Hypertension is one of the most well-known pathologies of the cardiovascular system, and a disease such as arterial hypotension (hypotension) remains practically unattended. However, there are not much fewer hypotensive people among the population than people suffering from high blood pressure.
Arterial hypotension negatively affects the condition of the body's blood vessels, including the eyes. Due to the reduced level of pressure, hypotonic angiopathy may occur in the retina. To understand the process of its development, it is necessary to understand why pressure decreases and how this affects the body.
Major retinal diseases
- Retinal angiopathy;
- retinal detachment;
- retinal dystrophy;
- diabetic retinopathy;
- retinal tear;
- retinal degeneration;
- macular degeneration and macular degeneration;
- retinitis;
- hypertensive retinopathy;
- retinal tumor;
- retinal hemorrhage.
Retinal pathologies can occur with various general and systemic diseases - hypertension, diabetes mellitus, kidney and adrenal gland diseases, as well as with eye injuries and traumatic brain injuries. Some infectious diseases (flu, etc.) can be complicated by retinal diseases.
Main “risk groups”
- People with moderate and high degrees of myopia;
- pregnant women;
- elderly people with diabetes.
The initial stages of the disease may not be accompanied by any symptoms , so if you are at risk, be sure to undergo vision diagnostics using modern equipment. This examination will reliably determine whether you need treatment. If you are scheduled for surgery, do not put off surgery for too long. Before surgery, you need to protect your eye from possible damage in every possible way.
If diseases of the retina of a dystrophic nature are detected, with its thinning and rupture in the periphery, it is strengthened using a laser. Otherwise, any sufficiently strong tension can lead to detachment, requiring immediate surgical intervention. It is better to prevent such a situation. Moreover, detachment can occur when urgent provision of qualified ophthalmological care is impossible (at the dacha, on a trip, etc.)
Reasons for the development of the disease
Angiopathy develops against the background of vascular pathologies, so the reasons for the development of the disease are the risks that provoke vascular diseases:
- age from 30 years,
- smoking,
- alcoholism,
- pathological conditions of pregnancy,
- overweight,
- systematic intoxication (when working in toxic industries, during treatment),
- congenital disorders,
- diabetes,
- atherosclerosis,
- osteochondrosis and scoliosis,
- inflammation of the vascular wall,
- blood diseases and so on.
Inflammatory disease of the retina - retinitis
Retinitis is an inflammatory disease of the retina, which can be either unilateral or bilateral. This inflammatory disease of the retina can be either infectious or toxic-allergic in nature. Retinitis can occur due to a number of infectious diseases. For example, such as: AIDS, syphilis, viral and purulent infections, etc.
Symptoms of retinitis depend on the location of the process on the retina. But the main one is a decrease in visual acuity and a change in the field of vision. There are cases where retinal damage is initially limited to small areas, which then enlarge, leading to progressive loss of vision. Retinitis is treated with medication.
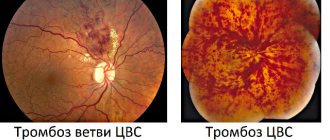
Retinal hemorrhage
Hemorrhages in the retina are more often related to vascular diseases and lead to decreased visual acuity, retinal detachment, secondary glaucoma, retinal dystrophy and other diseases.
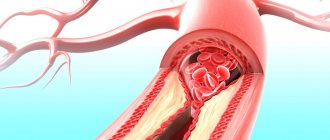
The causes of retinal hemorrhage may be associated with hardening of blood vessels in old age, due to thrombosis (blockage) of the central retinal vein or one of its branches. Also, retinal hemorrhage can be caused by diabetes, heart defects, blood diseases, skin burns, bruises, etc.
Professional diagnostics in the clinic
To diagnose retinal dystrophy, a complex of various methods is used in medicine. The most progressive of them is optical coherence tomography. It gives a more detailed and accurate picture of the condition of the retina tissue (compared, for example, with ultrasound), helps to detect changes in their structure and thickness, and areas affected by degeneration.
Optical coherence tomography is a painless and non-invasive examination method. It is carried out using rays of a certain spectrum, and depending on how they are reflected by the retina, a picture of its condition is drawn up. The study does not require special preparation and is absolutely safe for the patient.
Retinal detachment
Retinal detachment is the separation of the retina of the eye from the choroid. When the retina ruptures, the intraocular fluid penetrates under it and peels off from the choroid. If retinal detachment occurs, you should immediately consult a doctor, as delay may result in blindness.
Retinal detachment is usually treated surgically. This can be extrascleral ballooning or filling (the purpose of such treatment is to achieve adherence of the retina to the choroid), then laser coagulation and vitrectomy are performed (used to remove scars and blood from the vitreous). Surgical treatment methods usually require restriction of visual work and physical activity. Read more about the treatment of retinal detachment.
