Decoding the results is the competence of a pediatrician, therapist or specialist, since it is important not only to analyze the numbers, but also to compare deviations from the norms of different indicators, to compare the information obtained during examination and history taking. To have an overview and be prepared when you see your doctor, learn what blood elements are tested in the laboratory, how to interpret the results, and what abnormalities may mean.
What indicators does the blood test contain?
Donating blood for testing is necessary during planned hospitalization, to assess the effectiveness of the therapy, and during pregnancy. To make an accurate diagnosis and prescribe treatment, the doctor always prescribes a general blood test. Material for research is taken from a finger or from a vein. The second option is preferable, since venous blood more accurately shows the level of hemoglobin and red blood cells.
First of all, red blood cells, white blood cells and platelets are analyzed, as well as:
- Hemoglobin level.
- Erythrocyte indices.
- Hematocrit level.
- Reticulocyte count.
Additionally, the erythrocyte sedimentation rate (ESR), color and blood clotting period are determined.
An extended study involves indicating the leukocyte formula, including the count of eosinophils, lymphocytes, monocytes, band and segmented neutrophils.
How to decipher test results?
A general idea of the number, size and shape of the constituent elements of blood (erythrocytes, platelets, lymphocytes, leukocytes) is given by a clinical blood test. Decoding its results can tell a doctor a lot about the condition of his patient’s body. For each indicator there is a range of reference (normal) values. These norms depend on gender and age. Thus, blood test standards in adults and children can differ significantly. As a rule, modern laboratories indicate reference values in the results form that the client receives. However, deviations from the norm of certain indicators do not yet indicate the presence of pathological conditions. The results of blood tests can be influenced by severe physical activity on the eve of blood sampling, and in women, also by the phase of the menstrual cycle. It is known, for example, that the day before the start of menstruation, the level of leukocytes can rise almost 2 times, so the normal values will differ from the standard ones. Therefore, it is better to contact a specialist for interpretation.
But what to do when it is important to get at least a general idea of the state of your body before going to the doctor? In this case, you can use the “online analysis interpretation” service, where you can enter the indicators of your analysis online and receive a preliminary conclusion. It is important to do this on the website of the exact laboratory where the tests were taken, because different units of measurement for blood parameters may be used. If the tests were taken in a laboratory whose website does not have such a service, then at your service is a calculator for converting units of measurement and a table for deciphering the main indicators of a general blood test. It contains blood test indicators that are considered reference values for middle-aged men and women. The interpretation of blood tests in children varies depending on age. The younger the child, the more his normal blood counts will differ from those of an adult. Thus, the number of leukocytes in the first days of a child’s life can be 2-3 times higher than the concentration of these cells in the blood of an adult. And this will not be a deviation from the norm.
Interpretation and normal values of the main blood test parameters
| How is it designated? | What does it mean | Norm for women | Norm for men |
| R.B.C. | Red blood cells | 3,5-4,5 | 4,0-5,5 |
| WBC | Leukocytes | 4-9 | |
| PLT | Platelets | 180-320 | |
| HGB | Hemoglobin | 120-140 | 130-170 |
| MCV | Average erythrocyte volume | 82-98 | 81-95 |
| MCH | Average HGB level in erythrocyte | 26-32 | |
| MCHC | Average concentration of red blood cells in HGB (%) | 31-38 | |
| HCT | Hematocrit (in%) | 35-44 | 40-50 |
| RET | Reticulocytes (%) | 0,2-1 | |
| ESR | ESR (mm/h) | 2-15 | 1-10 |
| CPU | Color | 0,85-1,05 | |
What deviations in the UAC may mean
For diagnosis, both a current blood test and previous studies are important to track changes. Let's consider what deviations in indicators can mean:
- Red blood cells. Exceeding the value is accompanied by insufficient oxygen supply, dehydration, acquired heart disease, and impaired adrenal function. The level may be lower than normal due to blood loss, iron deficiency anemia, in the second half of pregnancy, and with chronic infectious diseases.
