The term “occlusion” in all areas of medicine (except for orthodontics, where it means closure) refers to the pathological condition of complete obstruction of any duct or vessel. The causes of such a catastrophe - and the speed of development and severity of the consequences are always, without exaggeration, catastrophic - can be different, but the most common cause of occlusion, at least vascular, is blockage by migrating atherosclerotic plaques, clots of coagulated blood, etc.
Both veins and arteries can become thrombosed, but in the case of the circulatory system of the eye, it is somewhat more common to encounter occlusion of the central retinal vein. The incidence of this pathology is relatively low - it amounts to tenths of a percent of the general population - fortunately, since any disturbances of the venous outflow (as well as the influx of saturated arterial blood), given the importance of the photosensitive retinal tissue in the visual system, are extremely dangerous and require immediate specialized assistance.
Table of contents:
What is central retinal vein thrombosis Causes of occurrence Main symptoms of the disease Stages of the disease Diagnosis of central retinal vein thrombosis Treatment methods Prevention of the disease
The formation of blood clots prevents blood circulation through the vessels. As a result, they become blocked, leading to the development of the disease. Treatment of central retinal vein thrombosis is possible with medication or surgery. The choice of thrombosis therapy technique depends largely on the degree of damage.
Hypertensive retinopathy
Hypertensive retinopathy reflects changes in the fundus of the eye due to arterial hypertension. Due to the high prevalence of hypertension (23% of the unselected world population), it is expected that the incidence of fundus pathology associated with this disease will also increase.
The main diagnostic method is ophthalmoscopy. Complications of hypertensive retinopathy may include recurrent hemophthalmos and retinal vein thrombosis.
Treatment takes place with the participation of a cardiologist and an ophthalmologist. It is mainly aimed at stabilizing hypertension and its consequences.
Reasons for appearance
Thrombosis occurs under the influence of other pathologies in the patient that negatively affect the vascular system of the organs of vision:
- atherosclerosis of arteries;
- hypertension;
- infectious viral and bacterial diseases;
- diabetes;
- sepsis;
- swelling of the optic nerve.
The disease can develop due to the patient's sedentary lifestyle, obesity, and endocrine disorders. Improper therapy for the listed diseases also leads to blockage of blood vessels.
Causes of occlusion of the central vein branch
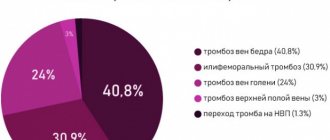
Risk factors for occlusion of the central vein can be both specific cardiovascular diseases (the undisputed “leaders” among which are atherosclerosis and hypertension, or arterial hypertension syndrome), and systemic endocrine disorders with the effect of damage to the vascular walls (primarily diabetes mellitus, which, in general, is associated with a lot of serious problems for the visual system). A typical scenario of the prethrombotic phase is mechanical compression of a vein by a neighboring artery, caused by organic degeneration of the arterial walls (hardening, thickening). Venous outflow becomes difficult and slows down, which can be diagnosed by ophthalmoscopy by specific changes in the color and shape of the vein (tortuosity, expansion, the presence of microhemorrhages, pallor and swelling of the surrounding area of the retina), thus creating conditions favorable for thrombus formation.
In general, venous stagnation, even before direct occlusion, leads to a number of serious organic changes: in particular, the permeability of the vascular walls increases, about (squeezing out, leaking) liquid fractions of blood into the surrounding tissues and spaces, due to which retinal edema and local capillary hemorrhages develop.
Main symptoms of the disease
Symptoms of thrombosis appear when a patient reaches a certain stage of pathological changes in the retina. The blockage is of a non-ischemic type, in which visual acuity remains at 0.1 diopters. Ischemic thrombosis is characterized by extensive hemorrhages.
The process of development of the disease can last up to several years, while the person’s vision remains normal. The main danger is that the patient does not attach importance to the initial signs of retinal disease. Incomplete thrombosis hardly manifests itself and does not cause concern.
Occasionally a person sees spots before his eyes. Patients experience symptoms in the evenings or mornings when looking at certain objects. Blind spots sometimes occur depending on the extent of the lesion.
Vision deteriorates: patients complain of blurred and blurred lines. Edema gradually develops, which is clearly visible during ophthalmoscopy. The vitreous body becomes covered with hemorrhages. They pass after a few months, but vision is not completely restored. Sometimes the back of the retina is damaged, but the patient does not lose vision.