Retinal tumor
Retinal tumors are neoplasms of the retina that can be malignant or benign. Most often, tumors develop in childhood: in the first months of life in 20% of cases, in the first years in 55%. In 25% of patients, the process affects both eyes. The most common of retinal tumors are gliomas, which arise from the outer layer of the retina.
In the early stages, thickening of the retina occurs and this can only be determined by examining the fundus and ultrasound of the eye. After some time, the tumor takes up most of the eye. Due to the development of the tumor, the eyeball protrudes and its mobility is limited. Vision disappears.
The occurrence of the disease has a certain hereditary connection according to the incorrect dominant type.
Retinal tumors must be treated as soon as possible and in specialized ophthalmology departments of hospitals. If treatment is delayed, it can lead to irreversible consequences. Of the modern techniques for retinal tumors, the most effective are low-temperature (cryogenic) therapy and photocoagulation. Surgical treatment methods are organ-preserving.
Diagnosis of angiopathy
The disease is easy to detect with a standard fundus examination. During retinal imaging, you can identify:
- narrowing or dilation of arteries and veins,
- thickening of the vascular wall with the formation of pathological reflexes,
- tortuosity or straightening of the course of blood vessels,
- hemorrhages,
- areas of compression of arteries, veins, etc.
Important to remember! An annual examination by an ophthalmologist is mandatory if a person has hypertension, cardiac pathology, diabetes and atherosclerosis. In our clinic, it is possible to conduct not only examinations of the fundus of the eye with a description and conclusion of a specialist, but also to observe the dynamics of changes yourself using photographic recording of the condition of the retinal vessels (FundusFoto).
In some cases, additional examination is prescribed:
- Vascular ultrasound – determination of blood flow speed and the condition of the vascular walls;
- X-ray with the introduction of contrast - determination of vascular patency;
- MRI – assessment of the condition of eye tissues;
- visometry – determination of visual impairment;
- ophthalmoscopy - identification of the affected area of the retina;
- tonometry - determination of intraocular pressure.
The eyes are the only place on the human body where you can see blood vessels on the surface. This feature is successfully used in diagnostics. Based on the condition of the eye vessels, the following can be identified before the therapist:
- diabetes,
- hypertension,
- atherosclerosis,
- systemic diseases,
- pathology of the blood vessels of the head and neck,
- heart rhythm disturbance (in some cases).
Diagnosing retinal vascular angiopathy and monitoring its development can help in adequately assessing the course and success of treatment of the general disease. For example, the adequacy of the selection of antihypertensive therapy for hypertension is assessed by the degree of leveling of signs of hypertensive angiopathy.
Expert opinion
Klyuganov Vitaly Sergeevich
Qualified ophthalmologist
Work experience: 12 years
Retinal vascular angiopathy is not an independent disease, but only one of the manifestations of certain pathological conditions complicated by damage to the blood vessels of the retina or the entire body.
Based on the condition of the blood vessels, diabetes mellitus, hypertension, atherosclerosis, systemic diseases, vascular pathology of the head and neck, heart rhythm disturbances, etc. can be identified earlier than the therapist. An examination by an ophthalmologist is mandatory if a person has cardiac pathology, diabetes mellitus, hypertension and atherosclerosis.
It is not difficult for an experienced specialist to detect the disease. In the process of visualization of the retina, one can identify narrowing or expansion of arteries and veins, thickening of the vascular wall with the formation of pathological reflexes, tortuosity and straightening of the course of blood vessels, hemorrhages, areas of compression of veins, and much more. Taking into account the stage of angiopathy determined by the ophthalmologist, the therapist, endocrinologist, and cardiologist can assess the severity of the underlying disease.
Therefore, examination of the fundus with a wide pupil is mandatory during a full ophthalmological examination.
Retinal angiopathy during pregnancy
The causes of retinal angiopathy during pregnancy include:
- increase in blood volume in the body;
- presence of autoimmune diseases;
- development of gestational diabetes mellitus;
- chronically high or low blood pressure.
- gestational diabetes
- toxicosis
- bleeding disorder
Angiopathy in pregnant women most often goes away on its own and therefore does not require treatment. However, if the patient suffered from pathology before bearing the child, then the disease can progress and lead to complications: thrombosis, retinal detachment and hemorrhage. In severe cases, the disease can provoke termination of pregnancy.
When retinal angiopathy appears, treatment of concomitant diseases that provoked the development of pathology will be required. The woman is recommended to be monitored by a therapist and endocrinologist.
Most often, medications are prescribed that improve blood circulation and reduce the permeability of vascular walls. To normalize blood flow in the eyeball, special drops are used. In case of severe retinal angiopathy of both eyes, additional physiotherapeutic procedures may be prescribed.
