Publications in the media
An abdominal aortic aneurysm develops, as a rule, as a result of atherosclerotic lesions and is localized below the level of the origin of the renal arteries. Observed much more often than thoracic aortic aneurysm.
Clinical picture • Pain in the abdomen (usually on the left) or back, associated with blood leaking through the artery wall. The pain is intense if the aneurysmal sac compresses the spinal roots • Sensation of pulsation in the abdomen • Intermittent claudication (due to impaired blood supply to the lower extremities).
Diagnostics. Approximately 40% of aneurysms are an incidental finding during clinical or radiological examination • X-ray examination - calcification of the wall of the abdominal aortic aneurysm in 60% of cases • Ultrasound and CT of the abdomen allow the most accurate determination of the location and size of the aneurysm. CT makes it possible to assess in detail the relationship of the aneurysm with the renal and other visceral vessels and identify possible anomalies of the venous bed • Angiography is indicated for patients with arterial hypertension with severe or unstable angina, renal artery stenosis, patients with suspected ischemia of the mesenteric vessels, as well as patients with symptoms of occlusion distal arteries.
Differential diagnosis is carried out with a pancreatic tumor.
TREATMENT
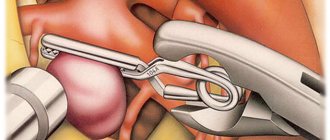
Surgical treatment • Indication for surgery - an increase in the diameter of the aneurysm by more than 0.4 cm/year • Aneurysmectomy with replacement of the aneurysm with an aortic prosthesis made of Dacron or other synthetic material • Before, during and after the operation, careful monitoring of the pressure in the cavities of the heart and the size of cardiac output using a Swan-Ganz catheter.
Conservative treatment • Trepirium iodide, imequin • b-blockers (propranolol) • Sodium nitroprusside • Mannitol is prescribed to stimulate diuresis during surgery • After surgery, urgent correction of acidosis and hyperkalemia may be required.
Complication - rupture of an aneurysm • The risk of rupture depends on the size of the aneurysm (usually an aneurysm is considered large if its diameter is twice the diameter of the vessel): •• Less than 4.5 cm in diameter - 9% •• Diameter from 4.5 to 7 cm - 35 % •• More than 7 cm in diameter - 75% • Diagnostics •• Shock clinic. For small ruptures, blood pressure may remain stable •• Severe abdominal or back pain, at times localized to the lower abdomen, groin, testicles •• Pulsatile abdominal mass in more than 80% of cases •• Direct visualization with CT scans • Surgical treatment Aortic aneurysm ruptures should be carried out immediately after diagnosis. Operative mortality is 50–60%.
Forecast. 90% of patients die from aneurysm rupture within a year.
ICD-10 • I71 Aneurysm and aortic dissection
Note. Atypical aneurysms of the abdominal aorta • Inflammatory aneurysms are characterized by pronounced fibrotic changes in the anterior and lateral walls of the aneurysm and underlying tissues • Septic aneurysms are characterized by fever, leukocytosis and signs of septic embolism. Aneurysms have a saccular shape, atypical localization and slight calcification of the walls.
URGENT CARE. DISLASING AORTIC ANEURYSM
Note:
Clinical suspicion of dissecting aortic aneurysm arises based on history, physical examination, chest x-ray, and ECG. An aneurysm that has been dissecting for less than 2 weeks is classified as acute, while aneurysm that has existed for a longer period of time is classified as chronic. Complications of this condition include progression of the lesion to involve vital organs or extremities, rupture or threatened rupture (eg, formation of a saccular aneurysm), regurgitation in the aortic valve (very rare), retrograde extension of the dissection into the ascending aorta, and inability to control pain and blood pressure with medications. , Marfan syndrome. The proximal aneurysm includes a dissecting aneurysm involving the ascending section and aortic arch, and the distal aneurysm is localized below the origin of the left subclavian artery.
Symptoms of the disease:
• largely depend on the location of the lesion; • characterized by a sudden onset with the appearance of severe “tearing” pain; • pain is most often localized behind the sternum, in the interscapular region, in the lower back (its localization changes as the dissection progresses); • possible loss of consciousness; • both hypertension and hypotension are detected (you should first make sure that blood pressure is not determined in the vessel involved in the dissection process); • with supravalvular localization of the lesion, regurgitation in the aortic valve (in severe cases leading to heart failure) and cardiac tamponade may occur; • pulse deficiency, decreased pulsation amplitude in the vessels involved in the rupture; • symptoms of myocardial ischemia, brain and spinal cord, limbs, and abdominal organs may appear.
