What is heart rate and why does it change with age?
Heart rhythm (heart rate) is an indicator of the number of heartbeats in one minute. The value is purely individual, it directly depends on gender, age, constitution, time of day, general psychological and physical state of a person.
In a newborn, the heart beats at its maximum frequency, but by the age of 13-15 it reaches the levels characteristic of an adult, reducing the rhythm by almost half. It depends on what:
- the myocardium loses its ability to stretch to its maximum;
- the blood volume changes in accordance with the enlargement of the heart chambers;
- the length of blood flow increases;
- the vessels gradually lose their elasticity;
- increased sensitivity to adrenaline.
Since heart rate is a marker of the work of the heart and blood vessels, it is very important to navigate its children’s age norms and, if necessary, control these numbers.
Newborn blood circulation
In newborns, extrauterine circulation is established, and the pulmonary and systemic circulations begin to function.
In the left atrium, blood pressure increases due to the entry of a large amount of blood, and the valve of the oval window mechanically closes. It is generally accepted that closure of the ductus arteriosus occurs under the influence of nervous, muscular and torsion factors. Usually by the 6th week of life the ductus arteriosus closes, and by 2-3 months. - ductus venosus, by 6-7 months. - foramen ovale in the interatrial septum. By cutting off blood flow through the placenta, the total peripheral resistance almost doubles. This in turn leads to an increase in systemic blood pressure , as well as pressure in the left ventricle and atrium. At the same time, there is a gradual significant (about 4 times) decrease in hydrostatic resistance in the pulmonary circulation due to an increase in oxygen tension in the lung tissues (a feature of the smooth muscles of the pulmonary circulation vessels is its reduction in response to hypoxia) to 15-20 mm Hg. Art. by 1-2 months of age.
The consequence of a decrease in the resistance of the vessels of the pulmonary circulation is an increase in the volume of blood flowing through them, as well as a decrease in systolic pressure in the pulmonary artery, right ventricle and atrium.
The heart of a newborn has a large reserve force: a decrease in blood viscosity (due to a decrease in the number of red blood cells), switching off the placental blood circulation (which leads to a decrease in the amount of circulating fetal blood by 25-30% and a shortening of the path that the blood takes), in the postnatal period, the load on the right the ventricle gradually decreases, and the left one increases (in utero, both ventricles do the same work, and the right one even does a little more).
Normal children's heart rate
Despite the fact that a child’s heart rate is individual and can fluctuate relative to the norm, there are still average guidelines for digital heart rate values for different age categories.
In the fetus
The first heartbeat in the fetus is recorded at the 5th week of pregnancy, when the heart already has 4 chambers and exhibits a rhythm of 110 to 190 beats/minute. Heart rate fluctuations persist until childbirth; they are associated with the development of the nervous system.
This is the norm, but even during intrauterine development, disturbances in heart rate can be observed; they are determined by CTG (cardiotocography).
Two sensors are attached to the pregnant woman's belly to record the fetal heart rate. This procedure is carried out after 32 weeks. A heart rate below 120 beats/minute indicates hypoxia, requiring immediate correction. Otherwise, serious complications arise.
In premature babies
Premature birth entails immaturity of internal organs, which requires time to adapt to the environment. Pulse is one of these characteristics, so 180 beats/minute in this case is considered normal.
The permissible range is from 120 to 190 beats/minute. In addition, premature babies have increased irritability: light, sound, unfamiliar smells increase their heart rate, but do not pose a threat to life.
In newborns
The normal pulse rate in children at birth is 120-140 beats/minute. This is a very variable value, which even depends on the time of birth of the baby.
The baby’s heart is still very small and fragile, so any effort, be it crying, laughing, or feeding, causes the heart rate to increase.
Therefore, contrary to the popular belief that a newborn can cry or scream as much as he wants, a state of overexertion is dangerous for the baby. The heart rate reaches 190 beats/minute, which even for a completely healthy baby is a negative reaction and carries a risk of cardiac complications.
In children under one year old
Over the course of 12 months, a small miracle occurs: the baby almost completely adapts to the conditions offered to him. Therefore, with a reasonable diet, daily routine, and appropriate care, he begins to easily overcome unusual sensations.
