Consultation with a dermatologist-venereologist – 1,750 rubles.
- Types of phlebitis
- Symptoms
- Diagnostics
- Treatment
Phlebitis is an inflammation of the vascular wall, namely the venous wall, with its gradual destruction. It occurs in both acute and chronic forms. The main danger of this disease is the development of a high risk of blood clots with subsequent blockage of blood vessels.
Provoking factors for the development of phlebitis most often are infections suffered by a person, acute inflammatory diseases, or the entry into the bloodstream of substances that cause irritation of the vessel wall.
What types of phlebitis are there?
There are several categories in the classification of phlebitis:
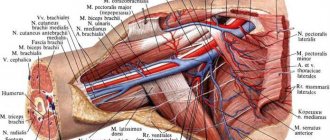
Depending on the location of the vein lesion, phlebitis is distinguished between superficial and deep . These two types are radically different in their symptoms and are easily differentiated.
In addition, phlebitis is divided depending on which vein wall is affected:
Endophlebitis is characterized by inflammatory changes in the inner wall of the vessel. The provoking factor is internal damage to the vein, such as during prolonged catheterization;
Periphlebitis - the lesion is predominantly localized on the outer wall of the vein. Occurs during the transition of the inflammatory process with a number of located organ tissues;
Panphlebitis is a common inflammation of all membranes.
Causes
For thrombophlebitis to occur, one or more of three factors must be present (the so-called Virchow triad):
- Damage to the vein wall (can be either mechanical, due to injury, or chemical - a burn from the administration of concentrated drugs, narcotic substances)
- Violation of the rheological properties of blood (increased coagulability, viscosity, etc.). This happens with dehydration, certain diseases, hormonal, and genetic disorders.
- Slowing of blood flow in the vein (when the vein is compressed, movement is limited (for example, when wearing a plaster cast)).
Under the influence of one or several factors, a blood clot forms in the lumen of the vessel and inflammation of its wall occurs. Example: with a serious leg injury, all three factors are present - mechanical damage (tears in the vein wall due to an impact), increased coagulability (due to blood loss), slowdown of blood flow (tissue swelling, plaster application).
Usually, with thrombophlebitis of the superficial veins, one vein is affected; inflammation can also spread to its tributaries. Migrating thrombophlebitis is known - with it, sequential inflammation of several veins occurs in different parts of the limbs. Such thrombophlebitis requires additional diagnostics to exclude oncological processes or genetic coagulation disorders.
Symptoms of phlebitis
As mentioned earlier, superficial and deep phlebitis have significant differences. Thus, with superficial phlebitis, local symptoms of inflammation come to the fore. At the site of the lesion, you can feel an area of tension, pain and compaction. The skin in this area becomes hyperemic, with a local increase in temperature. Sometimes this process is accompanied by a general deterioration in well-being, the development of weakness, and malaise.
In the case of deep phlebitis, the primary symptom is a significant increase in body temperature. Against this background, pain occurs in the affected area and pronounced swelling. The skin over this area does not turn red, but rather acquires a marble-white hue.
In severe inflammation, cerebral symptoms may occur in the form of headache, dizziness, and vomiting. An increase in blood pressure occurs. Without timely treatment, this disease can lead to liver or kidney failure.
What it is?
Phlebitis
is an inflammatory disease of the walls of venous vessels, which can occur in acute or chronic form. The acute form is characterized by severe pain in the affected veins, fever and general weakness. With chronic phlebitis, the disease is asymptomatic for a long time and appears only during exacerbations. Inflammation can occur in the veins of the legs, arms, and other parts of the body, but phlebitis of the lower extremities is most common. A serious complication of this disease can subsequently be thrombophlebitis (inflammation with the formation of a blood clot).
How to treat phlebitis?
First of all, the patient is provided with bed rest. The affected limb is fixed in an elevated position. Anticoagulants and anti-inflammatory drugs are prescribed. After relief of inflammation - physiotherapy.