- Leukocytes. Leukocytosis (exceeding the norm) can be caused by physiological characteristics or pathology. In the first case, the causes are: pregnancy, intense physical/psycho-emotional overload, hypothermia/overheating. Inflammatory and oncological diseases, poisoning and allergic reactions are manifested by pathological leukocytosis. With leukemia, bone marrow hypoplasia, liver damage, measles, lymphogranulomatosis, autoimmune diseases, a decrease in leukocytes will be detected.
- Platelets. The amount decreases with leukemia, AIDS, poisoning, bone marrow damage, prolonged therapy with hormones or antibiotics. The indicator goes beyond the normal range with inflammation of the rectal mucosa, osteomyelitis, joint diseases, cancerous lesions, and in the postoperative period.
- Hemoglobin level. Exceeding the norm occurs against the background of an increased platelet count, impaired blood clotting function, after a gastrointestinal disorder, or with an overdose of medications for anemia. Low HGB gives the right to suspect the presence of internal bleeding, kidney dysfunction, malignant neoplasms, and bone marrow damage.
- Erythrocyte indices (MCV, MCH, MCHC). The indicators give an idea of the state of red blood cells and their functionality. MCV is the average volume of one red blood cell; it increases with diseases of the liver and hematopoietic system, lack of folic acid and vitamin B12. Decreased in some types of anemia, hyperthyroidism, hemoglobinopathy. MCH shows the average hemoglobin content in one red blood cell. Analogous to color index. MCHC – average concentration of red blood pigment. The interpretation is carried out taking into account other indices.
- Hematocrit level. Allows you to assess the severity of anemia associated with iron deficiency. Exceeding the norm indicates dehydration, extensive burns, and inflammation of the peritoneum. A low figure gives the right to suspect pathologies of the heart and vascular system, kidney disease, blood disease, extensive blood loss, malaria, and poisoning.
- Reticulocyte count. Exceeding the norm is observed in case of blood loss, poisoning, taking certain medications, during the recovery period after treatment of cancer, diseases of the hematopoietic system, metastases in the bone marrow. A decrease in the number of young red blood cells is caused by: anemia, kidney disease, chronic infections, bone marrow tumors, blood pathologies, myxedema of the thyroid gland, chemotherapy, deficiency of folic acid and vitamin B12.
- ESR. Decreases in heart pathologies, joint diseases, anaphylactic shock. Exceeding the norm is observed during pregnancy, anemia, severe poisoning, exacerbations of chronic diseases, and inflammatory processes in the body.
- Color. Hyperchromia (exceeding the norm) indicates a deficiency of cyanocobalamin, possible polyps in the stomach, various malignant tumors, and a lack of vitamin B9. Hypochromia (decreased color index) indicates anemia or lead poisoning. With normochromia, the doctor looks at the values of other, more informative indicators.
Clinical blood test is a laboratory study assessing the quantitative and qualitative characteristics of all classes of blood cells, including a cytological examination of a peripheral blood smear to calculate the percentage of leukocyte varieties and determine the erythrocyte sedimentation rate.
Synonyms Russian
Complete blood count (CBC), hemogram, CAC, complete blood count.
English synonyms
Complete Blood Count (CBC), Hemogram, CBC with White Blood Cell Differential Count, Peripheral Blood Smear, Blood Film Examination.
What biomaterial can be used for research?
Venous blood, capillary blood.
How to properly prepare for research?
- Eliminate alcohol from your diet for 24 hours before the test.
- Children under 1 year of age should not eat for 30-40 minutes before the test.
- Children aged 1 to 5 years should not eat for 2-3 hours before the test.
- Do not eat for 8 hours before the test; you can drink clean still water.
- Avoid physical and emotional stress for 30 minutes before the test.
- Do not smoke for 30 minutes before the test.
General information about the study
A clinical blood test is performed to diagnose quantitative and qualitative changes in the formed elements - blood cells: red blood cells, leukocytes and platelets. Their changes may be caused by disturbances in the hematopoietic process, but most often they are reactive in nature - they reflect the reaction of hematopoiesis to other pathological conditions and diseases. Therefore, a clinical blood test is one of the most common routine tests and is used by doctors of various specialties; it plays a leading role in the primary diagnostic search.