The pulse follows it and gradually slows down, reaching about 130 beats/minute. This is facilitated by a gradual increase in the volume of the baby’s heart chambers, the amount of blood inside them, and a slowdown in metabolism.
In early childhood
2 – 3 years is a period of intensive growth of internal organs. The heart grows, its ratio compared to body weight changes, and the heartbeat becomes slower.
Normally, the range corresponds to 95 – 155 beats/minute; it is influenced by the baby’s motor activity and his psycho-emotional lability. Heart rate fluctuations can differ significantly from the average norm, but this only speaks about the individual characteristics of the child and is not a pathology.
In preschoolers
The older the baby gets, the slower his pulse and metabolism, the more intense his body growth. From three to six years, heart rate indicators fall within the range from 85 beats/minute (during sleep) to 125 (during outdoor games). Heartbeat is influenced by many factors:
- stress;
- overwork, fatigue, physical stress;
- binge eating;
- temperature changes;
- taking medications.
This age is the time for the first visit to kindergarten, clubs, forced temporary separations from parents, which inevitably affects heart rate.
For schoolchildren
This category includes a very diverse age group from 7 to 17 years old. Naturally, the pulse rate indicators will be very different. It is very important during this period, focusing on the summary table of the age-specific heart rate norm, not to miss the pathology. The following signs indicate it:
- dyspnea;
- retrosternal discomfort;
- cyanosis of the nasolabial triangle;
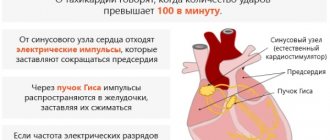
- tachycardia;
- hyperhidrosis.
All this is a reason to visit a doctor.
In teenagers
Teenagers are separated into a separate group based on their puberty period. Fluctuations in hormonal levels associated with sex hormones are significant, followed by the pulse, the norms of which range from 50 to 100 beats/minute.
This is a period of intensive development of many body systems that require increased nutrition, oxygen supply, that is, increased heart rate. Due to the physiology of adolescents, even daily fluctuations in heart rate are significant.
In turn, tachycardia affects the functioning of the heart, causing the risk of unwanted complications. Therefore, the lifestyle of a teenager is very important. If he plays sports, is trained, and is resistant to hyperstress, for him a heart rate at the upper limit of normal is not dangerous.
But if we have an asthenic person, a teenager with a hyperlabile nervous system who uses narcotic substances, we can predict the formation of cardiovascular pathologies.
Growth imbalances, stress, and hyperstress can provoke chest discomfort and tachycardia, which is physiological in nature and disappears without a trace by adulthood. This happens when:
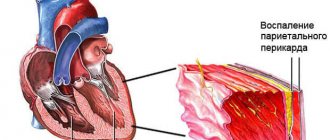
- pericardial entrapment (radicular syndrome);
- respiratory arrhythmia;
- sinus tachycardia.
The borderline state between normal and pathological pulse in adolescents requires a thorough clinical and laboratory examination.
During physical activity
Measuring heart rate in children and adolescents requires taking into account indicators at rest and during physical activity. This makes it possible to identify possible deviations at a very early stage of development. When counting shocks in the area of the vessel, you should pay attention to the rhythm of the strokes.
There is a direct connection between heart rate and exercise: increasing the load increases the heart rate. At the same time, the pulse should not go beyond the average statistical limits. Control is carried out using the formula: 220 minus the child’s age.
For example, for an 11-year-old child, the maximum permissible heart rate during physical activity should not exceed the value: 220 – 11 = 209, and for a 16-year-old: 220 – 16 = 204.
The minimum value is calculated using the following formula: [(220 – age) – number of heartbeats before exercise] x 0.5 + number of heartbeats before exercise = lower limit of heart rate.
For example, for an 11-year-old, the minimum would be: [(220 – 11) – 80] x 0.5 + 80 = 144.5. For a 16-year-old: [(220 – 16) – 60] x 0.5 + 60 = 132.
Such control makes it possible to adjust the load for athletes and hyperactive children. If after squats or running the pulse does not reach the upper limit and does not fall below the lower limit, everything is fine, the load is not maximum, it can be increased.
If not, then you should reduce the load. There is a limit to what the heart can do at any age. If it is exceeded, a life-threatening condition occurs.