Symptoms and clinical diagnosis
Patients with central thrombosis most often complain of sudden, painless unilateral vision loss. Such clinical signs are more typical for the ischemic occlusion scenario. Non-ischemic thrombosis has less pronounced symptoms and is manifested by unilateral clouding and blurred vision. Detecting occlusion of smaller branches is somewhat difficult because it can be asymptomatic. Sometimes there are sectoral opacities and blurred vision, with which patients are in no hurry to see a doctor.
The diagnostic process is based on a detailed study of the patient’s complaints and existing clinical symptoms. General clinical examinations such as general and biochemical blood tests, as well as a coagulogram are performed to determine the state of the blood coagulation system and the risks of recurrent thrombosis. The following instrumental methods are also used to make a diagnosis:
- Ophthalmoscopy to assess the condition of the vessels of the fundus and retina - allows you to see the expansion and blood filling of the venous segment, as well as subsequent swelling of the optic nerve head
- Fluorescein angiography - contrast helps to identify the level of occlusion and assess the functional state of blood vessels
- Optical coherence tomography – if necessary, is performed to visualize the central parts of the retina.
The diagnostic methods described above do not exclude the determination of visual acuity and boundaries.
Stages of the disease
There are several stages of retinal damage:
- Prethrombosis. The veins of the organs of vision are pathologically dilated. Vascular changes and macular edema are noticeable. At this stage, symptoms do not bother the patient. In rare cases, visual acuity decreases or objects appear blurry.
- Thrombosis. The retina is covered with multiple hemorrhages. The pathological focus can affect only one vein. The boundaries of the optic nerve are unclear, and swelling is noticeable around the macula. Possible loss of part of the visual field, decreased acuity.
- Retinopathy. After thrombosis, vision slowly recovers. Blood clots are visible at the bottom of the eye.
In some cases, recurrences of retinal vascular thrombosis are possible.
Forecast
In the absence of a pronounced and prolonged ischemic process against the background of vein thrombosis in the retina, the prognosis is favorable. If it is not possible to avoid ischemia, the likelihood of complications is high:
- neovascular glaucoma;
- recurrence of thrombosis and vitreous hemorrhage;
- traction retinal detachment.
All these pathologies lead to permanent vision loss, which even modern surgical interventions cannot correct. That is why you should not ignore the signs of partial venous obstruction in the retina: the earlier it is diagnosed, the higher the chance of avoiding vision loss.
Treatment methods
Thrombosis therapy begins immediately after diagnosis. The prescribed measures are aimed at resolving the resulting hemorrhages, reducing IOP, improving tissue nutrition and blood circulation.
Sometimes a positive result for the disease can be achieved with the help of drug therapy. The patient is prescribed eye drops that reduce pressure on the retina and accelerate the destruction of thrombotic formations. The use of B vitamins and ascorbic acid is indicated.
If traditional methods of treating the disease do not produce results, the ophthalmologist prescribes laser coagulation. Surgical intervention involves the impact of a laser device on a specific area of the shell.
Laser coagulation is good because it is bloodless, safe and does not require special preparation. The laser has coagulating properties, so it seals blood vessels and accelerates regeneration. After surgery, the rehabilitation period is significantly reduced.
The surgery takes place in a sitting position. The patient is seated on a chair and a drip of anesthesia is injected into the visual organs. With the help of drugs, the pupil is dilated to provide access to hard-to-reach areas of the retina.
A lens is installed on the patient's eye, thanks to which the light radiation will be focused. At this point, the patient may feel tingling or slight discomfort.
The surgeon controls the process of surgical intervention for the disease using a stereomicroscope. The laser beam seals certain areas and glues the membrane to the vascular fundus. Coagulation points keep the retina from further detachment.
Upon completion of the operation, the lens is removed. The patient should sit quietly for some time. At this time, ophthalmologists monitor the patient and monitor his condition. If there are no negative feelings, the patient goes home.
After surgery, you should not overstrain your visual organs. For a while you need to stop watching TV and working on the computer. If the operation was performed on one eye, the patient will not notice any special effects on vision.
Complete rehabilitation takes place in 2 weeks. During this period, it is important to avoid visiting the sauna, swimming pool, and heavy physical activity. It is not advisable to drink alcohol or antidepressants. Do not bend sharply. Since the operated eye is easily susceptible to infectious influences, it is important to promptly treat colds and viral diseases.
Complications after surgical treatment are rare. Sometimes repeated detachment occurs, in which case the operation is repeated. Possible inflammation of the conjunctiva or minor changes in vision.
Treatment of central retinal vein thrombosis
The main and mandatory condition for a favorable prognosis is the immediate initiation of responsive therapeutic measures when thrombosis begins, and even better - in the prethrombotic phase.
