What are platelets
Platelets are called nuclear-free blood cells that are synthesized by red bone marrow tissue. Their life cycle is about 7 days, after which they are utilized in the liver and spleen. In platelets, the aging process is more pronounced than in other blood cells.
Like other components of blood, platelets are divided into young, mature and old. In a healthy person, the number of mature cells should not exceed 95%. If the analysis reveals a large concentration of young cells, this indicates the development of certain diseases, including numerous damage to blood vessels and so on. In addition to young platelets, old platelets are often found in the blood plasma. This phenomenon indicates a disruption in the process of cell production and disposal.
Role in the body
Platelets take an active part in processes associated with the formation of blood clots. They also produce a special substance necessary for tissue regeneration, stimulation of cell division, regulation of the level of permeability of cell membranes and maintaining the elasticity of blood vessels.
The quantitative and qualitative composition of platelets is of valuable importance in the diagnosis of heart and vascular diseases. A high number of these bodies is called thrombocytosis, a low number is called thrombocytopenia.
Important! Depending on the age, the cells have different degrees of staining, which makes it possible to use this morphological feature for differential diagnosis.
What do the test results mean?
A blood test with the calculation of the leukocyte formula provides important information for doctors of various specialties about general and specific pathological changes in the functioning of the body:
- White blood cells increase in response to the development of infection, blood diseases, and autoimmune reactions. Leukocytes decrease in severe forms of disease, intoxication, some viral infections and toxic effects of drugs.
- Neutrophils begin to predominate in the leukocyte formula during infections of bacterial etiology, injuries, poisoning and after surgery or other tissue damage. The number of neutrophils decreases as a result of suppression of bone marrow activity due to drug-induced and autoimmune lesions.
- Lymphocytes increase as indicators of the activity of the cellular immune response during viral and some bacterial infections, lymphocytic leukemia. The number of lymphocytes decreases with long-term persistence of viruses (HIV, hepatitis, herpes viruses), and during the treatment of autoimmune diseases with corticosteroids.
- Monocytes increase during viral infections, long-term chronic inflammation, and some types of leukemia.
- Eosinophils are usually elevated in allergic diseases and parasitic infestations.
- Basophils increase in response to chronic inflammation, allergies and uremia.
The blood formula can change physiologically depending on the circadian rhythm, the nature of nutrition, changes in the temperature of the environment, and excitement.
What is the Fonio method?
Platelet count according to Fonio is an analysis that helps to identify the exact number of these cells in the blood and diagnose many diseases in a person. In this case, platelets are counted in a blood smear per thousand red blood cells, after which this number is recalculated in the ratio of 1 microliter or liter. The technique is considered very accurate and is used to diagnose many pathologies.
During the analysis, the blood is stained using the Romanovsky-Giemsa method
To carry out the analysis, blood is taken from a finger. The total number of platelets in a unit of blood is called a coagulogram. This type of study is prescribed to every patient, because the analysis helps to suspect and identify many diseases.
Detailed description of the study
Platelets are nuclear-free blood cells, blood platelets. They are formed in the red bone marrow and remain viable for 7-10 days. Platelets have properties such as adhesion (the ability to stick to the vascular wall) and aggregation (the ability to stick together). These properties ensure the implementation of the main functions of platelets: hemostatic and angiotrophic. Platelets also contain some active substances and coagulation factors, which, when activated, are released into the blood.
The hemostatic function of platelets is the secretion of vasoconstrictor substances, the formation of a platelet plug when the integrity of blood vessels is disrupted, and the acceleration of the formation of a fibrin clot.
