Hypertension in old age is usually quite severe. That is why blood pressure medications for older people should work as gently as possible, but at the same time effectively.
Medicines from the following groups are prescribed:
- diuretics (diuretics);
- ACE inhibitors;
- calcium channel blockers;
- statins;
- beta blockers.
When calculating the dosage, several factors are taken into account, in particular, the current stage of tachycardia and the age of the patient.
Diuretics
To reduce blood pressure in older people, drugs and groups of diuretics are often used. A decrease in blood pressure occurs due to a strong diuretic effect. For older people, diuretics are prescribed in small dosages. Otherwise, an increase in blood cholesterol levels is possible.
The list of most commonly used drugs is presented by the following representatives of the group:
- Amiloride. Has a weak diuretic effect. Prescribed at the initial stage of development of hypertension. The decrease in blood pressure occurs after about 1.5 hours. Contraindication – increased calcium levels in the blood. If side symptoms develop, the drug must be taken every other day.
- Metolazone. In addition to normalizing blood pressure, it helps cope with edema. With long-term use, the development of hapokalemia cannot be ruled out.
- Indapamide. Recommended for high blood pressure in elderly patients with diagnosed diabetes. Used as an independent remedy at the beginning of the onset of the disease. It helps well in the treatment of hypertension in women during menopause.
- Furosemide. It has an active but short-lived diuretic effect. The effect is observed after 15 minutes of taking the tablet and lasts for the next three hours. Contraindication: renal failure.
Advantages of treatment and rehabilitation of patients with hypertension in boarding houses and rest homes
The private boarding house has created comfortable conditions for the rehabilitation of elderly people with hypertension. Residents are under 24-hour supervision by medical staff. In critical situations, acute attacks are quickly stopped with effective medications.
In combination with medication support, therapeutic exercises and exercises on exercise bikes are carried out. Patients spend a lot of time outdoors. If an elderly person begins to worry and feel sad, psychologists come to the rescue. The staff of the boarding house takes their duties responsibly. Elderly people feel completely safe.
Calcium antagonists
When taking drugs of this group, a decrease in calcium ions occurs, which contributes to the expansion of the lumen of the coronary vessels. The medicine has a prolonged effect, so normalization of blood pressure occurs slowly and gently.
Among the drugs in this group for high blood pressure, the following drugs have received good recommendations:
- Nifedipine. Practically ineffective for advanced hypertension. Well tolerated in old age. Shows excellent results in various forms of hypertension, including kidney disease.
- Adalat. The active ingredient is nifedipine. The drug is recommended for use in the development of hypertensive crisis. The dosage is selected individually in each specific case.
- Isotropine. Affects myocardial function. The average daily dose of the drug is 240...280 mg. Take it morning and evening. An increase in dosage is justified if the prescribed dosage does not bring the expected therapeutic effect.
- Amlodipine. Used to normalize blood pressure in elderly patients with excess weight, diabetes and atherosclerosis.
Beta blockers
The effect of taking beta-blockers is based on a decrease in the activity of beta-adrenergic receptors located in myocardial tissue.
Beta-blockers can be used both as a single drug and as part of combination therapy
List of drugs used:
- Tenoric. It is used in the treatment of pathology both as an independent remedy and as part of a complex treatment. Has a cumulative effect. The maximum effect is observed two to four hours after taking the tablet.
- Metoprolol. Used for arrhythmias. It has a prolonged effect, so you need to take the tablet once a day at the same time. There is no withdrawal syndrome.
- Betaxalol. Reduces blood pressure, prevents the development of hypertensive crisis against the background of psycho-emotional and physical stress. Does not interfere with glucose metabolism. At the very beginning of treatment, weakness and slight numbness of the limbs may appear. The condition goes away on its own within a few days.