Retinal angiopathy in a child
The development of angiopathy in a child is usually associated with the following factors:
- Increased intracranial pressure
- Deviation in the innervation of blood vessels, leading to a change in their tone
- Traumatic brain injuries
- Kidney diseases
- Diabetes mellitus type 1
- Autoimmune diseases
- Scoliosis
- Congenital malformations of the cardiovascular system
- Systemic pathologies of the hematopoietic organs
- Oxygen starvation of the fetus in late gestation or during labor
The disease in childhood can cause serious complications. Thus, retinal angiopathy in newborns often becomes chronic and leads to irreparable organic changes in the circulatory structure of the eye. With the development of pathology in a teenager (the so-called Eales disease), the vitreous body of the eye is replaced with fibrous tissue, which often provokes glaucoma and cataracts.
Treatment of the disease most often consists of prescribing medications that affect blood circulation and prevent platelets from sticking together. However, such treatment of retinal vascular angiopathy is prescribed only to children of preschool and school age. Newborns require regular monitoring by a doctor, since sometimes pathology occurs during a difficult birth and does not require additional therapy.
In case of severe angiopathy and its spread to both eyes, surgery may be performed to remove fibrous tissue.
Types of treatment
With angiopathy, the underlying disease must first be treated. Thus, for the treatment of retinal angiopathy of the hypertensive type, medications are prescribed to lower blood pressure; for diabetic angiopathy, diet and drugs that lower sugar levels are prescribed.
Treatment with medications
To eliminate the symptoms of angiopathy, relieve the disease and restore the ocular vessels, drug treatment is effectively used:
- Trental, Arbiflex improve blood circulation;
- Vitamins B, C, E and A, nicotinic acid normalize microcirculation;
- Calcium dobesilate, Xanthiol nicotinate, Ginkgo Biloba strengthen the walls of blood vessels;
- Cocarboxylase and ATP activate metabolism in tissues;
- Trombonet, Ticlodipine, Magnicor, Dipyridamole prevent the formation of blood clots.
Taking medication lasts about two weeks.
In case of stabilization of angiopathy, which is caused by an incurable or chronic disease, treatment is carried out every six months in courses of 2-3 weeks.
It is important to remember that treatment must be prescribed by a doctor. Self-administration of medications may do more harm than good.
Physiotherapy
In combination with other treatment methods, the following are used:
- acupuncture,
- magnetotherapy,
- laser irradiation.
Surgical intervention
To prevent vision loss at a late stage of the disease, laser coagulation of blood vessels is performed.
The operation takes 20 minutes and is performed under local anesthesia.
Retinal dystrophy
Retinal dystrophy is usually caused by disorders in the vascular system of the eye. It mainly affects older people, whose vision gradually deteriorates. Very often, degenerative changes in the retina accompany moderate and high degrees of myopia. The fact is that usually in this case the size of the eyeball is increased, and the retina lining its back surface is stretched, which leads to dystrophy.
Modern treatment of this condition, as well as other types of dystrophies (many inflammatory and vascular diseases of the retina lead to dystrophies), occurs using an argon laser. The main goal of this treatment is to strengthen and, in the case of retinal detachment, to postoperatively limit the retinal tear.
The principle of treatment is based on the fact that laser exposure leads to a sharp increase in temperature, which causes coagulation (clotting) of the tissue. Thanks to this, the operation is bloodless. The laser is very precise and is used to create fusions between the retina and uvea of the eye (i.e., strengthening the retina). Read more about laser coagulation of the retina.
Forecast and preventive measures
The prognosis for vasospasm is influenced by the nature of the attack. A short-term narrowing of the small branches of the central nervous system of the eyeball passes without a trace. Vasospastic reactions lasting 15 minutes or more, when irreversible changes in the retina occur, are considered unfavorable in terms of prognosis. Specific preventive measures are currently unknown. Nonspecific prevention consists of monitoring blood pressure and blood glucose levels, taking statins for atherosclerosis, and using personal protective equipment when working with pesticides in production conditions.
Age-related macular degeneration (AMD)
The most common cause of vision loss in people over 50 years of age. In VMD, the central part of the retina, the so-called macula macula, is affected.
The main risk factors for developing AMD are:
- age over 50 years;
- cardiovascular diseases (atherosclerosis, hypertension);
- genetic predisposition;
- gender (more common in women).
In the initial stages, the disease occurs unnoticed by the patient and can only be detected during an appointment with an ophthalmologist. With the progression of AMD and its transition to the so-called neovascular form, the patient may notice decreased vision, a feeling of curvature of lines, blurred and disappearing areas. If these symptoms occur, urgent consultation with a doctor is necessary.