The angiotrophic function is that platelets supply growth factors for the cells of the vascular wall, necessary for its restoration. Therefore, thrombocytopenia is often accompanied by the appearance of pinpoint hemorrhages in the skin or mucous membranes. In addition, platelets perform a protective function by “gluing” (agglutination) bacteria. Marked changes in the number of platelets in the blood can lead to various pathological processes: blood clotting disorders (thrombosis or bleeding), vascular fragility (the appearance of bruises and petechiae), and a decrease in the body’s protective properties. Sometimes counting platelets in a complete blood count can be difficult. This is observed with a pronounced tendency of platelets to aggregation, with certain diseases, as well as with exposure to toxic substances.
In such cases, platelet count according to Fonio is recommended. The advantage of this method is that the platelet count is calculated per thousand red blood cells in stained blood smears. Then the resulting amount is recalculated in proportion to a certain volume using a special formula.
Preparing for analysis
Several factors can affect the result of the Fonio platelet test. In this regard, it is necessary to properly prepare for donating blood. The patient should consider the following recommendations the day before collecting biological material:
- blood donation should be carried out 8 hours after the last meal, since many foods can affect the color index of blood cells;
- The day before the test you should not play sports. If a person has performed any physical activity, the test result may be inaccurate;
- material is collected in the morning;
- The most accurate information can be obtained by donating blood again. This helps to monitor platelet concentration over time.
In addition, the doctor should be sure to tell you whether you have taken any medications before. Many medications can also distort the results.
MEDICAL CENTER
Interpretation of study results contains information for the attending physician and is not a diagnosis.
The information in this section should not be used for self-diagnosis or self-treatment. The doctor makes an accurate diagnosis using both the results of this examination and the necessary information from other sources: medical history, results of other examinations, etc. Units of measurement at the STUDIO DOCTOR medical center: thousand/µl (103 cells/µl).
Alternate units: 109 cells/L.
Conversion factors: 109 cells/l = 103 cells/µl = thousand/µl.
Reference values:
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| Children | boys | girls |
| < 2 weeks | 218 — 419 | 144 — 449 |
| 2 weeks — 1 month | 248 — 586 | 279 — 571 |
| 1 — 2 | 229 — 562 | 331 — 597 |
| 2 — 6 | 244 — 529 | 247 — 580 |
| 6 months - 2 years | 206 — 445 | 214 — 459 |
| 2 years - 6 years | 202 — 403 | 189 — 394 |
| Age | Platelet concentration, thousand/µl (103 cells/µl) | |
| > 6 years | 150 — 400 | |
Interpretation of results
Increased values (thrombocytosis)
Functional (reactive) thrombocytosis:
- physical stress;
- inflammatory processes (systemic inflammatory diseases, osteomyelitis, tuberculosis);
- anemia due to blood loss, some types of hemolytic anemia;
- conditions after surgery;
- oncological diseases (not hemoblastosis);
- splenectomy;
- acute blood loss or hemolysis. Tumor thrombocytosis:
- myeloproliferative diseases, including erythremia, idiopathic hemorrhagic thrombocythemia.
Decreased values (thrombocytopenia)
Congenital thrombocytopenias:
- Wiskott-Aldrich syndrome;
- Chediak-Higashi syndrome;
- Fanconi syndrome;
- May-Hegglin anomaly;
- Bernard-Soulier syndrome (giant platelet syndrome). Acquired thrombocytopenia:
- idiopathic autoimmune thrombocytopenic purpura;
- drug-induced thrombocytopenia;
- systemic lupus erythematosus;
- thrombocytopenia associated with infection (viral and bacterial infections, rickettsiosis, malaria, toxoplasmosis);
- splenomegaly;
- aplastic anemia and myelophthisis (replacement of bone marrow with tumor cells or fibrous tissue);
- tumor metastases to the bone marrow;
- megaloblastic anemia;
- paroxysmal nocturnal hemoglobinuria;
- Fisher-Evans syndrome (autoimmune hemolytic anemia and thrombocytopenia);
- DIC syndrome (disseminated intravascular coagulation syndrome);
- massive blood transfusions, extracorporeal circulation;
- during the neonatal period (prematurity, hemolytic disease of the newborn, neonatal autoimmune thrombocytopenic purpura);
- congestive heart failure;
- renal vein thrombosis.