Both venous and capillary blood can be used for the study, with venous blood being preferable. The collection is performed using a vacuum system, most often from the veins in the elbow. A special tube called a vacutainer already contains an anticoagulant (EDTA), which prevents blood clotting. The volume of blood drawn into the vacutainer must correspond to the mark on it - this way the required concentration of the anticoagulant is achieved, which prevents the formation of microclots and, as a result, incorrect calculation of the number of cellular elements and distortion of their morphological structure.
Currently, a clinical blood test is most often performed on a hematology analyzer - a high-tech device that can detect and automatically calculate more than 30 blood characteristics, including counting formed elements, including the main populations of leukocytes. The operating principle of hematology analyzers is based on the passage of a cell suspension through a sensitive element - a laser beam or electric current. Each cell refracts the laser or changes the resistance of the electric current; these changes are proportional to the size of the cell, which is what the analyzer is based on to distinguish them.
If there are deviations in the results of a study on a hematology analyzer, the laboratory diagnostics doctor performs a morphological study of the blood smear. Smear microscopy was included initially in this study. To visually count the formed elements, one or two drops of blood are dripped onto a glass slide, another glass is used to smear it into a thin layer in one motion and is fixed with special substances. The smears are then stained with dyes to make it easier to distinguish and visualize cells and are examined by a doctor under a microscope. Traditionally, the count is carried out per hundred cells and the resulting numbers are recorded as percentages. Knowing the total number of leukocytes, percentages can be converted into absolute values, which much more objectively reflect the state of the leukocyte population.
Parameters determined in the study
Red blood cells are the most numerous blood cells; their main function is the transport of oxygen, which they perform with the help of a special protein they contain - hemoglobin. The hematology analyzer determines the number of red blood cells, hemoglobin content, hematocrit and, based on this, calculates a number of characteristics - the so-called red blood cell indices.
Red blood cells (RBC, Red Blood Cell) are anucleate cells, formed in the bone marrow from reticulocytes, and have the shape of a biconcave disk, which allows them to achieve the maximum possible surface area for binding oxygen. Red blood cells have a diameter of 7-10 micrometers, they are elastic and can easily change shape to safely pass through the smallest vessels - capillaries. In a blood smear they appear as pale red round elements with a clearing in the center. The unit of measurement is 1012 per liter (trillion cells per liter).
Hemoglobin (HGB) is a protein, the main component of red blood cells, which has an affinity for oxygen, which ensures the transport function of red blood cells. Oxygenated hemoglobin gives red blood cells and blood in general their red color.
Hematocrit (HCT) – characterizes the ratio of the volume of red blood cells and plasma. This is a calculation parameter - the hematology analyzer calculates the volume of red blood cells from their number and the average cell volume (MCV).
Mean Corpuscular Volume (MCV, Mean Corpuscular Volume) – is calculated by the analyzer by dividing the sum of cell volumes by the number of red blood cells. It may have a normal value if both microcytosis and macrocytosis are present in the blood. In such situations, you should pay attention to the RDW parameter. The unit of measurement is femtoliter.
The average hemoglobin content in an erythrocyte (MCH, Mean Corpuscular Hemoglobin) – reflects the degree of saturation of the erythrocyte with hemoglobin. Calculated by dividing the hemoglobin concentration by the number of red blood cells.
The average hemoglobin concentration in an erythrocyte (MCHC, Mean Corpuscular Hemoglobin Concentration) also characterizes the saturation of an erythrocyte with hemoglobin. Calculated by dividing hemoglobin by hematocrit.
Distribution of erythrocytes by volume (RDW, Red Cell Distribution Width) - characterizes the degree of variability of erythrocyte volume - anisocytosis. If there is a population of red blood cells in the blood with an altered, but fairly uniform size, RDW values may remain normal. With pronounced differences in the volume of red blood cells, when MCV, which characterizes the average volume of all cells, is normal, RDW will be increased.
