the lumen of the carotid artery in patients with hypertension and hypoestrogenism (r = 0.56; p=0.001) may indicate that the leading place in the expansion of CCA as a sign of remodeling and preclinical atherosclerotic lesions of the vascular wall is occupied by the level of SBP, apparently due to a more pronounced variability of this indicator against the background of disturbed hormonal levels. The identified inverse correlation between the shear stress on the endothelium of the CCA and the thickness of the intima-media complex before treatment (r = –0.65; p = 0.001), as well as the diameter of the CCA (r = –0.57; p = 0.001) may indicate that that the expansion of the lumen reduces the shear stress on the endothelium, and this can, by influencing the mechanisms of nitric oxide production, stimulate the constriction of the muscle cells of the media, increasing the tone and thickness of the vascular wall. In addition, the patients had a low dilating response of the endothelium during the reactive hyperemia test, which was apparently associated with deeper organic changes in the smooth muscle cells of the vascular wall. This may be due to an increase in the mass of smooth muscle cells against the background of estrogen deficiency, which increases the degree of vasoconstriction in response to neurohormones, leads to an increase in peripheral vascular resistance and contributes to the stabilization and worsening of hypertension [28]. Thickening of the vascular wall, leukocyte infiltration, and mechanical damage due to excess blood pressure trigger the process of apoptosis of endothelial cells and predispose to the development and progression of atherosclerosis [4, 5, 11]. In addition, with a progressive decrease in the level of estradiol, the level of fibrinogen increases, which is characterized by an increase in blood viscosity, hypercoagulation, increased platelet aggregation and damage to erythrocytes [15], which also affects the condition of the vascular bed and contributes to the aggravation of atherosclerotic changes in the vascular wall.
Damage to target organs and, above all, their vascular bed with the development of arteriosclerosis, the manifestations of which we found in women with hypertension with dyslipidemia in the PMP, suggests a decrease in the vasomotor function of the endothelium in patients with hypertension with estrogen deficiency. According to modern data, one of the most important places in the development and progression of CVD is occupied by DE, which regulates the balance of processes such as maintaining the tone and structure of blood vessels, hemostasis, local inflammation and permeability of the vascular wall.
Angiotensin-converting enzyme inhibitors can improve endothelial function and inhibit atherogenesis. The clinical trial TREND (Trial on Reversing ENDotelial Dysfunction) confirmed the data of numerous experimental studies on the presence of endothelium-modulating and anti-atherosclerotic properties in this group of drugs. With DE, remodeling of the vascular wall is possible due to estrogen deficiency, which has a negative effect on the vascular wall. In addition, the endothelium of the vessel is constantly under pressure load and is damaged due to high blood pressure, and NO, which the endothelium secretes to expand the lumen of blood vessels, is not released in the required quantity, the stiffness of the vessel increases, elasticity is lost, vasodilation decreases, oxygen delivery decreases, and can develop ischemia.
One of the pleiotropic effects of statins is the improvement of endothelial function. It is known that the vasodilatory effect and prevention of pathological vasospasm under the influence of acetylcholine administration develop within 24 hours after taking a single dose of statins [26]. Vasodilation occurs due to increased production of nitric oxide due to increased expression of NO synthase. In addition, there is a decrease in the concentration of the vasoconstrictor factor endothelin-1. It has been established that in addition to an increase in NO concentration under the influence of statins, there is an improvement in the bioavailability of NO produced by the endothelium [27].
Thus, when examining women with hypertension and dyslipidemia in the primary care hospital, it is necessary to take into account blood lipid composition and disturbances in the status of sex hormones as independent risk factors for the progression of hypertension. Women with hypertension in primary care, dyslipidemia, and an imbalance of sex hormones should be allocated to a separate group of dispensary observation. The rapid progression of vascular wall remodeling with the development of arteriosclerosis and DE, characteristic of these patients, as well as the combination of such independent risk factors as high blood pressure, imbalance of sex hormones, which determine the transition of adaptive remodeling to maladaptive with the development of hemodynamic disorders and chronic heart failure, requires involvement in observation not only a cardiologist, but also a gynecologist-endocrinologist to determine the management tactics for patients in this category.
We noted an improvement in endothelial function and VA distensibility in both groups, more pronounced during combination therapy with diroton and mertenil. The data presented in the article are important for the practicing physician, as they allow one to predict the course of hypertension and changes in the structural and functional state of the vascular bed in this and the next periods of a woman’s life.
What is the difference
A comparison of the drugs Atorvastatin and Rosuvastatin revealed that, despite some similarities, they belong to statins of different generations. Rosuvastatin is the latest development, and Atorvastatin precedes it. The advantage of the latest generation is that the dosage of the drug can be reduced, since it is highly effective.
Lovastatin and its analogues
Unlike Atorvastatin, 90% of Rosuvastatin is excreted from the body through the digestive system, and 5% through urine. In addition, if we compare drugs with each other in terms of lowering low-density cholesterol, Atorvastatin is slightly inferior to Rosuvastatin.