Medicines:
- anticancer drugs prescribed in sufficient doses that act on all patients (actinomycin D, asparaginase, azathioprine, bisulfan, chlorambucil, cisplatin, cyclophosphamide, cytarabine, dicarbazine, diunorubicin, doxorubicin, etoposide, mechlorethamine, mercaptopurine, methotrexate, nitrosourea, plicamycin, pro carbazine , thioguanine, vinblastine, vincristine - rarely);
- increased sensitivity of individuals to the effects of medications: certain analgesics (acetaminophen, antipyrine, aspirin, codeine, meperidine, formin, non-steroidal anti-inflammatory drugs (ibuprofen, indomethacin, naproxen, oxyphenbutazone, funacetin, phenylbutazone, paramethadione, phenytoin, trimethadione, valproic acid), antihistamines (chlorpheniramine, diphenhydramine), antimicrobials (p-aminosalicylic acid, amphotericin B, cephalosporins, chloramphenicol, clondamycin, clotrimazole, erythromycin, isoniazid, novobiocin, organic arsenic preparations, penicillin, pyrazinamide, rifampicin, stibophen, streptomycin, sulf Anilamides, tetracyclines , vancomycin), antithyroid drugs (methimazole, propylthiouracil, thiouracil), cardiovascular drugs (alprenolol, amiodarone, amrinone, captopril, digitoxin, mexiletine, nitroglycerin, oxyprenolol, quinidine, reserpine, tocainide), diuretics (acetazolamide, bumetanide, diazoxide, furosemide, mercury diuretics, thiazides, triamterene), metals (bismuth, mercury, gold compounds, silver), hypoglycemic drugs (carbutamide, chlorpropamide, glibenclamide, insulin, tolbutamide), psychotropic drugs (amitriptyline, desipramine, barbiturates, meprobamate, chlorpropazine, trifluoperazine ), other drugs (allopurinol, chloroquine, cimetidine, colchicine, cyclosporine, dextroamphetamine, dinitrophenol, ergot, estrogens, ganciclovir, heparin, hydroxychloroquine, alpha-interferon, levamisole, methyldopa, penicillamine, potassium iodide, prednisone, procaine, quinine, ranitidine, timoxifen, ticlopidine, vitamin K), alcohol.
Platelet count according to Fonio
When counting platelets, the laboratory technician uses several types of reagents. This is sodium ethylenediaminetetraacetate or magnesium sulfate. Reagents are taken using the SEE meter pipette.
The analysis is carried out in several stages:
- One of the reagents and blood are added to the test tube using a pipette. The amount of reagent is taken to the 75 mark, the blood volume to the K mark.
- The resulting mass is mixed well and used to make smears.
- If magnesium sulfate is used, the smear is stained using the Romanovsky-Giemsa method for 120 minutes and 45 minutes if the laboratory technician takes sodium ethylenediaminetetraacetate. In this case, the platelets turn purple-pink.
Platelet counts are performed through a microscope
Using a microscope, platelets and red blood cells are counted up to a thousand red blood cells. To find out the number of platelets, they are multiplied by the number of red blood cells in 1 microliter, and then the resulting figure is divided by a thousand. The specific color of the cells being studied helps to obtain the most reliable results. That is why many specialists use the Fonio platelet count method when making a diagnosis.
What exactly is determined during the analysis process?
cells (RBCs) are red blood cells. Not only their quantity matters, but also their size, shape and saturation with hemoglobin (Hb) , a protein that carries oxygen and ensures oxygen exchange in the body.
Hematocrit (Ht) is the proportion of red blood cells as a percentage of the total blood volume, a necessary indicator for diagnosing anemia.
MCV is the average erythrocyte volume, useful in diagnosing the causes of anemia.
MCH - the average hemoglobin content in one red blood cell will additionally indicate the presence of anemia.