During high physical activity, a teenager’s heart can contract at a rate of up to 200–210 beats/min, while maintaining a good stroke volume. This rhythm is very energy-consuming; the heart can withstand it for only a few minutes (sprint burst). Every 10 years the maximum value decreases by approximately 10 strokes.
Treatment
Therapy depends entirely on the specific nosology. Infectious endocarditis and pericarditis are treated with drugs, but tumors or defects require surgical intervention, otherwise the child will grow, and with it pathological holes (or neoplasms) in the organ, which will lead to death.
Conservative treatment
Non-drug methods are recommended for all patients with a predisposition to or presence of cardiac problems. They include:
- normalization of work and rest regimes;
- 8 hours sleep;
- regular moderate physical activity;
- control of salt intake;
- weight loss (if you are overweight);
- avoiding alcohol and smoking;
- changing your diet towards proper nutrition.
Specific drug therapy depends on the cause of cardiac dysfunction. Main groups of drugs:
- Antibiotics (for bacterial etiology);
- Antihypertensives (Beta blockers, diuretics, ACE inhibitors and angiotensin II receptor blockers dilate blood vessels to lower blood pressure);
- Cardiac glycosides (to restore cardiac conduction and contractility);
- Nonsteroidal anti-inflammatory drugs (suppress inflammation);
- Immunosuppressors (for autoimmune processes), etc.
Surgery
The surgeon restores the heart rhythm by implanting a pacemaker. The batteries for it are changed every 5-7 years during repeated surgery.
All affected valves are replaced with artificial ones. In severe cases, a heart transplant is required.
Summary table of heart rate norms in children by age
Approximate heart rate indicators for children by age are presented in the table
| Child's age | Normal limits from minimum to maximum in beats/minute | Average in beats/minute |
| Newborns | 110-170 | 140 |
| Up to a year | 102-162 | 132 |
| Up to two years | 94-155 | 124 |
| Up to 4 years | 90-140 | 115 |
| Up to 6 years | 86-126 | 106 |
| Up to 8 years | 78-118 | 98 |
| Up to 10 years | 68-108 | 88 |
| Up to 12 years | 60-100 | 80 |
| Up to 15 years | 55-95 | 75 |
| Under 18 years old | 60-93 | 75 |
Factors influencing increased and decreased heart rate
The heart rhythm is not constant. Tachycardia or bradycardia in children depends on a number of reasons:
- a small heart beats more often, so in newborns the pulse is maximum, and in adolescents it is almost comparable to that of adults;
- in a hot, stuffy room, the heart rate is higher in children due to imperfect thermoregulation;
- if the baby is sick, hyperthermia causes increased heart rate;
- emotional state affects heart rate;
- Eating changes your heartbeat;
- sleep or wakefulness is reflected in the heart rhythm;
- body position adjusts the heart rate: if the child is sitting, it increases by 10%, if standing - by 20%.
However, in any case, an increase or decrease in heart rate is a sign of pathological changes in the body and requires a thorough examination.
Symptoms and causes of high readings
A high heart rate (tachycardia) is considered normal in children under 7 years of age.
An increase in the child's body temperature by 1 degree increases the pulse by 7-12 beats.
Symptoms:
- painful tremors in the chest area;
- numbness of fingertips;
- feeling of fainting;
- blurred vision;
- cold extremities;
- general weakness.
Causes:
- thyroid dysfunction;
- pathology of the upper chamber of the heart;
- lung disease.
Coffee, tobacco, tea, lack of vitamins, nervousness, fear, rich foods also stimulate an increase in heart rate
And also read: what to do with a rapid pulse at low, normal and high blood pressure?
How to measure a child's pulse
Reliable data on heart rate can be obtained by measuring the pulse with a heart rate monitor or manually (in infants - on the carotid or temporal artery, in older children - on the wrist) according to the following rules:
- the measurement should be carried out in a state of complete rest of the baby (in newborns - immediately after waking up);
- at the same time for several days in a row;
- Before measuring, the child needs to clearly explain the essence of the manipulation so that he does not worry.
Only such an algorithm will be the key to reliable measurements.