Pharmacotherapy of arterial hypertension in elderly patients
The issues of rational pharmacotherapy of arterial hypertension (AH) and the optimal choice of antihypertensive drugs are important and relevant for a variety of categories of patients, but they are of particular importance for patients who have a variety of concomitant conditions, diseases and risk factors. All this fully applies to elderly and senile patients who, in addition to hypertension, have a wide range of concomitant pathologies. Frequent concomitant diseases among them are coronary heart disease (CHD), chronic obstructive pulmonary disease (COPD), diseases of the gastrointestinal tract, thyroid pathology, metabolic syndrome, etc. These diseases significantly increase the risk of general and cardiovascular mortality, which requires improving the tactics of managing elderly patients [1, 2].
A rational choice of pharmacotherapy also requires taking into account a number of factors on which the choice of a particular class of drugs depends. In elderly and senile people, first of all, the features of the formation and pathogenesis of high blood pressure (BP) and the features of the pharmacokinetics and pharmacodynamics of drugs should be taken into account [3].
Features of hypertension in the elderly
Although the reasons leading to the development of hypertension are the same in all patients, regardless of age, in the elderly, during the aging process, additional prerequisites for the development of hypertension appear, such as hypoxic damage and age-related functional restructuring of the diencephalic-hypothalamic structures of the brain, age-related changes in the sympathoadrenal (SAS) and renin-angiotensin-aldosterone systems (RAAS); age-related decrease in elasticity, increased rigidity, as well as atherosclerotic changes in the aorta and large arteries; worsening dysfunction of the vascular endothelium and reducing its ability to produce vasodilating substances; ischemic changes in the kidneys and heart; deterioration of blood rheology, microcirculation and tissue metabolism; increase in body weight, decrease in physical activity, increase in the duration of bad habits.
There is a low concentration of plasma aldosterone, which correlates with the level of angiotensin and plasma renin activity. All this determines the characteristics and formation of the most common variant of hypertension in the elderly - isolated systolic hypertension (ISAH), which is characterized by an increase in the stiffness of the aorta and large arteries, a decrease in the damping role of the blood wave in large and small arteries, an increase in systolic blood pressure (SBP) and a decrease diastolic blood pressure (DBP). The prevalence of ISAH is 0.1% among persons under 40 years of age, 0.8% among those aged 40–49 years, 5% among those aged 50–59 years, 12.6% among those aged 60–69 years, and 23 .6% - aged 70–80 years. This increase in the number of patients with ISAH is associated with the fact that an increase in SBP occurs at least until the age of 80, while DBP after 50 years either remains at the same level or tends to decrease [2]. Data from the Framingham study indicate that in people of all age groups, the risk of developing cardiovascular complications (CHD, including myocardial infarction, stroke, heart failure, atherosclerosis of peripheral arteries) has close correlations, primarily with the level of systolic and not diastolic blood pressure. The risk of developing chronic heart failure during a 34-year follow-up was 2.3 times higher in men and 3.0 times higher in women when comparing groups of people with the lowest and highest systolic blood pressure.
In patients over 60 years of age, a peculiar form of hypertension may occur with frequent short-term, asymptomatic rises in blood pressure to high levels, which are alternated by a drop in blood pressure below normal values. Such episodes can occur either for no apparent reason or as a result of taking low doses of antihypertensive drugs. The quality of life in such patients deteriorates significantly, primarily due to the fear of waiting for the next rise or fall in blood pressure. Prescribing antihypertensive drugs, even in small doses, can lead to aggravation of the severity of hypotensive conditions. In the pathogenesis of this variant of hypertension, disorders of the autonomic nervous system at various levels associated with age-related degenerative changes play an important role.
Features of hypertension in the elderly are also “pseudohypertension”, associated primarily with increased vascular stiffness, “white coat hypertension”, increased blood pressure variability, as well as episodes of postprandial and orthostatic hypotension. Hypertension in elderly patients is often accompanied by metabolic disorders (dyslipidemia, diabetes mellitus, gout, obesity), the presence of which increases the overall risk of developing cardiovascular complications. The presence of left ventricular myocardial hypertrophy in elderly patients increases the risk of sudden death. The decline in glomerular filtration rate and kidney function with age requires dynamic monitoring of urea, creatinine and electrolyte levels.