MCHC - the degree of saturation of erythrocyte hemoglobin is relevant in the diagnosis of anemia associated with iron deficiency.
Relative red blood cell distribution width (RDW) is a measure of the distribution of red blood cells throughout the blood volume.
Platelets (PLT) , cytoplasmic fragments of megacryocytes involved in the formation of a blood clot to stop bleeding, are produced in the bone marrow every 7–10 days. If a low platelet count is obtained during an automated study, it is necessary to exclude the phenomenon of EDTA-induced thrombocytopenia - cell gluing into aggregates; for this purpose, microscopy of a blood smear is performed with counting the number of platelets and assessing the presence of aggregates.
White blood cells (WBC) are cells of the immune system, various in function, expressed in the leukocyte formula. With the normal version of the leukoformula, the percentages of different populations are not disturbed: neutrophils, monocytes, lymphocytes, basophils, eosinophils are in their reference values. The presence of atypical or immature forms of cells in the blood sample is necessarily reflected in the result form.
Advantages of the technique
The Fonio method of counting red blood cells has been successfully used by many doctors for many years. The technique has a number of advantages, including:
- when examining blood under a microscope, the laboratory technician clearly sees the material being examined, color, shape, number of cells;
- if necessary, analysis can be carried out at any time of the day;
- the method is easy to use, which is associated with a simple formula, but at the same time very informative.
Important! Despite the fact that medicine does not stand still and today there are new methods for counting blood particles, Fonio’s method is not inferior to them in its accuracy and information content.
What low scores may indicate
Thrombocytopenia or a reduced concentration of red blood cells in a person’s blood indicates the development of various undesirable conditions. The most common reasons for low performance include:
- radiation exposure of the patient;
- exposure to lead and other harmful substances on the body;
- pathologies of the hematopoietic system;
- collagenosis in a patient (a set of diseases affecting connective tissue);
- hereditary predisposition;
- chronic nephritis.
Patients with thrombocytopenia experience clinical manifestations such as frequent nosebleeds, bleeding gums, and subcutaneous hemorrhages. In women, the disease manifests itself in the form of heavy and prolonged periods.
Thrombocytopenia causes bleeding tendency
Treatment of this condition involves eliminating the underlying cause that led to the disorder. In this case, therapy with medication is used. In particularly severe cases, removal of the spleen or bone marrow transplantation is performed.
What you need to know about platelets and bruises
Falls and blows lead to bruises and abrasions. The body has powerful defenses in this case, stopping bleeding and resolving hematomas (bruises). The number of bruises is related to physical activity. Problems arise if there is a lack of coordination. Then even simple exercises and movements end in injury and hematoma.
The harder the blow, the bigger the bruise
If you cannot connect the blow and the appearance of a bruise, look at your shins, where the elastic of the socks ends. If there are small red spots that do not disappear with pressure, or bruises, this is a reason to be examined further.
The appearance of bruises, even with a minor injury, at the site of compression by an elastic band (from socks, panties, a belt, etc.) is called increased bleeding (hemorrhagic syndrome). Pay attention to complaints such as frequent nosebleeds, bleeding from the gums, and prolonged heavy menstruation in girls.
In mild cases, there is always an explanation: inflammation of the gums, hormonal imbalance, previous infection, and even stories that “in our family all the girls have heavy menstruation,” “and our dad also always has bruised legs,” etc. .
But not everything is so rosy. Severe hemorrhagic syndrome often ends in massive bleeding that threatens life. All of the above may be a manifestation of diseases combined into the group of thrombocytopathies - platelet pathologies.
What are platelets
Platelets are small platelets of blood produced in the bone marrow. Their purpose is to protect the walls of blood vessels in case of damage. Being able to stick to each other, platelets form a plug at the site of the wound and prevent blood from flowing out of the damaged vessels. In some congenital or acquired diseases, platelet production is reduced and thrombocytopenia (low number of platelets in the blood) develops; in some cases, platelets are born with defects, which is called thrombocytopathy.