Surgical treatment is carried out in case of complications, for example. thrombosis
To prevent the development of phlebitis, it is important to promptly treat infectious and inflammatory diseases, as well as follow the rules for performing intravenous injections.
Diagnostic methods
- Examination of affected veins by a specialist
- Blood tests
- Duplex/triplex angioscanning of the veins of the lower extremities
- Duplex/triplex angioscanning of arteries and veins of the upper extremities
- Ultrasound Dopplerography of veins (USDG).
Specialists to contact (depending on symptoms):
- Phlebologist consultation
- Cardiologist
- Surgeon
- Traumatologist-orthopedist
- Therapist
To establish a diagnosis and prescribe immediate treatment, we invite you to contact specialists from the Central Clinical Hospital of the Russian Academy of Sciences in Moscow.
Treatment
Phlebitis in most cases is subject to complex treatment using conservative methods. Outpatient treatment is possible, and if the disease is severe, the patient must be hospitalized. For certain indications, surgical intervention is prescribed.
Treatment includes:
- Drug therapy (painkillers, antiviral drugs, antibiotics, anti-inflammatory drugs, blood thinners, etc.)
- Physiotherapeutic procedures
- Wearing compression garments
- Prevention of disease.
Pathogenesis
The inflammatory process can be caused by various etiological factors, such as:
- infection;
- allergy;
- mechanical damage, etc.
The disease can also develop after a chemical burn to a vessel. In certain situations, phlebitis can be caused artificially. For example, during the treatment of varicose veins in phlebology, a technique called sclerotherapy is often used. The principle of operation of the procedure is based on the introduction of a special drug that causes aseptic phlebitis, which promotes subsequent gluing of the venous walls.
Confirmation of the diagnosis of thrombophlebitis
During the examination, the specialist individually selects the required minimum of research for each specific case. To confirm or exclude thrombophlebitis of the lower extremities, your doctor may choose one of the following diagnostic methods:
- Blood tests (clinical blood test, coagulogram, D-dimer);
- Venography (X-ray examination of the venous bed using the injection of a contrast agent that stains the vessels from the inside). Currently, due to the development of low-traumatic and highly informative research methods (primarily duplex angioscanning), it is used extremely rarely;
- Computed tomography and magnetic resonance imaging in vascular mode - performed in situations where ultrasound diagnostic methods are not very informative;
- Ultrasound diagnostic methods (Dopplerography and duplex angioscanning) are currently the “gold standard” for diagnosing thrombophlebitis.
After a diagnosis has been established, you may need additional diagnostics to identify the causes of thrombophlebitis, as well as control studies to clarify the nature of the dynamics of the pathological process.
Forecast
Life-threatening complications are rare. Pulmonary embolism is observed in only 2% of cases of subclavian thrombosis. Even with immediate intervention, some patients do not fully regain arm function and may have residual symptoms or require continued treatment. Severe venous insufficiency of the arm usually does not occur. Thrombosis of the subclavian vein does not pose a serious threat to life. After adequate treatment, the edema decreases significantly, but complete patency is rarely restored. If the causes for subclavian thrombosis persist, relapses of the disease may occur, so it is necessary to identify and eliminate them. As a reminder of the history of venous thrombosis, the patient is left with an increase in the volume of the shoulder and a network of visible saphenous veins in the area of the shoulder joint.
Consequences of the disease
If you ignore the need for treatment and do nothing, phlebitis can become thrombophlebitis. As a result, one of the formed blood clots can break off at any moment and block the blood flow, and this can lead to death. Previous phlebitis, in turn, can cause postthrombophlebitis disease.
The most common disease is among:
- athletes;
- people with varicose veins;
- smokers;
- drug addicts;
- people who are given medications over a long period of time using a venous catheter.