Features of pharmacokinetics and pharmacodynamics of drugs in the elderly
With age, processes progress that significantly affect the bioavailability and, ultimately, the effectiveness of drugs. Of great importance are age-related changes in the gastrointestinal tract (hypokinesia of the stomach and intestines, atrophic changes in their mucous membrane, decreased blood flow), which ultimately lead to a slowdown in the rate of gastric emptying and a decrease in active absorption.
Decrease in muscle mass, total and percentage body water, plasma volume, albumin concentration and adipose tissue content, as well as age-related atherosclerotic changes in blood vessels also contribute to a decrease in the volume of distribution of water-soluble and fat-soluble substances. The rate of pharmacokinetic processes changes, determining both the rate of biotransformation of xenobiotics due to a decrease in the activity of liver enzymes and a decrease in its blood supply, and the rate of renal excretion of drugs. With age, the mass of the kidneys, the number of functioning glomeruli, the rate of renal blood flow (in patients over 70 years old it is 2 times lower than in middle-aged people) and glomerular filtration decrease.
Also, with age, the density of receptors, the dynamics of ion channels, the activity of enzyme systems responsible for the formation of the pharmacological effect on drugs change, homeostatic mechanisms are weakened, which can often lead to hypotonic states during antihypertensive therapy, hypoglycemia during treatment with hypoglycemic agents.
Principles of antihypertensive therapy in the elderly
All of the above factors determine the features of the approach and principles of antihypertensive pharmacotherapy in elderly patients:
- when selecting adequate doses of antihypertensive drugs, it is necessary to monitor blood pressure in both sitting and standing positions;
- A sharp decrease in blood pressure should be avoided, especially with the appearance and/or worsening of heart failure;
- It is advisable to begin treatment with monotherapy with any antihypertensive drug in a small dose, which is gradually, at intervals of several weeks, increased until a sufficient antihypertensive effect is achieved, which avoids a rapid decrease in blood pressure that is poorly tolerated by elderly patients and orthostatic disorders, accompanied by worsening cerebral and renal failure , on the other hand, makes it possible to gradually find the minimum effective dose and continue treatment with a low probability of side effects;
- individual selection of drugs for initial treatment should be made taking into account concomitant pathology, individual pathophysiological characteristics of hypertension, indications and limitations for certain groups of drugs;
- preference should be given to long-acting drugs with the most optimal metabolic profile;
- You should not use drugs that can cause orthostatic hypotension (α-blockers) and impaired cognitive function (central α-2-adrenergic agonists).
Particular attention in the European and national recommendations of the latest revision is paid to the target level of blood pressure, which for elderly patients with SBP more than 160 mm Hg. Art. is 150–140 mmHg. Art. (grade of recommendation I, level of evidence A). For elderly patients under 80 years of age who lead an active lifestyle, if treatment is well tolerated, the target SBP level may be less than 140 mmHg. Art. (class of recommendation IIb, level of evidence C) [4, 5].
Choice of antihypertensive drugs in elderly patients
Modern cardiology has a large number of modern antihypertensive drugs, the rational use of which, of course, leads to a reduction in the incidence of adverse outcomes. The issues of optimal and rational choice of a drug (drug), taking into account the peculiarities of their action, are of particular relevance in the primary health care system, since the further prognosis for the patient depends on well-chosen antihypertensive therapy in outpatient clinics. Recommendations summarizing the evidence base for all classes of antihypertensive drugs can be of great help to the practitioner at the stage of choosing pharmacotherapy.
The guidelines for the treatment of hypertension recommend five main classes of drugs that have a convincing evidence base for their effect on prognosis. These are angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), calcium antagonists (CAs), beta-blockers (BABs) and diuretics, which can be prescribed either as monotherapy or as part of combination therapy. All these classes of antihypertensive drugs can be used in elderly patients with hypertension, however, in ISAH, diuretics and calcium antagonists have an advantage (class of recommendations I, level of evidence A) [4, 5].