The first reduces by a maximum of 54%, and the second by 63%. They also differ in their half-life. If for Atorvastatin this period of time takes from 15 to 30 hours, then for Rosuvastatin it takes 19 hours.
The newest generation drug has a higher bioavailability. This means that it is better absorbed by the body. But the difference between them is not so significant: Atorvastatin – 12% and Rosuvastatin – 20%.
What also makes these drugs different is the nature of their solubility. Thus, Rosuvastatin is a hydrophilic drug, and Atorvastatin is lipophilic. This means that Atorvastatin is fat soluble and Rosuvastatin is water soluble. If you have to make a choice between Atoris and Rosuvastatin, then you must keep in mind that Atoris is a type of Atorvastatin, so the similarities and differences will be approximately the same.
In terms of safety, both drugs under consideration are approximately the same. But, for example, in type 2 diabetes, preference should be given to Rosuvastatin, since it has less effect on carbohydrate metabolism.
If we compare these drugs by cost, then in general the price of Atorvastatin is significantly lower than the cost of Rosuvastatin. In this sense, the dosage of the drug and the number of tablets in the package are important. For example, 90 tablets of 20 mg of Atorvastatin will cost about 800 rubles, while for the same package of Rosuvastatin you will have to pay more than 1000 rubles.
Judging by the effectiveness of these drugs, practice shows that Rosuvastatin has a more pronounced effect compared to Atorvastatin. Their effectiveness is higher, and the potential for side effects is lower than that of first-generation statins, for example, Simvastatin.
Instructions for use
Statins should be taken orally with a sufficient amount of water. It is forbidden to chew the tablet because it is coated, which dissolves in the intestines. Before starting a therapeutic course of 3rd and 4th generation statins, the patient must adhere to an anti-cholesterol diet, and the diet must accompany the entire course of medication treatment.
The doctor individually selects the dosage and drug for each patient, based on the results of laboratory tests, as well as the individual tolerance of the body and concomitant chronic diseases. Dose adjustments, as well as replacement of the drug with another medicine, are carried out no earlier than two weeks from the date of administration.
Atorvastatin dosage regimens
The initial dosage for systemic atherosclerosis is Rosuvastatin - 5 mg, Atorvastatin - 10 mg. You need to take the medicine once a day.
Daily dosage for the treatment of hypercholesterolemia of various etiologies:
- for homozygous hypercholesterolemia, the dosage of Rosuvastatin is 20 mg, Atorvastatin is 40-80 mg;
- in patients with heterozygous hypercholesterolemia - 10-20 mg of Atorvastatin, divided into morning and evening doses.
Features of Atorvastatin
The drug Atorvastatin belongs to the category of third generation statins. The drug is available in various dosages - 10, 20, 40 and 80 mg. The pharmacy chain offers 2 types of this drug - Russian (Atorvastatin) and Israeli (Atorvastatin-Teva). The active ingredient in Atorvastatin is atorvastatin calcium trihydrate.
The drug reduces the concentration of low-density lipoproteins and simultaneously increases the content of high-density lipoproteins. Also effective for familial and homozygous hypercholesterolemia. The effectiveness of the medicine appears after 2 weeks of regular use. After just 30 days, the maximum effect of the anticholesterol drug is achieved, which persists throughout the entire duration of treatment.
Atorvastatin, like Rosuvastatin, belongs to a new generation of statins
Taking Atorvastatin must be combined with diet. According to the diet, the patient must exclude from the diet foods rich in animal fats, as well as dishes prepared by frying. You can take the tablets regardless of meal time. The dosage is selected individually by the attending physician based on the results of the lipid profile.
The initial dosage is 10 mg; subsequently, if necessary, it can be increased to 80 mg per day. Patients suffering from renal or liver failure take Atorvastatin at this initial dosage all the time. Indications for the use of Atorvastatin are the complex treatment of high levels of total cholesterol and LDL and increased levels of triglycerides.
The following side effects may occur while taking Atorvastatin:
- sleep disturbance;
- headache and dizziness;
- anemia or thrombocytopenia;
- dyspeptic disorders;
- arthritis and myalgia;
- allergy;
- swelling;
- baldness;
- increased sweating;
- sensitivity to light.
Atorvastatin is not prescribed for use in cases of increased activity of liver enzymes, renal failure, during pregnancy and lactation, in case of individual intolerance to the components of the drug, severe liver pathologies. The drug is also contraindicated in patients under 18 years of age.
The cost of the drug in pharmacies depends on the dosage and manufacturer and varies from 130 to 400 rubles. Its analogues are the drugs Atoris, Liprimar, Tulip.
Review of Atorvastatin and Rosuvastatin
Atorvastatin is a drug that has a hypocholesterolemic effect.
As it passes through the body, the inhibitor controls the functionality of enzyme molecules that regulate the synthesis of mevalonic acid. Mevalonate is a precursor to sterols, which are found in low-density lipoproteins. 3rd generation statin tablets are used in the treatment of high cholesterol. During the period of atherosclerotic manifestations, the use of the drug shows a positive effect on lipid metabolism, reducing the concentration of lipid fractions of LDL, VLDL and triglycerides, which are the basis for the formation of atherosclerotic tumors. When using the drug, the cholesterol index decreases, regardless of its etiology.
