What is subclavian artery stenosis?
23.10.2019
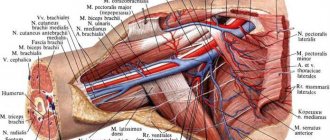
The clinical presentation of subclavian and innominate peripheral artery (SIPA) ranges from arm claudication to cerebral hypoperfusion to distal embolization and digital ischemia. PAAD of the upper extremity may present as lower extremity claudication in patients undergoing extraanatomic axillary or femoral bypass surgery.
Survey
Physical examination is significant for weak pulses on the ipsilateral limb, systolic blood pressure difference greater than 10 mmHg. Art. compared to the contralateral limb. Sometimes the affected hand may feel cool to the touch, and in severe cases digital ischemia has also been described. Often the disease is present during the sixth or seventh decades of patients' lives if they have associated risk factors for peripheral arterial , such as smoking, diabetes mellitus , hyperlipidemia, hypertension .
Subclavian artery stenosis causes notable morbidity because it causes symptomatic ischemic problems that affect the upper extremities, brain and heart . Atherosclerosis is the most common cause. Other etiologies include:
- arteritis;
- inflammation caused by radiation;
- compression syndromes;
- fibromuscular dysplasia ;
- neurofibromatosis.
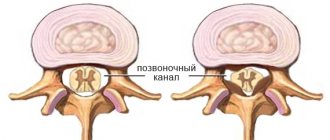
PAD of the great vessels is associated with narrowing of the arteries due to atherosclerosis . It is estimated that about 2% of the population has PAD of the subclavian artery . The prevalence in adults over 70 years of age is about 15%. Of these, almost 25% require revascularization. Most patients are asymptomatic due to the slow progression of the disease. Symptoms usually appear when there is 50% luminal narrowing of the vessel .
Prevalence
The prevalence of disease in the brachiocephalic artery in patients with PDPA is approximately 42%. About half of patients with this peripheral artery have left subclavian artery stenosis (30%). Half of patients with subclavian arterial disease have coronary artery , and a third have carotid or vertebral disease.
Risk factors
Vascular risk factors, including diabetes , hyperlipidemia, hypertension , and tobacco abuse, increase cell adhesion molecules, which promote the adherence of inflammatory cells to the arterial . This process causes remodeling of the arterial wall and lipid deposition through the tunica. the arterial lumen eventually narrows , which in turn causes calcification of the arterial .
In addition, the brachiocephalic arteries , including the innominate and subclavian arteries, can be affected by vasculitides such as Takayasu arteritis and giant cell arteritis. The disease of brachiocephalic atherosclerosis can be single-focal or multifocal. Brachiocephalic artery can present in several ways, including transient ischemic attack (TIA), upper limb ischemia or claudication, and vertebrobasilar insufficiency. Brachiocephalic artery aneurysms are uncommon and may be associated with atherosclerotic poststenotic dilatation, trauma, inflammation, or infection.
Symptoms
Upper extremity symptoms include arm lameness or muscle fatigue and finger necrosis. Neurological problems include vertebrobasilar hypoperfusion, visual , syncope, ataxia, vertigo facial sensory deficits .
In patients with internal mammary artery resulting from coronary artery bypass surgery symptoms of artery disease , including angina , caused by coronary-subclavian theft are predominant.
While diagnosis is usually based on imaging, a thorough physical examination is important. Upon examination you can show:
- unequal pressure on the hand;
- absent or significantly reduced impulses;
- neurological and cardiac complications;
- ulcers;
- gangrenous skin changes.
Initial diagnosis of patients with subclavian arterial disease involves measuring blood pressure in both arms to assess for upper extremity discrepancies and the presence of contusions (carotid, cervical, or supraclavicular). Less common physical findings include ulcers , necrosis, splinter hemorrhages, or gangrenous skin changes.
Published in Cardiology Premium Clinic
Atherosclerosis of the carotid arteries
What is atherosclerosis of the carotid arteries. One of the most common causes of arterial damage is atherosclerosis. Atherosclerosis is a systemic disease that results in the pathological deposition of cholesterol and fat on the inner wall of the artery, leading to the formation of plaque. Over time, the plaque grows, blocks the internal lumen of the artery and impedes blood flow as a result. Atherosclerosis affects all arteries supplying blood to the brain - vertebral and carotid; the aorta and arteries of the lower extremities, as well as arteries supplying internal organs - visceral and renal arteries.
Why is atherosclerosis dangerous?
Due to the narrowing of the carotid arteries, the blood supply to the brain sharply decreases and a stroke (acute cerebrovascular accident or cerebrovascular accident) can occur with a variety of motor and sensory disorders, including paralysis, and speech disorders. Sometimes a fragment or thrombus breaks off from the surface of an atherosclerotic plaque of the carotid artery, leading to the same consequences. In 70% of cases, a cerebral stroke develops without any warning signs, and in 40% of cases, a stroke leads to the death of a person. It is believed that after the artery lumen narrows by more than 60%, the likelihood of developing a stroke increases sharply.
Who may be at risk?
The following groups of patients are at greater risk of developing atherosclerosis of the carotid arteries:
- with high blood pressure
- with high blood cholesterol levels
- with diabetes
- obese
- smokers, etc.
Symptoms of arterial damage.
It is important to know! Damage to the carotid arteries often occurs without any complaints or symptoms!
Who should see a doctor and what tests should they undergo?
If there are predisposing factors in your life:
- age over 55 years,
- smoking,
- hypercholesterolemia (abnormal increase in blood cholesterol levels),
- hereditary predisposition (stroke or heart attack in relatives),
you need to undergo a special study - duplex scanning of the carotid arteries (brachiocephalic) and seek advice from a vascular surgeon.
Indications for surgical treatment.
Large - hemodynamically significant, i.e. disrupting the flow of blood through the carotid artery - atherosclerotic plaques are an indication for surgical treatment to prevent the development of stroke.
Possibilities of surgical treatment.
There are several types of surgical treatment:
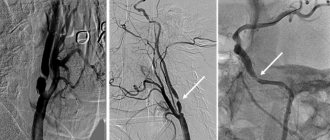
- open surgical removal of plaque from the lumen of the artery (carotid endarterectomy)
- endovascular treatment - placement of a stent into the lumen of the vessel.
The surgeon makes a decision on the volume and type of surgical treatment based on the results of the examination.
Possible consequences of the operation.
These operations are usually safe. The likelihood of complications developing is estimated at 1-2%. The most important thing is that in the future, repeated narrowings usually do not occur and strokes do not develop. History of a patient at MCSC.
A 70-year-old man contacted the MCSC. He previously suffered a stroke due to blockage of blood flow through the right internal carotid artery. As a result, my right arm and leg began to work poorly. With a diagnosis of atherosclerosis of the carotid arteries, he was admitted to the vascular surgery department of the Moscow Scientific Research Center.
MCSC specialists diagnosed atherosclerosis of the carotid arteries: atherosclerotic stenosis (narrowing to a minimum) of the left internal carotid artery by 90%, and performed carotid endarterectomy (direct removal of atherosclerotic plaque from the affected artery) in order to prevent stroke on the left. The patient was successfully operated on in our Center.
Rehabilitation was easy. On the fifth day, the patient was discharged and returned home without assistance.
Doctors at the vascular surgery department managed to improve the patient’s quality of life and prevent a second stroke.