What to do if the child’s heart rate does not correspond to the age norm
A normal pulse in a child is evidence of good functioning of the heart, blood vessels, and respiratory organs. If children do not show any complaints and do not have any alarming symptoms, regular heart rate measurement is not necessary.
Accidentally detected deviations from the norm in any direction indicate the formation of pathological processes in the child’s body or an incorrect measurement of heart rate. A control measurement is required. Repeated detection of heart rhythm disturbances warns of serious problems.
Most often we are talking about arrhythmias of various origins, tachycardia or bradycardia.
However, pathology of the bronchopulmonary, endocrine, and hematopoietic systems cannot be excluded. Such pathologies can only be identified by immediately contacting a doctor for a thorough examination. Regular measurements of the child’s pulse and attentive attention to his behavior and complaints can help in timely consultation.
Possible complications
It is necessary to find out the cause of the constant high or low pulse and begin timely treatment. If this rule is ignored, there is a high probability of complications.
Possible consequences:
- loss of consciousness;
- impaired blood circulation in the brain and other organs;
- the formation of blood clots in the heart;
- heart failure;
- death.
Pulse is a criterion by which the state of human health can be determined. PS has different characteristics - frequency, rhythm, content. Most often, the pulse is detected at the wrist or neck. After measurement, the value is compared with the norm. In adolescence (12–17 years), the pulse is slightly higher than in adults. PS may deviate from the optimal value up or down.
This indicates physiological (stress, poor diet, being in an unventilated area) or pathological (cardiovascular, endocrine diseases) reasons. If the pulse deviates from the norm for a long time, you need to visit a specialist.
The doctor will prescribe diagnosis and treatment. The most important thing is to reduce the likelihood of complications. To do this, you must follow your doctor's recommendations.
Why examine children
Usually, if a pathology of the cardiovascular system is suspected, doctors recommend an inpatient examination. This is very correct, since life depends on the work of the heart (namely, its marker is the pulse). It is very easy and dangerous to miss pathology. Hospitalization occurs in a specialized hospital on the direction of the attending doctor.
Such an examination is especially important for a child 11-12 years old, during puberty, when the pulse in its indicators approaches the norm of an adult and stabilizes. At this time, all systems of the child’s body are rebuilt, rapid hormonal correction begins, the emotional background and attitude to everything that surrounds the teenager changes.
It is at this age that the heart most often fails to cope with its work in the case of provoking factors (stress, bad habits, computer addiction). The child begins to talk about what worries him. It is important not to miss this moment.
Alarming symptoms do not yet have a real physical cause and do not cause irreversible organic changes. That is why an examination by specialists is needed to prevent further negative development of the scenario.
One of the most important points in diagnosis is correct and regular pulsometry performed by specialists.
When to see a doctor
If the pulse constantly deviates from the optimal value or various symptoms appear (chest pain, dizziness), it is recommended to visit a specialist for diagnosis. First you should contact a therapist - this is a general practitioner.
The specialist will conduct a survey, during which it is necessary to talk about the symptoms, if any. Next, important indicators are measured (pulse, blood pressure, temperature). Then the teenager's body is examined.
Next, the therapist can write a referral to another specialist, depending on the cause of the change in pulse. For example, if you suspect endocrine diseases, you should visit an endocrinologist.
After passing through all the specialists, a diagnosis is prescribed. For example, if a heart disease is suspected, a teenager may be referred for an electrocardiogram (ECG), 24-hour monitoring (Holter) and other procedures.
If a person’s well-being rapidly deteriorates or there are serious symptoms (fainting, severe heart pain), an ambulance should be called.
Prevention
{banner_banstat9}
For the proper development of the cardiovascular system, from childhood, parents must teach their child simple rules of behavior that guarantee the prevention of any diseases. These include:
- active lifestyle, fight against physical inactivity;
- playing sports according to age;
- hardening;
- balanced diet;
- morning exercises;
- walks in the open air;
- clothing according to the season and weather;
- refusal of large amounts of flour and sweets;
- calm and friendly atmosphere in the family;
- 8-9 hour sleep;
- correct indoor microclimate.
This lifestyle will help the baby grow up strong, courageous, balanced, and friendly, which will certainly affect the condition of the heart and blood vessels, and will guarantee a normal pulse in accordance with age.