Properties of statins
The drug Rosuvastatin is prescribed when there is an increased concentration of LDL molecules in the blood plasma. The drug belongs to the group of fourth (last) generation statins, where the main active ingredient is rosuvastatin. The latest generation medications containing rosuvastatin are the safest for the body and also have a high therapeutic effect in the treatment of hypercholesterolemia.
Features of Rosuvastatin
Rosuvastatin is a lipid-lowering agent and is prescribed to normalize the level of triglycerides and phospholipids and lipoproteins in the blood. The main active ingredient is rosuvastatin. It is prescribed for the treatment and prevention of hypercholesterolemia, atherosclerosis and its complications, and vein thrombosis.
Rosuvastatin reduces high concentrations of low-density cholesterol, total cholesterol, triglycerides, and apoliprotein. At the same time, it helps to increase the level of high-density lipoproteins. While taking this drug, the atherogenicity index decreases. This effect indicates normalization of the lipid profile.
Indications for prescribing this drug are as follows:
- hereditary tendency to increase cholesterol;
- initial detection of high cholesterol levels in the blood;
- increased levels of triglycerides in the blood;
- prevention of complications of atherosclerosis, namely angina pectoris, hypertension, myocardial infarction and stroke in patients over 50 years of age.
Since Rosuvastatin is not metabolized in the liver, its effect on this organ is minimal. After 90% of the drug is excreted through the intestines with feces, the rest through the kidneys with urine. The drug is not prescribed to persons under 18 years of age, patients with lactose intolerance, women during pregnancy and breastfeeding.
It is contraindicated in patients at the acute stage of liver disease, patients with myopathy, and those with individual intolerance to the components of the drug. The combination of Rosuvastatin with Cyclosporine is unacceptable. During treatment with this statin, doctors recommend following an anti-cholesterol diet. When prescribing a drug in a dosage of more than 40 mg, the attending physician takes into account the absolute and relative indications for this.
Rosuvastatin lowers cholesterol levels better than all other similar drugs
Both drugs - Atorvastatin and Rosuvastatin - have good patient reviews. Since these medications have similar effects, they are interchangeable. But the choice of a particular one should be determined by the doctor in accordance with the diagnosis and individual characteristics.
Reviews
Oksana, 46 years old, Pyatigorsk: I took Atorvastatin to lower cholesterol. It reduces well, but I experienced side effects myself. After 3 months of regular use, almost all lipid profile indicators, except triglycerides, approached normal. Based on the results of the analysis, the doctor supplemented the treatment with Dibikor, and triglycerides also decreased. I was afraid for my liver, but in vain. Everything is fine there.
Ekaterina, 35 years old, Moscow: I can’t say that Atorvastatin is significantly different in effectiveness from previous drugs. My father was prescribed 60 mg per day; he has high cholesterol. He says that he does not notice any significant changes in his condition after the course of treatment. Cholesterol remains what it was. Apparently this is due to hereditary predisposition.
Kirill, 60 years old, Samara: With a diagnosis of coronary heart disease, the doctor prescribed statins to prevent complications. The choice fell on the drug Rosuvastatin. I don’t feel its influence on myself, but according to tests, cholesterol corresponds to the norm for a healthy person. Before starting to take Rosuvastatin, it was increased several times. I can confidently recommend this drug to others to reduce high cholesterol.
Interaction with other medications and analogues
Statins may not be compatible with all medications. Sometimes taking two medications together can cause severe side effects:
- When taken together with Cyclosporine, myopathy occurs. Myopathy also occurs when combined with antibacterial agents of the tetracycline, clarithromycin and erythromycin groups.
- A negative reaction of the body can occur when taking statins and Niacin.
If you take Digoxin and statins, the concentration of Digoxin and statins increases. It is not recommended to take statin tablets or grapefruit juice. The juice reduces the medicinal effect of the statin, but increases its negative impact on organs and systems in the body.- Parallel use of statin tablets and antacids, and magnesium, reduces the concentration of statin by 2 times. If you use these drugs at intervals of 2-3 hours, then the negative impact is reduced.
- When combining the use of tablets and protease inhibitors (HIV), then AUC0-24 increases significantly. For people infected with HIV, this technique is contraindicated and can have complex consequences.
Atorvastatin has 4 analogues, and Rosuvastatin has 12. Russian analogues “Atorvastatin-Teva”, “Atorvastatin SZ”, “Atorvastatin Canon” are distinguished by their low price and good quality. The cost of medicines is from 110 to 130 rubles.
The most effective analogues of Rosuvastatin:
- Rosucard is a Czech drug that effectively reduces cholesterol in a short therapeutic course.
Crestor is an American drug that is the original 4th generation statin drug. Crestor - passed all clinical and laboratory studies. The only drawback in it is the price of 850-1010 rubles.- Rozulip is a Hungarian medicine that is often prescribed for atherosclerosis for long-term use.
- The Hungarian drug Mertenil is prescribed to lower bad cholesterol and to prevent cardiac diseases.