Of the diuretics, the optimal drug that meets modern requirements is Indapamide retard, which belongs to the thiazide-like diuretics. Its beneficial effects have a large evidence base, which indicates that the drug not only affects blood pressure levels and the condition of target organs, but also reduces mortality rates [6–12]. Indapamide retard is distinguished by good tolerability of treatment and a low incidence of side effects, which is crucial in the treatment of the elderly both from the point of view of maintaining quality of life and from the point of view of ensuring adherence to therapy. A number of studies have shown a lower incidence of hypokalemia, the absence of a negative effect on carbohydrate and lipid metabolism in comparison with classical thiazide diuretics, as well as generally data on good tolerability of treatment with Indapamide retard.
Calcium antagonists
Of the calcium antagonists (CAs), clinical use has mainly been achieved by those that have competitive antagonism of voltage-dependent slow L-type calcium channels. First-generation AKs with a short half-life are well known and have long been used in clinical practice: nifedipine, verapamil, diltiazem. The II generation includes drugs with a long half-life, which are divided into two subclasses: IIa - new dosage forms of prototype drugs with slow release; IIb - drugs that differ from the prototypes in chemical structure and have a slow release. The third generation includes ultra-long-acting dihydpyridine derivatives - amlodipine, lacidipine and lercanidipine [13].
The advantage of all AKs is good tolerability and a wide range of pharmacological effects: antianginal, antihypertensive, cytoprotective, antithrombotic, and therefore they are widely used in cardiological practice.
One of the new third-generation AKs is lercanidipine (the original drug Lerkamen®), which, due to its high lipophilicity and vascular selectivity, is capable of providing a gradually developing and long-lasting antihypertensive effect when taken once a day. Unlike other dihydropyridine AKs, it has very high selectivity for vascular smooth muscle, exceeding its affinity for other types of smooth muscle. The relaxing activity of lercanidipine on the smooth muscle of the rat aorta was 177 times higher than that in the bladder, and 8.5 times higher than in the intestine (for comparison, nitrendipine has the same activity against the three types of tissue tested). Moreover, the concentration ratio required to inhibit contractility by 50% in cardiac/vascular tissue was higher for lercanidipine (730) than for lacidipine (193), amlodipine (95), felodipine (6) and nitrendipine (3) [14] .
The effectiveness of modern antihypertensive drugs provides the opportunity to improve the functional and structural state of target organs. The organoprotective properties of lercanidipine include a reduction in the mass of the left ventricular myocardium [15, 16], nephroprotection [17], and angioprotection [18–20]. It is also important that lercanidipine is metabolically neutral and even has a positive effect on lipid metabolism in patients with mild and moderate hypertension and in patients with type 2 diabetes mellitus (DM) [21].
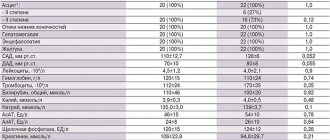
The drug is effective in patients with mild, severe or resistant hypertension (as part of combination therapy) [22], with isolated systolic hypertension, in postmenopausal women with hypertension [23], in patients with type 2 diabetes [21, 24] , as well as in elderly patients (Table) [25–29]. Moreover, lercanidipine in elderly people over 60 years of age is not inferior in effectiveness and tolerability to two other dihydropyridine AKs - amlodipine and lacidipine [26].
The pharmacokinetics of lercanidipine in the elderly and in patients with mild to moderate renal or hepatic dysfunction are little different from those in the general population. No dose adjustment of lercanidipine is required during the initial phase of treatment in elderly patients and patients with mild to moderate renal or hepatic impairment, although initiation of treatment and dose titration in them should be carried out with caution. According to clinical studies, lercanidipine is well tolerated [19, 29, 30]. Most adverse reactions when taking the drug are associated with vasodilation. In the two largest studies (9059 and 7046 patients with mild and moderate hypertension), adverse reactions were noted in 1.6% and 6.5% of patients receiving lercanidipine at a dose of 10 or 20 mg/day, respectively. The most common adverse reactions were: headache (0.2% and 2.9%), swelling of the ankles (0.4% and 1.2%), feeling hot (1.0% and 1.1%) [19 , thirty].