Chest X-ray:
• findings are nonspecific and often do not help diagnosis; • possible expansion of the shadow of the aorta (sometimes with the presence of a characteristic protrusion at the site of dissection), less often the mediastinum, the appearance of fluid in the pleural cavity (usually on the left); • a normal radiograph does not exclude the diagnosis.
ECG in 12 leads:
• in the absence of characteristic changes, myocardial ischemia can be excluded as the cause of chest pain; • the presence of changes characteristic of myocardial infarction (usually lower localization) does not exclude dissecting aortic aneurysm.
Aortic imaging methods:
• the choice of method largely depends on capabilities and experience; • transesophageal echocardiography is especially indicated in unstable patient conditions (can be quickly performed at the patient’s bedside, as well as in the operating room immediately before surgery, does not require cessation of monitoring and ongoing therapeutic measures); • computed tomography with contrast agent injection can be used if transesophageal echocardiography is not available; • magnetic resonance is more often used in patients whose condition is stable, in the chronic form of the disease; • aortography is used in cases where a specific diagnosis has not been established using the above studies.
Methods of drug treatment:
• the main goals of treatment include reducing blood pressure and myocardial contractility; • desired level of systolic blood pressure – 100 – 120 mm Hg. Art. or the lowest level that does not cause ischemia of the heart, brain and kidneys in patients with hypertension; • to quickly reduce high blood pressure, they resort to intravenous infusion of sodium nitroprusside or nitroglycerin with the obligatory simultaneous use of a b-blocker; • to quickly reduce myocardial contractility, intravenous administration of b-blockers is carried out in an increasing dose until the heart rate reaches 50 - 60 per minute (propranolol - 1 mg every 3 - 5 minutes until the effect is achieved or up to a total dose of 0.15 mg/kg with repetition after 4 – 6 hours, 2-6 mg; esmolol – bolus 30 mg, then infusion 3-12 mg/min); • both goals can be achieved with labetolol (10 mg intravenously over 2 minutes, then 20 - 80 mg every 10 - 15 minutes to a maximum dose of 300 mg, as a maintenance measure - infusion of 2 - 20 mg / min); • if b-blockers are contraindicated, calcium antagonists that slow the heart rate (verapamil, diltiazem) can be used; • taking short-acting nifedipine drugs orally or sublingually can lead to a rapid decrease in blood pressure even in refractory cases, but is associated with the risk of reflex tachycardia; apparently, these drugs should not be prescribed without prior administration of a b-blocker; • when the renal arteries are involved in the dissection, intravenous administration of an angiotensin-converting enzyme inhibitor (enalapril 0.625 - 5 mg every 4 - 6 hours) may be most effective to reduce blood pressure; • clinically significant hypotension requires rapid intravenous fluid administration; in refractory cases, an infusion of pressor agents is performed (preferably norepinephrine; dopamine is used only in low doses to stimulate urination).
Surgery:
• if there is a suspicion of aortic rupture, as well as cardiac tamponade, it is necessary to take the patient to the operating room as quickly as possible; • the urgency and expediency of surgical intervention depend on the location of the lesion, how long ago the dissection occurred and the presence of complications (see diagram).
| Aortic imaging | |
| • transesophageal echocardiography • computed tomography with contrast agent • magnetic resonance • aortography | |
| Confirmation of the presence of dissecting aortic aneurysm | |
| Surgical treatment: • method of choice for acute proximal dissection • acute distal dissection in the presence of complications | Medical treatment: • treatment of choice for uncomplicated distal dissection • stable isolated aortic arch dissection • stable chronic dissection (uncomplicated dissection 2 weeks or more old) |
Cost of surgery to remove a cerebral aneurysm in Germany
Prices for regular diagnostics in Germany, rehabilitation and recovery after removal of an aneurysm are calculated based on the patient’s condition at the time of contacting the Nordwest clinic. You can consult a doctor to identify an aneurysm by signing up for a video consultation. The acute course of the disease requires immediate hospitalization. Patient relationship managers will provide you with assistance in organizing your treatment as soon as you contact them and go through all the stages of interaction. They will also be able to advise you how much the operation costs to prevent complications in the form of rupture or stroke if the diagnosis has already been established.