In addition to the above-mentioned Lucentis injections and laser coagulation, such measures may include the following prescriptions. Streptokinase and hemase in injections have a partial thrombolytic and good fibrinolytic (resolving hemorrhages) effect. Antihypertensive eye drops are used to stimulate retinal circulation.
Swelling is relieved with injectable dexamethasone and/or diprospan.
However, one of the most important tasks remains the cessation of neovascularization and the hemorrhages caused by it; here the first choice means are laser coagulation of the retina, injections of Lucentis or Ozurdex.
Disease prevention
Compliance with preventive measures will help prevent the development of thrombosis:
- Maintaining and maintaining a healthy lifestyle;
- reduce consumption of foods that increase blood pressure;
- playing sports;
- performing exercises to develop eye muscles;
- high-quality treatment of vascular diseases;
- timely examination by an ophthalmologist.
For the prevention and treatment of pathology, you can make an appointment with a doctor at the Santa Clinic in Chelyabinsk by calling. Operators will select a convenient time for a visit for the patient.
VENOUS THROMBOSIS IN OPHTHALMOLOGICAL PRACTICE
The classification, etiology, pathogenesis and outcomes of central vein thrombosis of the retina are considered. The importance of identifying ischemic thromboses is emphasized. The current therapeutical approaches are divided into laser and drug treatments. The significance and priority of timely laser treatment are shown in terms of outcomes.
I.A. Loskutov, Ph.D. honey. Sci. Department of Eye Microsurgery, Hospital named after. ON THE. Semashko, Moscow IALoskutov, MD, Candidate of Medical Sciences, Department of Eye Microsurgery, NASemashko Hospital, Moscow
P
The problem of thrombosis of the central retinal vein or its branches has been worrying the minds of ophthalmologists for a long time. Unfortunately, it should be stated that, despite the huge amount of research on the etiology, pathogenesis and treatment of such conditions, it is still not possible to reliably help the patient. Even on issues of terminology, there are still quite a lot of discrepancies. In this regard, it is appropriate to mention the statement of T. Williamson: “If confusion in terminology truly reflects confusion in understanding a specific issue, then the problem of central retinal vein occlusion is no exception” [1]. For the first time, under the name “retinal apoplexy,” a description of the clinical picture of thrombosis of the central retinal vein was given by Leibreich back in 1854. 20 years after this, Leber published a similar description of the condition of the fundus using a new term — “hemorrhagic retinitis.” Currently, the term “central retinal vein thrombosis” is practically generally accepted, which emphasizes the presence of an obstruction to the outflow of blood through the central vein of the retina. Although there are other definitions: “retinopathy of venous stasis” and “hemorrhagic retinopathy” according to S. Hayreh [2], “ischemic” and “non-ischemic” thrombosis of the central retinal vein according to Gass, “partial” or “incomplete” thrombosis and “threatening” thrombosis [3], primary and secondary retinal vein thrombosis according to R. Walsh [4].
Etiopathogenesis
The pathogenesis of retinal vein thrombosis was first addressed by Von Michel, who in 1878 published histological findings in two patients with retinal vein thrombosis. Retinal vein obstruction by thrombus was thought to occur after a significant slowdown in blood flow. At the beginning of this century, the famous pathologist Verhoeff argued against the presence of a blood clot in all cases of retinal vein occlusion. Thus, the researcher found a blood clot in only two cases out of 39 clinically diagnosed retinal vein occlusions. It is quite obvious that it was the issues of homeostasis that attracted special attention from researchers in order to identify possible risk factors for thrombosis. For example, resistance to activated protein C was found in 12% of patients with central retinal vein occlusions, although in the control group this figure was only 5%. This factor is of great importance in the processes of hemostasis [5]. Complex coagulological studies may well be useful in examining patients with retinal vein thrombosis, although the role of known indicators is not yet sufficient to predict the development of thrombosis [6]. Electrophysiological studies of the eyes, which are currently very widely used, have revealed typical changes in the electroretinogram in patients with retinal vein thrombosis. The particular significance of these studies is that the retinogram is a very sensitive test for ischemic damage to the retina. The most important change is a decrease in the amplitude of wave b or a decrease in the ratio between waves a and b. There are also many other deviations from normal retinogram data in patients with retinal vein thrombosis, the studies of which, unfortunately, are of little use in wide ophthalmological practice [7]. Obviously, for normal circulation of venous blood, its viscosity indicators are of great importance. It is logical to assume that there is a connection between an increase in the viscosity of venous blood and the occurrence of venous stasis, especially if we take into account the slower speed of blood flow in the venous bed in general. Studies have revealed a significant increase in blood viscosity for a number of indicators in patients with retinal vein thrombosis compared to the control group. One of them was a decrease in the ability of red blood cells to deform [5]. It should be borne in mind that the indicators of the study of blood viscosity in the systemic bloodstream may differ from those in the venous system of the eyeball and, quite possibly, in the direction of increasing their values. The role of the arterial system of the eye vessels in