It is recommended to exercise special caution when prescribing it to patients with sick sinus syndrome (unless a pacemaker is implanted). The risk of drowsiness and fatigue when taking lercanidipine is small, but should be taken into account when driving or servicing potentially dangerous machinery.
Conclusion
The calcium antagonist lercanidipine, due to its high lipophilicity and vascular selectivity, is capable of providing a gradually developing and long-lasting antihypertensive effect when taken once a day. The drug is effective in patients with hypertension of different categories, including the elderly. Lercanidipine is as effective as many other current antihypertensive drugs, and the good tolerability profile may contribute to better adherence to long-term antihypertensive therapy with this drug.
This article is an independent opinion piece and is not sponsored.
Literature
- Shalnova S. A., Balanova Yu. A., Konstantinov V. V. et al. Arterial hypertension: prevalence, awareness, use of antihypertensive drugs and the effectiveness of treatment among the population of the Russian Federation // RKZh. 2006; 4:45–50.
- Fletcher A. Epidemiology of Hypertension in the elderly // J Hypertens. 1994; 12 (Suppl. 6).
- Pharmacotherapy of chronic cardiovascular diseases: Guide / Ed. Morozova T. E. 2nd edition, revised. and additional M., 2011. 392 p.
- 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) // Journal of Hypertension. 2013; 31(7):1281–1357.
- Diagnosis and treatment of arterial hypertension. Clinical recommendations of the Ministry of Health of the Russian Federation, 2013. https://cardioweb.ru/klinicheskie-rekomendatsii.
- Gosse Ph., Sheridan D., Zannad F. et al. Regression of left ventricular hypertrophy in hypertensive patients treated with indapamide SR 1.5 mg versus enalapril 20 mg: the LIVE Study // J Hypertension. 2000; 18: 1465–1475.
- Kostis JB, Wilson AC, Fruedenberger RS Long term effect of diuretic based therapy on fatal outcomes in subjects with isolated systolic hypertension with and without diabetes // Am J Cardiol. 2005; 95:29–35.
- Marre M., Garcia-Puig J., Kokot F. et al. Equivalence of indapamide SR and enalapril on microalbuminuria reduction in hypertensive patients with type 2 diabetes: the NESTOR study // J Hypertension. 2004; 22: 1613–1622.
- Marre M., Garcia-Puig J., Kokot F. et al. Efficacy of indapamide SR compared with enalapril in elderly hypertensive patients with type 2 diabetes // Am J Hypertension. 2007; 20: 90–97.
- Peters R., Beckett N., Forette F., Tuomilehto J., Clarke R., Ritchie C. et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial // Lancet Neurol. 2008; 7:683–689.
- The HYVET Study Group. Treatment of Hypertension in Patients 80 Years of Age or Older // N Engl J Med. 2008; 358.
- Weidmann P. Metabolic profile of indapamide sustained-release in patients with hypertension // Drugs Safety. 2001; 24: 1155–1165.
- Morozova T. E., Vartanova O. A. Lercanidipine is a third-generation dihydropyridine with ultra-long action // Consillium medicum. 2011, No. 10, vol. 13, p. 22–29.
- Bang LM, Chapman TM, Goa KL Lercanidipine: a review of efficacy in arterial therapy // Drugs. 2003; 63(22):2449–2472.
- Fogari R., Mugellini A., Corradi L. et al. Efficacy of lercanidipine vs losartan on left ventricular hypertrophy in hypertensive type 2 diabetic patients // J Hypertens. 2000; 18 (Suppl. 2): S65.
- S'anchez A., Sayans R., Alvarez JL et al. Left ventricular hypertrophy regression after a short antihypertensive treatment with lercanidipine vs. enalapril // Fourth European Meeting on Calcium Antagonists. 1999, Oct 27–29; Amsterdam.