Platelets (PLT, Platelet) are blood cells involved in stopping bleeding by forming blood clots. They are not cells; they are fragments of the cytoplasm of bone marrow megakaryocytes. Diameter 2-4 microns.
Mean platelet volume (MPV, Mean Platelet Volume) – platelet volume decreases as cells age, so an increase in this parameter indicates a predominance of young platelets in the population.
Platelet distribution by volume (PDW, Platelet Distribution Width) – characterizes the variability of platelet sizes.
Leukocytes (WBC, White Blood Cell) are a heterogeneous population of nucleated blood cells, the main function of which is to protect the body from foreign agents. Leukocytes include cells of the granulocytic (eosinophils, basophils, neutrophils), monocyte and lymphoid (T- and B-lymphocytes) series. Modern analyzers can differentiate the main five types of leukocytes, but smear microscopy is still the most accurate method for assessing the leukocyte population, as it allows not only to determine the number of different leukocytes, but also to identify changes in their morphology, as well as detect atypical cells.
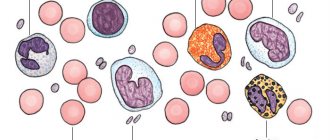
The percentage of different types of leukocytes in a blood smear is called the leukocyte formula . Staining of blood smears allows you to differentiate 5 types of leukocytes due to different staining of the nuclei and intracellular space (cytoplasm):
- Neutrophils are granulocytic leukocytes: their cytoplasm contains granules with specific active substances that allow them to perform their protective functions (capture and destroy foreign objects). Neutrophils also have a nucleus, according to the structure of which they are divided into band-nuclear and segmented (this is the final stage of maturation following the band-nucleus, at which the nucleus is divided by constrictions into 4-5 lobes). When stained, neutrophil granules turn purple, which, together with the peculiarity of the nucleus, allows them to be distinguished from other granulocytes.
- Eosinophils are granulocytes involved in allergic reactions and antiparasitic immunity. Their granules contain mediators of allergy and inflammation. Eosinophils have a two-segmented nucleus, and their granules are orange-pink in color.
- Basophils are granulocytes that take an active part in immediate allergic reactions. They have an S-shaped non-segmented nucleus, which is often not visible due to large granules of intense blue color containing allergy mediators.
- Lymphocytes are cells with a large nucleus, practically devoid of cytoplasm. Their nucleus is colored intense purple-violet, and the cytoplasm is blue-blue. Lymphocytes participate in more complex immune reactions associated with the recognition of their own and foreign antigens.
- Monocytes are relatively large leukocytes containing an unsegmented bean-shaped nucleus and, unlike lymphocytes, a large amount of cytoplasm. When stained, the nucleus becomes purplish-red, and the cytoplasm is a cloudy bluish-gray. The main function of monocytes is phagocytosis, that is, the absorption and digestion of microorganisms, their own dying cells, etc.
The above types of leukocytes are found normally in a peripheral blood smear. In some diseases, cells that normally should not be in the smear may enter the blood from the bone marrow: for example, blasts are the morphological substrate of acute leukemia. In the conclusion to the study, the number and, if possible, morphological features of atypical cells must be indicated.
In addition to counting leukocytes, microscopy evaluates the morphological characteristics of red blood cells - their size, shape. These parameters are important in the diagnosis of various acquired and congenital anemias.
Erythrocyte sedimentation rate . The test is based on the ability of red blood cells to settle under the influence of gravity in blood that is deprived of the ability to clot. Normally, red blood cells settle slowly; this process is accelerated by agglutination - the sticking of red blood cells to each other, which leads to an increase in the mass of settling particles. Ordinary red blood cells have a negative charge on the membrane, which helps them repel each other. In infectious-inflammatory, autoimmune and some tumor (especially paraproteinemic hemoblastoses) diseases, the protein composition of the plasma changes towards an increase in the content of proteins (for example, immunoglobulins). All protein molecules reduce the membrane charge of red blood cells, promoting their gluing to each other and increasing the rate of sedimentation. The test is carried out for an hour, the height of the resulting sediment is measured in millimeters.