Causes of the disease
A cerebral aneurysm can be either a congenital pathology or acquired during life. Usually congenital are combined with many other developmental defects: coarctation of the aorta, polycystic kidney disease, connective tissue diseases. The main causes of aneurysm:
- genetic abnormalities in the structure of the walls of brain vessels;
- pathological infectious processes;
- injuries and tumors;
- development of atherosclerosis and high blood pressure;
- thromboembolism;
- bad habits.
Scientists have not fully studied the causes of the disease and the theory of their occurrence.
Symptoms
More than half of the patients do not know about the existence of the disease, because for a long time the pathology may not manifest itself in any way, especially if the expansion is insignificant and does not compress the surrounding tissues. In rare cases, headaches of varying intensity may be present. The main symptoms of cerebral aneurysm:
- frequent disturbances in speech and coordination of movements;
- vision problems (double vision, blurred vision), of varying severity;
- strabismus and pain in the eye area;
- short-term memory, distracted attention;
- hearing impairment and taste perception;
- pronounced changes in the patient’s mood and behavior;
- signs of fatigue.
All of these symptoms are characteristic not only of this disease. Therefore, for the correct diagnosis and timely treatment of cerebral aneurysm, it is necessary to carry out a set of diagnostic measures to identify the pathology.
Cerebral aneurysms (Cerebral aneurysm)
According to its clinical manifestations, the pathology can have a tumor-like or apoplexy course. In the tumor-like variant, the cerebral aneurysm progressively increases and, reaching a significant size, begins to compress the anatomical structures of the brain located next to it, which leads to the appearance of corresponding clinical symptoms. The tumor-like form is characterized by the clinical picture of an intracranial tumor. It is most often detected in the area of the optic chiasm (chiasma) and in the cavernous sinus.
Anomaly of the vessels of the chiasmal region is accompanied by disturbances in visual acuity and fields; if it persists for a long time, it can lead to optic nerve atrophy. A cerebral aneurysm located in the cavernous sinus may be accompanied by one of three cavernous sinus syndromes, which are a combination of paresis of the III, IV and VI pairs of the cranial nerve with damage to various branches of the trigeminal nerve. Paresis of the III, IV and VI pairs is clinically manifested by oculomotor disorders (weakening or impossibility of convergence, development of strabismus); damage to the trigeminal nerve - symptoms of trigeminal neuralgia. A long-term condition may be accompanied by destruction of the skull bones, revealed by radiography.
Often the disease has an apoplectic course with the sudden onset of clinical symptoms as a result of aneurysm rupture. Only rarely is aneurysm rupture preceded by headaches in the fronto-orbital region.
Aneurysm rupture
The first symptom of a rupture is a sudden, very intense headache. Initially, it may be local in nature, corresponding to the location of the aneurysm, then it becomes diffuse. The headache is accompanied by nausea and repeated vomiting. Meningeal symptoms occur: hyperesthesia, neck stiffness, Brudzinski and Kernig symptoms. Then there is a loss of consciousness, which can last for a variable period of time. Epileptiform seizures and mental disorders ranging from mild confusion to psychosis may occur. Subarachnoid hemorrhage, which occurs when an aneurysmal extension ruptures, is accompanied by a prolonged spasm of the arteries located near the aneurysm. In approximately 65% of cases, this vascular spasm leads to damage to the brain substance such as an ischemic stroke.
In addition to subarachnoid hemorrhage, a ruptured cerebral aneurysm can cause hemorrhage into the substance or ventricles of the brain. Intracerebral hematoma is observed in 22% of cases of rupture. In addition to general cerebral symptoms, it is manifested by increasing focal symptoms, depending on the location of the hematoma. In 14% of cases, a ruptured aneurysm causes hemorrhage into the ventricles. This is the most severe variant of the disease, often leading to death.
The focal symptoms that arise from a rupture can be varied and depend on the location of the aneurysm. When located in the area of the bifurcation of the carotid artery, visual dysfunction occurs. Damage to the anterior cerebral artery is accompanied by paresis of the lower extremities and mental disorders, while the middle cerebral artery is accompanied by hemiparesis on the opposite side and speech disorders. An aneurysm localized in the vertebrobasilar system when ruptured is characterized by dysphagia, dysarthria, nystagmus, ataxia, alternating syndromes, central paresis of the facial nerve and damage to the trigeminal nerve. The protrusion of cerebral vessels, located in the cavernous sinus, is located outside the dura mater and therefore its rupture is not accompanied by hemorrhage into the cranial cavity.