The shape and properties of platelets suffer in many diseases: liver disease, scurvy (vitamin C deficiency), B12 deficiency anemia, hypothyroidism (thyroid deficiency), due to the action of drugs (aspirin and a group of non-steroidal anti-inflammatory drugs, some types of antibiotics and other).
What to look for in a blood test
A complete blood count is the first test that is done if defects and a decrease in platelets are suspected. Typically, venous blood is collected in a tube containing the anticoagulant EDTA (purple cap), which prevents the blood from clotting and allows cell counting.
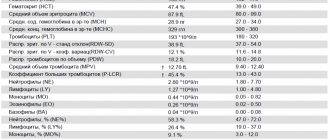
The automatic blood analyzer determines the following platelet parameters:
- Platelets, PLT - the number of platelets per unit volume.
- Mean platelet volume, MPV reflects the value of the mean platelet volume. A very important parameter in detecting thrombocytopathy (small, normal or large platelets).
- The indicator of platelet distribution by volume, PDW, reflects what percentage of platelets has a volume different from the bulk.
- Thrombocrit, PCT is an additional test that reflects the ratio of platelet volume to blood plasma, depending on their number and volume.
What is a “manual platelet count”?
Platelets behave harmfully not only in the body, but also in a test tube with venous blood. Because they know how to stick together and form small balls (conglomerates). This leads to false thrombocytopenia, the inability to detect defective platelets in an automatic analyzer, etc. Often, a general blood test must be repeated several times, blood must be collected in a test tube with a different filler, and a blood smear must be prepared and stained for “manual counting” and visual assessment of platelets under a microscope. This, like other specific tests for the properties of platelets, can be done in laboratories at hematology centers.
What to pay attention to:
- Presence of bleeding during teething/changing or extraction;
- Bleeding gums when brushing teeth;
- Presence of nosebleeds;
- Amount of menstruation in girls;
- Bleeding after surgical interventions (removal of adenoids, tonsils and others);
- The presence of similar symptoms in close relatives.
First tests for excessive bleeding
- Complete blood count with platelet count and determination of platelet indices
- Prothrombin index, prothrombin time, INR
In our Lab4U laboratory, tests can be taken at a discount of up to 50%, for example, a set of tests for increased bleeding.
In accordance with the “Federal clinical guidelines for the diagnosis and treatment of thrombocytopathies in children and adolescents.” Public organization National Society of Pediatric Hematologists and Oncologists; FSBI "FNKTs DGOI im. Dmitry Rogachev" of the Russian Ministry of Health. – Moscow, 2015.
Reasons for increased indicators
When the number of cells in question per unit of blood increases, we are talking about thrombocytosis. As a rule, this is a secondary pathology that occurs against the background of the following conditions:
- treatment with certain medications;
- previous surgery;
- splenectomy;
- heavy blood loss;
- inflammation of the lining of the brain;
- kidney and liver pathologies;
- development of oncological formations;
- Iron-deficiency anemia.
The greatest danger of thrombocytosis is the formation of blood clots that can clog arteries. This often leads to heart attacks, strokes and other dangerous diseases.
Cell norms in different population groups
When carrying out analysis using the Fonio method, a norm of 120 to 400 thousand cells per cubic millimeter of the material being studied is used. Fluctuation of boundaries depends on the patient’s age and gender. In women, men and children, deviations within these limits are considered normal.
Normal indicators:
- children under one year old - from 100 to 420 thousand per mm3;
- children from one year old - from 180 to 320 thousand per mm3;
- men - from 180 to 400 thousand per mm3;
- women from 180 to 340 thousand per mm3.
In adolescents, platelet levels can drop to 70 thousand per mm3. In men, the maximum number of these cells is observed at the age of 40 years. Such deviations must be taken into account when making a diagnosis and are explained by the physiological and age-related characteristics of the body.