What is the research used for?
- To assess general health (routine medical examinations, screening examinations, etc.);
- For diagnostics at the first stage of a wide range of diseases that may manifest themselves as changes in the characteristics of peripheral blood;
- Monitoring of peripheral blood parameters in diseases accompanied by quantitative and qualitative changes;
- To monitor the toxicity of treatment if the methods used may affect the composition of peripheral blood (for example, chemotherapy, radiation therapy).
When is the study scheduled?
- During screening examinations;
- As a primary diagnosis for suspected diseases that may be accompanied by changes in the cellular composition of the blood;
- In the presence of hematopoietic diseases;
- To monitor the effectiveness and toxicity of treatment.
What do the results mean?
Reference values
Leukocytes
| Age | Reference values |
| Less than 1 year | 6 - 17.5 *10^9/l |
| 1-2 years | 6 - 17 *10^9/l |
| 2-4 years | 5.5 - 15.5 *10^9/l |
| 4-6 years | 5 - 14.5 *10^9/l |
| 6-10 years | 4.5 - 13.5 *10^9/l |
| 10-16 years | 4.5 - 13 *10^9/l |
| More than 16 years | 4 - 10 *10^9/l |
Red blood cells
| Age | Floor | Red blood cells, *10 ^12/ l |
| 3,9-5,9 | ||
| 14 days – 1 month. | 3,3-5,3 | |
| 1-4 months | 3,5-5,1 | |
| 4-6 months | 3,9-5,5 | |
| 6-9 months | 4-5,3 | |
| 9-12 months | 4,1-5,3 | |
| 1-3 years | 3,8-4,8 | |
| 3-6 years | 3,7-4,9 | |
| 6-9 years | 3,8-4,9 | |
| 9-12 years | 3,9-5,1 | |
| 12-15 years | male | 4,1-5,2 |
| female | 3,8-5 | |
| 15-18 years old | male | 4,2-5,6 |
| female | 3,9-5,1 | |
| 18-45 years old | male | 4,3-5,7 |
| female | 3,8-5,1 | |
| 45-65 years | male | 4,2-5,6 |
| female | 3,8-5,3 | |
| > 65 years old | male | 3,8-5,8 |
| female | 3,8-5,2 |
Hemoglobin
| Age | Floor | Hemoglobin, g / l |
| 134-198 | ||
| 14 days – 1 month. | 107-171 | |
| 1-2 months | 94-130 | |
| 2-4 months | 103-141 | |
| 4-6 months | 111-141 | |
| 6-9 months | 114-140 | |
| 9-12 months | 113-141 | |
| 1-5 years | 110-140 | |
| 5-10 years | 115-145 | |
| 10-12 years | 120-150 | |
| 12-15 years | male | 120-160 |
| female | 115-150 | |
| 15-18 years old | male | 117-166 |
| female | 117-153 | |
| 18-45 years old | male | 132-173 |
| female | 117-155 | |
| 45-65 years | male | 131-172 |
| female | 117-160 | |
| > 65 years old | male | 126-174 |
| female | 117-161 |
Hematocrit
| Age | Floor | Hematocrit, % |
| 41-65 | ||
| 14 days – 1 month. | 33-55 | |
| 1-2 months | 28-42 | |
| 2-4 months | 32-44 | |
| 4-6 months | 31-41 | |
| 6-9 months | 32-40 | |
| 9-12 months | 33-41 | |
| 1-3 years | 32-40 | |
| 3-6 years | 32-42 | |
| 6-9 years | 33-41 | |
| 9-12 years | 34-43 | |
| 12-15 years | male | 35-45 |
| female | 34-44 | |
| 15-18 years old | male | 37-48 |
| female | 34-44 | |
| 18-45 years old | male | 39-49 |
| female | 35-45 | |
| 45-65 years | male | 39-50 |
| female | 35-47 | |
| > 65 years old | male | 37-51 |