- Dalla Vestra M., Pozza G., Mosca A., Grazioli V, Lapolla A., Fioretto P., Crepaldi G. Effect of lercanidipine on the level of albumin excretion in hypertensive patients with type 2 diabetes mellitus in comparison with ramipril // Medicine emergency conditions. 2006, 2 (3).
- Cargnoni A., Benigno M., Ferrari F. et al. Effects of lercanidipine and its enantiomers on ischemia and repefusion-1 // J. Cardiovascular. Pharmacol. 1997; 29 (suppl. 1): S48-S62.
- McClellan KJ, Jarvis B. Lercanidipine. A review of its use in hypertension // Drugs. 2000; 60(5):1123–1140.
- Rossoni G., Bernareggi M., De Gennaro Colonna V. et al. Lercanidipine protects the heart from low–flow ischemia damage and antagonizes the vasopressor activity of endothelin-1 // J. Cardiovascular. Pharmacol. 1997; 29 (suppl. 1): S41-S47.
- Notarbartolo A., Rengo F., Scafidi V. et al. Long-term effects of lercanidipine on the lipoprotein and aholipoprotein profile of patients with mild to moderate essential hypertension // Curr Ther Res. 1999. V. 60 (4): S 228–236.
- Paterna S., Licata A., Arnone S. et al. Lercanidipine in two different dosage regimens as a sole treatment for severe essential hypertension // J Cardiovasc Pharmacol. 1997; 29(Suppl. 2): S50–53.
- Herrera J., Ghais Z., Gonzalez L. Antihypertensive treatment with a calcium channel blocker in postmenopausal women: prospective study in a primary health care setting // J Hypertens. 2002; 20(Suppl. 4): S162.
- Barrios V., Navarro A., Esteras A. et al. Antihypertensive efficacy and tolerability of lercanidipine in daily clinical practice. The ELYPSE study // Blood Press. 2002; 11 (2): S. 95–100.
- Barbagallo M., Barbagallo Sangiorgi G. Efficacy and tolerability of lercanidipine in monotherapy in elderly patients with isolated systolic hypertension // Aging Clin Exp Res. 2000; 12 (5): S. 375–379.
- Leonetti G., Magnani B., Pessina AC et al. Tolerability of longterm treatment with lercanidipine versus amlodipine and lacidipine in elderly hypertensives // Am J Hypertens. 2002; 15(11):S932–940.
- Romito R., Pansini MI, Perticone F. et al. Comparative effect of lercandipine lercandipine, felodipine and nifedipine GITS on blood pressure and heart rate in patients with mild to moderate arterial hypertension: the Lercandipine in Adults (LEAD) study // J Clin Hypertens. 2003; 5(4):S249–253.
- Cherubini A., Fabris F., Ferrari E. et al. Comparative effects of lercanidipine, lacidipine and nifidepine GITS on blood pressure and heart rate in elderly hypertensive patients: the ELderly and LErcanidipine (ELLE) study // Arch Gerontol Geriatr. 2003. V. 3. S203–212.
- Borghi S., Prandin MG, Dormi A. et al. The use of lercanidipine can improve the individual tolerability in dihydropyridine calcium blockers in hypertensive patients // J. Hypertension, 2000; 18 (suppl. 2): S155—S156 (abstract).
- Dedova I. S., Preobrazhensky D. V., Sidorenko B. A., Tarykina E. V., Shaipova A. M. Lercanidipine is a new third-generation calcium antagonist: clinical pharmacology and experience in the treatment of arterial hypertension // Russian Medical magazine. 2006. No. 20, p. 1411–1417.
T. E. Morozova 1, Doctor of Medical Sciences, Professor OA Vartanova, Candidate of Medical Sciences MB Lukina
GBOU VPO First Moscow State Medical University named after. I. M. Sechenova Ministry of Health of the Russian Federation, Moscow
1 Contact information
ACE inhibitors
Medicines from the category of ACE inhibitors practically do not cause side effects when compared with drugs from the group of beta blockers and diuretics.