What affects the level of platelets in the blood
The decrease or growth of the cells in question does not always indicate the development of any pathology. Sometimes the level of these cells fluctuates due to intense and regular physical activity and poor nutrition. Many people may find it strange that platelet levels increase when you lose blood. This is explained by the body’s attempt to compensate for blood loss by increased production of its formed elements.
Stress and bad habits can affect platelet levels in the blood
Rates are often elevated in people who drink alcohol for a long time. The normal platelet count is disrupted when taking medications with thrombocytopenic effects. Even a harmless nosebleed can affect the test results.
Methods for normalizing indicators
The first thing to do when detecting increased or decreased levels of platelets in the blood is to conduct a further examination of the patient in order to identify the pathology that led to this condition. The main method of treating thrombocytopenia and thrombocytosis is to combat the root cause. If the disorder develops for harmless reasons, you can increase the platelet count using the following methods:
- give up harmful foods, exclude alcoholic beverages, red grapes, green tea, blueberries, tomatoes from the diet;
- include apples, buckwheat porridge, fish dishes, bell peppers, and liver in your daily diet;
- special medications are taken as prescribed by a specialist;
- Vitamins A, B and C will help increase the number of cells.
Refusal from extreme sports, adequate assessment of stressful situations, and avoidance of conflicts at home and at work will help reduce the concentration of these blood elements.
To reduce platelets, experts recommend following the following rules:
- take acetylsalicylic acid as prescribed by your doctor;
- exclude from the diet rose hips, pomegranate, mango and other dishes that increase platelet levels;
- take magnesium supplements in courses several times a year;
- Drink at least one and a half liters of water per day.
Platelet counting using the Fonio method is one of the most accurate methods of blood testing. With the help of such an analysis, the doctor can find out many pathologies and select the appropriate treatment for the patient. This analysis is also carried out for preventive purposes, which is necessary for early diagnosis of diseases and preventing the development of serious consequences against their background.
Platelet aggregation
Platelet aggregation
— an indicator of disturbances in the vascular-platelet phase of hemostasis. A platelet aggregation test is performed to evaluate platelet function. The study allows you to diagnose and prevent the risk of developing bleeding and thrombophilia, evaluate the effectiveness of antiplatelet therapy and select the optimal dose of antiplatelet agents.
When vessels are damaged, platelets accumulate at the site of damage, are activated and stick to each other, forming a platelet thrombus, and a primary hemostatic plug is formed, which helps stop bleeding and heal the wound. When platelets are activated, a reaction occurs that culminates in the activation of phospholipase. As a result, the cell membrane changes properties and can come into contact with neighboring cells. As a result, platelets can aggregate with each other and form a platelet thrombus.
Aggregation
- the property of platelets to connect with each other.
Adhesion
is the ability of platelets to adhere to damaged vessel intima. Thus, adhesion and aggregation are processes necessary for the formation of a so-called “plug” to close the lesion in the vascular wall. Increased activation of platelets in pathology can lead to excessive thrombus formation and, conversely, when aggregation slows down, hemorrhages (bleeding) can occur.
Activation of platelets in
- a necessary element for normal hemostasis. Under normal conditions, circulating platelets do not interact with the inner surface and endothelial cells of blood vessels. But when the vessel wall is damaged, collagen comes out into the lumen of the vessel and platelets, with the participation of von Willebrand factor, adhere (adhesion) to the damaged area of the vessel.
Increased platelet aggregation is accompanied by coronary heart disease and the development of myocardial infarction.
Indications:
- to determine the causes of thrombosis during miscarriage and infertility;
- in case of unsuccessful IVF attempts;
- for cardiovascular diseases - heart attacks, strokes;
- while using oral contraceptives;
- during pregnancy planning and during pregnancy;
- to determine the causes of increased bleeding and predict the risk of bleeding;
- while taking antiplatelet drugs;
- to identify sensitivity or resistance to antiplatelet agents;
- for the diagnosis of acquired and congenital thrombocytopathies.