| female | 35-47 |
Mean erythrocyte volume (MCV)
| Floor | Age | Reference values |
| Less than 1 year | 71 – 112 fl | |
| 1-5 years | 73 – 85 fl | |
| 5-10 years | 75 – 87 fl | |
| 10-12 years | 76 – 94 fl | |
| Female | 12-15 years | 73 – 95 fl |
| 15-18 years old | 78 – 98 fl | |
| 18-45 years old | 81 – 100 fl | |
| 45-65 years | 81 – 101 fl | |
| More than 65 years | 81 – 102 fl | |
| Male | 12-15 years | 77 – 94 fl |
| 15-18 years old | 79 – 95 fl | |
| 18-45 years old | 80 – 99 fl | |
| 45-65 years | 81 – 101 fl | |
| More than 65 years | 81 – 102 fl |
Average hemoglobin content in erythrocytes (MCH)
| Age | Floor | Reference values |
| 30 - 37 pg | ||
| 14 days - 1 month. | 29 - 36 pg | |
| 1 - 2 months | 27 - 34 pg | |
| 2 - 4 months | 25 - 32 pg | |
| 4 - 6 months | 24 - 30 pg | |
| 6 - 9 months | 25 - 30 pg | |
| 9 - 12 months | 24 - 30 pg | |
| 1 – 3 years | 22 - 30 pg | |
| 36 years | 25 - 31 pg | |
| 6 – 9 years | 25 - 31 pg | |
| 9-15 years | 26 - 32 pg | |
| 15-18 years old | 26 - 34 pg | |
| 18-45 years old | 27 - 34 pg | |
| 45-65 years | 27 - 34 pg | |
| > 65 years old | female | 27 - 35 pg |
| > 65 years old | male | 27 - 34 pg |
Mean erythrocyte hemoglobin concentration (MCHC)
| Age | Reference values |
| Less than 1 year | 290 – 370 g/l |
| 1-3 years | 280 – 380 g/l |
| 3-12 years | 280 – 360 g/l |
| 12-19 years old | 330 - 340 g/l |
| More than 19 years | 300 – 380 g/l |
Platelets
| Age | Reference values |
| Less than 10 days | 99 - 421 *10^9/l |
| 10 days – 1 month | 150 – 400 *10^9/l |
| 1-6 months | 180 – 400 *10^9/l |
| 6 months – 1 year | 160 - 390 *10^9/l |
| 1-5 years | 150 – 400 *10^9/l |
| 5-10 years | 180 - 450 *10^9/l |
| 10-15 years | 150 – 450 *10^9/l |
| More than 15 years | 150 – 400 *10^9/l |
RDW-SD (red blood cell volume distribution, standard deviation): 37 - 54.
RDW-CV (red blood cell volume distribution, coefficient of variation)
| Age | RDW-CV, % |
| 14,9 — 18,7 | |
| > 6 months | 11,6 — 14,8 |
Platelet distribution by volume (PDW): 10 - 20 fL.
Mean platelet volume (MPV): 9.4 - 12.4 fL.
Large platelet count ratio (P-LCR): 13 – 43%.
Neutrophils (NE)
| Up to 4 years | 1.5 - 8.5 *10^9/l |
| 4-8 years | 1.5 - 8 *10^9/l |
| 8-16 years | 1.8 - 8 *10^9/l |
| More than 16 years | 1.8 - 7.7 *10^9/l |
Lymphocytes (LY)
| Up to 1 year | 2 - 11 *10^9/l |
| 1-2 years | 3 - 9.5 *10^9/l |
| 2-4 years | 2 - 8 *10^9/l |
| 4-6 years | 1.5 - 7 *10^9/l |
| 6-8 years | 1.5 - 6.8 *10^9/l |
| 8-10 years | 1.5 - 6.5 *10^9/l |
| 10-16 years | 1.2 - 5.2 *10^9/l |
| More than 16 years | 1 - 4.8 *10^9/l |
Monocytes (MO)
| Up to 1 year | 0.05 - 1.1 *10^9/l |
| 1-2 years | 0.05 - 0.6 *10^9/l |
| 2-4 years | 0.05 - 0.5 *10^9/l |
| 4-16 years | 0.05 - 0.4 *10^9/l |
| More than 16 years | 0.05 - 0.82 *10^9/l |
Eosinophils (EO)
| Up to 1 year | 0.05 - 0.4 *10^9/l |
| 1-6 years | 0.02 - 0.3 *10^9/l |
| More than 6 years | 0.02 - 0.5 *10^9/l |
Basophils (BA): 0 - 0.08 *10^9/l.