Currently, the most effective treatment for AMD is the intravitreal (i.e. inside the eye) injection of drugs that block the growth of new vessels under the retina. These drugs can not only preserve, but also improve the vision of a patient with AMD. Treatment methods for AMD also include retinal laser photocoagulation and photodynamic therapy.
Diabetic retinopathy
In diabetes, the vessels of the retina are affected, which leads to a disruption in the supply of oxygen to the tissues and the development of diabetic retinopathy.
Diabetic retinopathy usually develops 5-10 years after the onset of diabetes. In type I diabetes mellitus (insulin-dependent), diabetic retonopathy proceeds rapidly and proliferative diabetic retinopathy . This form of the disease is characterized by the formation of new vessels that grow from the retina into the vitreous body and cause hemorrhages in it, and also enhance scarring processes in the vitreous body and can cause the development of retinal detachment.
In type II diabetes mellitus (insulin-dependent), changes mainly occur in the central zone of the retina. Diabetic maculopathy occurs , resulting in decreased central vision.
Another form of diabetic retinopathy is background retinopathy , in which pathological changes occur only in the retina of the eye. Due to disturbances in the area of the capillary vessels of the retina, small hemorrhages, deposits of metabolic products, and retinal edema occur. This form primarily affects older diabetics and eventually leads to gradual deterioration of vision.
Treatment methods for diabetic retinopathy:
- laser coagulation of the retina;
- intravitreal or intraocular injection of drugs that block the growth of new vessels under the retina;
- operation - vitrectomy.
How does hypotension develop?
The mechanism of development of the pathology is not fully understood. True, it is known that changes occur due to a failure of the autoregulatory system of blood pressure levels in the body. The result is an imbalance between the force of blood ejection from the heart muscle and the level of peripheral vascular resistance. The lower the pressure in the peripheral vessels, the lower the blood pressure numbers.
Not long ago, researchers found that along with substances that increase blood pressure (adrenaline, vasopressin, serotonin, etc.), the body also produces components that lower it (lactic and carbonic acids, taurine, prostaglandins, etc.). Their excess quantity also leads to the development of persistent hypotension.
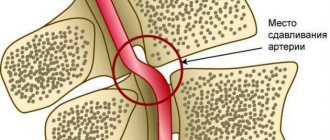
One of the main roles in the occurrence of hypotension belongs to disorders of neurohumoral self-regulation. The stability of blood pressure is maintained by the function of the carotid sinus, which exists in the branch of the aorta. Its innervation is carried out by the vagus nerve. This allows the sinus to quickly respond to any changes in pressure in the vessels and impulse “report” this to the vasomotor center of the brain to expand or narrow the vascular lumen.
If the irritation of the carotid sinus is insufficient, the brain does not receive commands to constrict blood vessels and blood pressure does not rise. Management of the function of the vasomotor center, in this case, passes to the parasympathetic nervous system and there is a persistent decrease in blood pressure throughout the body, including the eyes. A decrease in pressure in the vessels of the organ of vision often leads to the development of a hypotonic type of retinal angiopathy.
Retinal tear
Retinal tears most often occur in nearsighted people due to mechanical tension of the pathologically altered vitreous body. Patients note black threads in front of the affected eye, as well as light flashes. First, the edge of the tear in the retina begins to peel off, which later leads to retinal detachment.
To eliminate this, at the stage of holes or breaks, areas of the healthy retina are fixed using laser photocoagulation. Scarring occurs at retinal coagulation points. As a result, a strong connection between the retina and the choroid occurs. The coagulation technique involves applying 2-3 rows of coagulates around the hole or rupture.
What are PCRD and PVKHRD?
PCRD – peripheral chorioretinal dystrophy
This type of dystrophy directly affects the retina of the eye and its choroid (choroid). PCRD is considered a favorable type of dystrophy, since it does not carry any risks for the formation of a severe complication - retinal detachment. The most striking representative of the PCRD family is cobblestone dystrophy, which is harmless single or multiple foci of chorioretinal atrophy scattered along the periphery of the retina.
PVCRD – peripheral vitreochorioretinal dystrophy
In comparison with PCRD, PCRD is considered an unfavorable type of dystrophy, since in the pathological process, in addition to the retina and choroid, the vitreous body (lat. corpus vitreum), which is tightly fused to the area of chorioretinal dystrophy, is involved. It is believed that under conditions such as heavy lifting, sudden shaking of the body or head, childbirth, the vitreous body can provoke retinal rupture, thereby increasing the risk of retinal detachment. But, fortunately, in reality everything is not as scary as they used to think. Most PCVDs are harmless and simply require dynamic monitoring. There are types of PVCRD, the danger of which in most cases is greatly exaggerated. These include 2 types of dystrophies: lattice dystrophy (or “lattice”) and “snail track”. It is these two types of dystrophy that ophthalmologists constantly argue about.
"lattice" dystrophy
“snail track” dystrophy