Important! The use of ACE inhibitors in an elderly person significantly reduces the risk of myocardial infarction.
Treatment is carried out using the following medications:
- Ramipril. Used to stabilize and maintain blood pressure at an acceptable level, depending on the age group.
- Captopril. Often used for high blood pressure in older people, as it reduces it gradually.
- Enalapril. Quickly penetrates into the general bloodstream. Its maximum concentration is observed an hour after taking the tablet. The effect of lowering blood pressure is achieved by reducing the activity of the renin-angiotensin-aldosterone system.
Treatment, prevention and rehabilitation
Healthy people with a hereditary predisposition to hypertension need prevention of hypertension.
It is necessary to control body weight and get rid of excess kilograms. Limit the consumption of fats: sour cream, butter, whole milk. Preference is given to foods rich in proteins: low-fat fish, poultry, cottage cheese, and fermented milk drinks. You should follow a daily routine, get a good night's sleep, and spend at least 2 hours a day in the fresh air. Physical activity should be moderate and not cause fatigue and malaise. If an elderly person suffers from hypertension, he must undergo drug therapy. Other treatment methods are used when the condition normalizes. The regimen and period for taking the drugs is developed by the attending physician, taking into account the individual characteristics of the patient.
An important point in the rehabilitation program for retirees with hypertension is physical therapy. Exercises with a small load on the muscles alternate with loads that require significant effort. They actively use morning exercises, breathing exercises, and Nordic walking. By devoting half an hour to physical activity every day, you can achieve a lasting antihypertensive effect.
Combined treatment
Quite often, in old age, doctors prescribe combination medications for hypertension. Drugs of this group are used if monotherapy does not bring the desired therapeutic result.
A person is prescribed to take several medications from different groups at the same time. In this case, the dosage of each is calculated individually. As a result, this approach significantly reduces the likelihood of developing unpleasant side symptoms and improves the effectiveness of treatment.
In old age, the following schemes are most often used to normalize high blood pressure:
Diuretics for hypertension
- diuretic + calcium antagonist;
- diuretic + beta blocker;
- beta blocker + calcium antagonist;
- ACE inhibitor + calcium antagonist.
In addition, pharmacists offer medicines that initially have a combined composition. Such drugs have several advantages. There is no need to purchase several separate medications. Correct selection of dosages of active substances minimizes the risk of side effects, but at the same time the drug exhibits maximum hypotensive effect.
The most effective combination products:
- Ramigexal Compositum (hydrochlorothiazide and ramipril);
- Azomex N (amlodipine and hydrochlorothiazide);
- Captopres (captopril and hydrochlorothiazide);
- Tarka (verapamil and trandolapril);
- Berlipril Plus (enalapril and hydrochlorothiazide);
- Noliprel (perindopril with indapamide);
- Enzix Duo (indapamide with enalapril);
- Tenoric (atenolol with chlotalidone).
Since hypertension is a chronic disease in old age, blood pressure should be reduced to 120/80 mm. Hg Art. almost impossible. It must be taken into account that medications for hypertension take different times to take effect.
For example, only new generation drugs can simultaneously get rid of headaches and lower blood pressure. Classic diuretics have the necessary effect after two to three hours, but they “work” much longer.
Fast-acting drugs
Fast-acting drugs are prescribed to older patients with heart disease - after myocardial infarction, stroke, various defects, myocarditis, and arrhythmias. The medications act quickly and reduce blood pressure within 15 minutes, preventing the occurrence of increased stress on the myocardium. The duration of the therapeutic effect is no more than six hours.
Indapamide helps to quickly reduce blood pressure levels
In this group of drugs, the following have proven themselves best: Indapamide, Hydrochlorothiazide, Ramipril, Perindopril, Bisoprolol. In addition to normalizing blood pressure, medications improve the condition of the walls of blood vessels and the myocardium.
It is necessary to take medications from this group strictly as prescribed by your doctor, as they can cause serious side effects. The most common include dizziness, nausea and physical weakness. Unpleasant sensations disappear after complete absorption of the medicine taken.