Neutrophils, % (NE%)
| Up to 1 year | 16 — 45 % |
| 1-2 years | 28 — 48 % |
| 2-4 years | 32 — 55 % |
| 4-6 years | 32 — 58 % |
| 6-8 years | 38 — 60 % |
| 8-10 years | 41 — 60 % |
| 10-16 years | 43 — 60 % |
| More than 16 years | 47 — 72 % |
Lymphocytes,% (LY%)
| Up to 1 year | 45 — 75 % |
| 1-2 years | 37 — 60 % |
| 2-4 years | 33 — 55 % |
| 4-6 years | 33 — 50 % |
| 6-8 years | 30 — 50 % |
| 8-10 years | 30 — 46 % |
| 10-16 years | 30 — 45 % |
| More than 16 years | 19 — 37 % |
Monocytes, % (MO%)
| Up to 1 year | 4 — 10 % |
| 1-2 years | 3 — 10 % |
| More than 2 years | 3 — 12 % |
Eosinophils,% (EO%)
| Up to 1 year | 1 — 6 % |
| 1-2 years | 1 — 7 % |
| 2-4 years | 1 — 6 % |
| More than 4 years | 1 — 5 % |
Basophils,% (BA%): 0 - 1.2%.
Erythrocyte sedimentation rate (photometry)
| Male | Up to 15 years | 2 - 20 mm/h. |
| 15-50 years | 2 - 15 mm/h. | |
| More than 50 years | 2 - 20 mm/h. | |
| Female | Up to 15 years | 2 - 20 mm/h. |
| 15-50 years | 2 - 20 mm/h. | |
| More than 50 years | 2 - 30 mm/h. |
A clinical blood test includes a relatively large number of parameters that must be interpreted in combination. Most often, based on the results of the hemogram, the range of studies necessary to clarify the causes of the changes identified in it is determined.
Changes in erythrocyte parameters. A decrease in the level of hemoglobin and erythrocytes are laboratory manifestations of anemia, and changes in erythrocyte indices characterize its pathogenetic variant and help clarify the causes. Increased levels of red blood cells and hemoglobin may indicate a myeloproliferative disorder (polycythemia vera), but also occurs as a compensatory reaction in active smokers, people with respiratory diseases and heart defects.
Changes in platelets. An increase in platelet count may be a manifestation of essential thrombocythemia (a hematological disease characterized by excess production of platelets in the bone marrow), but also occurs as a compensatory reaction after massive bleeding. A decrease in platelet count is observed with an enlarged spleen, immune thrombocytopenia, as well as aplastic anemia, where it will be combined with a decrease in red blood cells and leukocytes.
Changes in leukocytes. Leukocytosis is considered a manifestation of infectious and inflammatory diseases, and the appearance in the blood smear of a large number of young forms of neutrophils - band and even metamyelocytes (this is called a shift of the leukocyte formula to the left) is characteristic. But too high an increase in the level of leukocytes may be a consequence of an oncohematological disease - acute or chronic leukemia. In this case, morphologically changed cells are found in the blood smear, as well as immature forms of leukocytes (blasts), which normally should not enter the peripheral blood. Leukopenia can accompany severe infectious diseases and in this case characterize the depletion of the leukocyte lineage, and be a consequence of inhibition of bone marrow hematopoiesis, for example, against the background of tumor metastases in the bone marrow.
Erythrocyte sedimentation rate. It is a nonspecific parameter indicating changes in the protein composition of plasma. Most often this is caused by infectious-inflammatory, autoimmune and oncological diseases.