the pathogenesis and outcome of retinal vein thrombosis was first emphasized back in 1904 by the famous ophthalmologist Coats, who showed that the phenomenon of angiosclerosis of the retinal arterial vessels is by no means uncommon in patients with venous thrombosis in the fundus. In this regard, it is logical to assume a relationship between changes in the arterial wall and the ratio of blood flow between the venous and arterial systems in the eye [8]. One of the most active researchers on the topic of venous thrombosis in the eye, Hayreh, fully shares this position. He believes that the development of ischemic forms of retinal vein thrombosis is determined by the presence of occlusive lesions not only of the venous, but also of the arterial bed, and provides his evidence for the importance of assessing the arterial system. In experiments on monkeys, it turned out that occlusion of the central retinal vein and temporary blocking of blood flow through the central retinal artery at the point of their exit from the optic nerve head led to the development of a pattern similar to that of central retinal vein thrombosis in humans. Interestingly, occlusion of the retinal vein alone did not produce the typical pattern [9]. In another study, Hayreh suggests that a decrease in systemic blood pressure at night also plays a role in the pathogenesis of central retinal vein thrombosis [10]. The question of the influence of systemic factors on the development of thrombosis has not been completely resolved, but it is known that among the factors that significantly increase the risk of retinal venous thrombosis are arteriopathy, increased levels of glucose in the blood plasma and the level of systemic blood pressure. Regular physical exercise reduces the risk of thrombosis [11]. The connection between primary open-angle glaucoma and cases of central retinal vein thrombosis has been traced by a number of researchers. On average, thrombosis occurs in 4% of cases of primary open-angle glaucoma, and primary glaucoma or ophthalmic hypertension is found, according to various authors, in 4–43% of cases of central retinal vein thrombosis. Despite a short-term decrease in intraocular pressure immediately after the onset of central retinal vein thrombosis, in the long-term follow-up period an increase in the level of ophthalmotonus is noted compared to the control group [1,12]. The identification of cases of retinal vein thrombosis in young people suggested a search for the role of inflammatory reactions in the etiology of the disease. Studies and observations have not revealed clear evidence to confirm the inflammatory etiology of thrombosis, although interest in this problem clearly remains [13]. It is very important to separate thrombosis of the central retinal vein and thrombosis of the branches of the central retinal vein, if only because there are well-defined clinical differences between these pathological processes . Thus, the above-mentioned phenomenon of increased intraocular pressure in the long-term observation period is much less likely to be detected with thrombosis of a branch of the central vein. Signs of branch thrombosis were detected in only 1% of cases of primary open-angle glaucoma. Much more often, with thrombosis of the branches, hypermetropic refraction of the eye, the presence of high blood pressure and atherosclerotic vascular damage are detected [1].
Treatment problems
Laser treatment
When theoretically considering the problem of retinal vein thrombosis, it should be noted that, unlike, for example, arterial occlusions, the progression of ischemic damage is more extended over time, which is certainly important for treatment.
However, at present, the main effective means remains only photo- or laser coagulation to prevent the occurrence of areas of newly formed vessels. In 1995, the results of the Central Vein Occlusion Study (CVOS) Study, supported by the American National Eye Institute, were published. The purpose of the study was to compare the outcome of the natural history of the disease with the effectiveness of panretinal photocoagulation for ischemic injury and selective photocoagulation for the relief of macular edema. A series of patients (728 eyes) were left without treatment to determine the natural course of thrombosis. It turned out that in eyes with a significant spread of retinal hemorrhages that did not allow fluorescein angiography, in 83% of cases ischemic damage developed with the appearance of neovascularization of the iris, and if fluorescein angiography was possible, in 16% of cases ischemic areas were identified already during the study within 4 months The main conclusions of the study [14] were the following: • In all eyes after central retinal vein thrombosis, non-perfused areas of the retina should be looked for to identify patients at high risk of developing neovascularization, which manifests itself already in the first months after the onset of the disease. • If fluorescein angiography is not possible, the case should be treated as potentially ischemic. A special risk group consists of eyes with thrombosis less than 1 month old and with a decrease in visual function below 0.1. • When assessing the condition of the eye as insufficiently perfused, panretinal photocoagulation is necessary, the effectiveness of which is much higher if it is carried out before the first signs of neovascularization appear in the anterior segment of the eye. • It should be borne in mind that the appearance of newly formed vessels on the iris is possible after they appear in the angle of the anterior chamber, therefore, when monitoring the patient, gonioscopic studies are necessary. • After panretinal photocoagulation, observation continues with examination of the anterior chamber angle (to decide whether the treatment is sufficient). Drug treatment
The effectiveness of anticoagulants and fibrinolytic agents in this condition was much less than expected.