Diet
If you have phlebitis, you need to radically reconsider your eating habits and give up foods containing large amounts of salt, animal fats, preservatives and other chemical additives. It is advisable to eat often, but little by little. Prepare dishes using gentle methods: steamed, oven, grilled, or simply boiled in water. Diet for thrombophlebitis For thrombophlebitis, the diet should consist of the following food groups:
- fish, seafood;
- lean meat;
- cereals: buckwheat, rice, oatmeal;
- fresh vegetables, fruits, berries, herbs;
- dairy and fermented milk products;
- freshly squeezed juices, fruit drinks;
- dried fruits, seeds, nuts.
Medical Internet conferences
The goal is to study the problem of the development of post-injection complications in patients suffering from drug addiction: assessing the frequency of their occurrence in the structure of possible post-injection complications, assessing the effectiveness of their treatment.
The most common site of drug administration is the cubital region (58%), which is due to the accessibility for self-injections. Groin area - 13%, thigh - 13%, foot - 3%, lower leg - 3%. Noteworthy is the appearance of post-injection complications in drug addicts in the gluteal region (10%), which was previously extremely rare, because This pathology is usually associated with the administration of drugs for therapeutic or prophylactic purposes.
Among this group of patients, the most common complication is phlegmon (45%). Abscess - 27%, inflammatory infiltrate - 6%, artery thrombosis - 10%, phlebitis - 6%, gangrene - 6%. 75% of this group of patients were observed in the hospital only with a localized lesion, however, some patients developed more complex complications - sepsis (3%), severe sepsis (9%).
Note that the severity of a possible complication or course of the disease is also influenced by concomitant pathology. In addition to the fact that all patients in this group suffer from drug addiction, 49% have Hepatitis C, 11% have Hepatitis B, 6% have Hepatitis A, 6% have HIV infection and only 28% of patients have no concomitant diseases, which is a rather low figure given the age of the patients.
When treating post-injection complications in this group of patients, almost all patients underwent surgical intervention (96%). For 82% of them, only one intervention was sufficient - opening and drainage of abscesses. 7% of patients underwent necrectomy and opening of purulent leaks (more often in patients with gangrene).
Based on the results of treatment, conclusions were drawn regarding the length of hospital stay for patients with a similar pathology. A larger number of patients in the study group were discharged from the hospital within a few days, but some patients needed an extension of their hospital stay due to the severity of their condition. Of course, it is impossible to unify the length of stay in the hospital for patients with post-injection complications and drug addiction, because There are a number of features: age, concomitant diseases, severity of the condition, risk of developing sepsis, etc.
When studying the problem of treating post-injection complications in patients suffering from drug addiction, it was impossible not to turn to data on the mortality of such patients. Among the selected group of patients, mortality was only 6%, although this figure is quite high. It should be noted that mortality in this group of patients was recorded in patients suffering from severe sepsis, and among such patients it was 67%.
Prevention
The following rules of prevention will help prevent the development of phlebitis:
- adherence to the basics of a healthy lifestyle;
- quitting smoking and drinking alcohol;
- proper nutrition;
- body weight control;
- engaging in moderate physical activity with a sedentary lifestyle;
- normalization of work and rest regime
- hemostasiogram, DDimer, AT3 – blood test once a year.
If any suspicious symptoms appear, do not self-medicate, but seek professional help from a phlebologist as soon as possible. Only correct and adequate treatment will help stop the progression of inflammation and prevent serious complications.
Prevention of phlebitis during pregnancy
During pregnancy, every woman may experience phlebitis, especially if she was previously diagnosed with varicose veins of the lower extremities. During pregnancy, most drugs used to treat phlebitis are strictly contraindicated. Therefore, it is necessary to take all measures to help prevent such vascular disease. Throughout the entire period of bearing a baby, it is useful to follow these simple recommendations:
- take daily walks in the fresh air;
- regularly do exercises that have a general strengthening effect;
- control weight;
- Healthy food;
- If you have suspicious symptoms, consult a doctor rather than wait for the situation to resolve on its own.