Preparation
No special preparation is required. It is recommended to take blood samples no earlier than 6–8 hours after your last meal. On the eve of the study, alcohol consumption, smoking, physical and emotional stress should be avoided.
If the patient is taking medications, you should consult with your doctor about the advisability of conducting a study while taking medications or the possibility of discontinuing it before the study; the duration of withdrawal is determined by the period of removal of the drug from the blood. Interpretation of results
Units of measurement: % As a percentage, the norm corresponds to 25–75%.
Factors that increase results:
- heparin;
- blood sample hemolysis;
- lipemia;
- nicotine.
Factors that reduce the result:
- excessive consumption of garlic (inhibits platelet aggregation);
- aspirin (acetylsalicylic acid inhibits platelet aggregation by blocking the synthesis of thromboxane A2);
- azlocidine, captopril, carbamate, carbencillin, chloroquine, chlorpromazine, clofibrate, cyproheptadine, dextran, dipyridamole, diuretics, flumenic acid, hydroxychlorin, isosorbide dinitrate, mezlocillin, moxalactam, nifedipine, nitrofurantoin, penicillin, phentolamine, piperacillin, prometh azine, propranolol, prostaglandin E1 , pyrindole, sulfinpyrazone, ticarcillin, tricyclic antidepressants;
- thrombocytopenia.
Deviations from the norm Abnormal platelet aggregation is combined with the following conditions:
- platelet disorders caused by deficiency of membrane glycoprotein receptors, deficiency of storage sites, deficiency of ADP release;
- lack of plasma proteins that ensure the interaction of platelets with the walls of blood vessels, including von Willebrand factor, fibrinogen, fibronectin;
- the presence of abnormal metabolites and plasma components in uremia, dysproteinemia, disseminated intravascular coagulation syndrome;
- collagen-vascular disorders (Marfan syndrome, osteogenesis imperfecta);
- myeloproliferative disorders (essential thrombocythemia, polycythemia vera, chronic myeloid leukemia);
- Glanzmann's thrombasthenia (Glanzmann): deficiency of glycoprotein IIb/IIIa, lack of aggregation under the action of ADP, collagen, adrenaline, thrombin, but normal aggregation under the action of ristomycin;
- Bernard-Soulier syndrome (Bernard-Soulier): Ib deficiency; normal aggregation under the influence of ADP, collagen, adrenaline; insufficient agglutination under the influence of ristocetin. Unlike von Willebrand's disease, agglutination due to the action of ristomycin is not corrected by the addition of normal plasma;
- deficiency of storage spaces/pools (Chediak-Higashi syndrome, glycogenosis type I, gray platelet syndrome, Hermansky-Pudlak syndrome, TAR thrombocytopenia syndrome - Thrombocytopenia/pathia with Aplasia of the Radius. This syndrome belongs to the group of congenital pathology of the megakaryocyte-platelet apparatus, combined with abnormalities of the skeletal apparatus - bilateral absence of the radius with shortening of the forearms, sometimes with deformation of the spine, scapulae, hip dysplasia, cleft palate, muscle defects, strabismus, pulmonary hypoplasia, congenital heart defects), Wiskott-Aldrich syndrome: platelet aggregation may be abnormal , often due to the absence or reduction of secondary ADP release;
- cyclooxygenase deficiency: abnormal platelet aggregation due to failure to activate the prostaglandin pathway; aspirin-like defect;
- von Willebrand disease: normal aggregation under the influence of ADP, collagen, adrenaline; absence or reduction of agglutination under the influence of ristocetin (with the exception of type IIB, where agglutination occurs at subnormal concentrations of ristocetin).
Decreased platelet aggregation
- taking acetylsalicylic acid, indomethacin, large doses of furosemide.