For example, the use of streptokinase significantly improves the outcome of the disease in terms of increasing visual functions, but the risk of its use turned out to be quite high in terms of the risk of hemorrhages in the vitreous body. The use of anticoagulants may be more effective if the presence of specific defects in the blood coagulation system is taken into account. For non-ischemic thrombosis of the central retinal vein, hemodilution may be an effective treatment method. An increase in circulating blood volume can apparently reduce blood viscosity and thereby increase perfusion. An improvement in the visual outcomes of thrombosis has been described with the use of a flavonoid drug, troxerutin [1, 15]. Outcome of central retinal vein thrombosis
The division of thrombosis into ischemic and non-ischemic is of fundamental importance when predicting the course of the disease. Thus, non-ischemic thrombosis of the central retinal vein has a generally good prognosis for visual functions [2], which cannot be said about the other form of the disease. Almost 70% of eyes with ischemic lesions have a final visual acuity below 0.05. In 21% of cases of central retinal vein thrombosis, neovascularization of the iris develops, which usually occurs after six months, although it can be detected even after 2 years from the onset of the disease. Neovascular glaucoma develops in 8% of all cases of central retinal vein thrombosis and in 67–82% of cases of ischemic central retinal vein thrombosis [16]. Thrombosis - the appearance of non-perfused zones - retinal ischemia - a stimulus for the formation of newly formed vessels - neovascularization in the area of outflow of intraocular fluid - impaired outflow of moisture from the anterior chamber of the eye - increased intraocular pressure - development of secondary neovascular glaucoma - irreversible loss of visual functions.
Literature
1. Williamson T. Central retinal vein occlusion: what is the story? Br J Ophthalmol 1997;81:698–704. 2. Hayreh S. So-called central retinal vein occlusion. Venous stasis retinopathy. Ophthalmologica 1976;172:14–37. 3. Gass J. Stereoscopic atlas of macular diseases. 4th Ed. Mosby 1997;546–55. 4. Walsh P, Goldberg R, Tox R, et al. Platelet coagulant activities in retinal vein thrombosis. Thromb Haemost 1977;38:399–406. 5. Williamson T, Rumley A, Lowe G. Blood viscosity, coagulation and activated protein C resistance in central retinal vein occlusion. Br J Ophthalmol 1996;80:203–8. 6. Loskutov I.A., Burgova N.S. Blood coagulation system in hemophthalmia and retinal vein thrombosis. Clinical issues of ophthalmology. Stavropol. – 1993. – P. 22. 7. Loskutov I, Shamshinova A. The role of electrophysiological investigations in the diagnosis of vascular pathology of the retina and optic nerve. 23d Symposium of international society for clinical electrophysiology. Athens., Greece 995; 131. 8. Williamson T, Baxter G, Lowe G. The influence of age, systemic blood pressure, smoking and blood viscosity on orbital blood velocities. Br J Ophthalmol 1995;79:17–22. 9. Hayreh S, Heuven W, Hayreh M. Experimental retinal vascular occlusion. Pathogenesis of central retinal vein occlusion. Arch Ophthalmol 1978;96:311–23. 10. Hayreh S, Zimmerman M, Podhajsky P et al. Nocturnal arterial hypotension and its role in optic nerve head and ocular ischemic disorders. Am J Ophthalmol 1994;117:603–24. 11. Glacet-Bernard A, Coscas G, Chabanel A, et al. Prognostic factors for retinal vein occlusion: prospective study of 175 cases. Ophthalmology 1996;103:551–60. 12. Rath E, Frank R, Shin D, et al. Risk factors for retinal vein occlusion. Ophthalmology 1992;99:509–14. 13. Fong A, Schatz H. Central retinal vein occlusion in young adults. Surv Ophthalmol. 1993;37:393–417. 14. Finkelstein D. Laser therapy for central retinal vein obstruction. Current Opinion in Ophthalmology 1996;7:80–3. 15. Glacet-Bernard A, Coscas G, Chabanel A, et al. A randomised, double-masked study on the treatment of retinal vein occlusion with troxerutin. Am J Ophthalmol 1994;118:421–9. 16. Quinlan P, Elman M, Bhatt A, et al. The natural course of retinal vein occlusion. Am J Ophthalmol 1990;110:118–23.