After normalization of blood pressure, in order to maintain the obtained indicator, the person is prescribed a constant intake of “weaker” medications. The following drugs are most often used in a maintenance dosage of 2.5 - 5 mg: Hartil, Tritace, Gopten, Mavik. They must be taken daily and for life.
Exercises to lower blood pressure for the elderly
Staying physically active is a very important aspect. Moderate loads keep the walls of blood vessels toned, promote normal heart function and eliminate congestion. In this case, preference is given to so-called aerobic exercises or cardio exercises - walking in the park, jogging, climbing stairs, yoga and breathing exercises. You need to choose from this list in accordance with the age and condition of the elderly person.
An important principle is to control your heart rate when performing exercises. Traditionally, it is calculated using the formula: 220 - the patient’s age. Thus, for a 70-year-old patient, the number of heartbeats during exercise should not exceed 150 times per minute. If the pulse steadily reaches its maximum, the optimal solution is to switch to deep and slow breathing, while inhaling through the nose and exhaling through the mouth.
A healthy lifestyle and diet are a great help for normalizing blood pressure. But you shouldn’t rely only on them in adulthood - you should definitely consult a doctor to select reliable medications.
Emergency medications
Elderly hypertensive patients need to have in their medicine cabinet products that can provide a rapid hypotensive effect. This:
- Clonidine. A decrease in blood pressure occurs 30 minutes after taking the tablet. Duration of action – 8 hours. Recommended for use in hypertensive crisis.
- Nifedepine. It starts to work very quickly. The tablet must be placed under the tongue.
- Nitroglycerine. The tablet should be placed under the tongue when pain occurs in the heart area.
- Capoten/Captopril. They reduce blood pressure quite quickly. Intended for sublingual use.
- Adelfan. It doesn’t work immediately, but it also works quite quickly.
- Moxonidine. A gradual decrease in blood pressure begins half an hour after taking the dose.
- Propronalol. A decrease in blood pressure occurs 30 minutes after taking the drug. The recommended dosage is 50 mg. The pressure remains stable over the next six hours.
- Furosemide. Has a powerful diuretic effect.
Emergency medications can be taken at any stage of hypertension.
Low blood pressure medications
Low blood pressure - hypotension - is not common in old age. But the condition still exists. And it is necessary to treat the pathology in the same way as hypertension. The following medications help with low blood pressure (they are recommended for a slight decrease in blood pressure):
- Citramon. Helps increase numbers due to the presence of caffeine.
- Papazol. A good remedy. Acts quickly but gently.
- Caffeine. Activates the nervous system and provokes the release of adrenaline into the blood. This is what causes an increase in blood pressure.
- Askofen. Includes caffeine.
- Symptol. It has a fairly strong vasoconstrictor effect. Available in the form of a solution. Place 25 drops of the product on a piece of sugar and eat it before meals.
- Midodrine (Gutron). Causes a decrease in the lumen of blood vessels. Recommended for use if a drop in blood pressure occurs due to stress. Quickly helps with low blood pressure, eliminating characteristic symptoms - dizziness, headache, nausea, flashing black spots before the eyes.
- Ecdisten. Herbal preparation. This blood pressure medication is not recommended to be taken in the evening as it may cause sleep disturbances.
Blood pressure medication for older people suffering from hypotension should be selected by the attending physician. Any medications for blood pressure – high or low – in old age should be selected by a specialist. Self-administration of medications can only worsen your overall health.
Why is it important for patients to maintain a sleep and rest schedule?
The daily routine is about maintaining a balance between rest and wakefulness. A well-designed daily routine corresponds to human biorhythms and helps to avoid physical and mental overload. Eating at certain hours improves the metabolic process and reduces the risk of gaining excess weight. Adequate sleep normalizes the nervous system and strengthens the immune system.
The daily routine is based on regularity. The body will tune in to a repeating rhythm: it will be ready at certain times for active activity, at other times for rest. A person becomes stress-resistant, he is not afraid of pressure surges, he skillfully regulates his emotions.