Pathologies of the cardiovascular system are accompanied by pulse disturbances in 85-90% of cases. Spontaneous deviations in cardiac activity occur in 100% of situations, which indicates the absolute prevalence of dysfunctions of this kind.
The most obvious option for the patient himself is tachycardia (increased heart rate).
There are two types of this pathological condition:
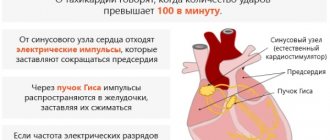
- Sinus form. It is represented by a disruption of the normal generation of an electrical impulse by the natural pacemaker (sinus node), located in the right atrium.
- Paroxysmal. It is determined by the formation of new, abnormal foci of activity. It occurs somewhat less frequently, flows more severely and is generally considered more life-threatening.
A pulse of 120 heart beats per minute is characteristic only of the sinus type; for the second, figures of 140 and higher are pathognomonic. This type of deviation does not pose any danger.
Does this mean that you can sit with your hands folded? No, definitely. On the one hand, over time, the acceleration of cardiac activity can progress, turning into something else: extrasystole, or ventricular fibrillation.
On the other hand, a pulse of 120-125 is almost always secondary and caused by other diseases. It is not known what we are talking about, therefore, fatal complications are quite likely.
Causes of pathology
A heart rate of 120 beats per minute is tachycardia. There are several reasons for its development. Most are transient in nature, and only a few are capable of creating a risk to human health and require emergency medical intervention.
Physiological
Temporary functional reasons that cause a rapid pulse include:
- unhealthy lifestyle: psycho-emotional overexcitation, stress - anything that can change the electrolyte balance of the myocardium (imbalance of potassium, sodium, calcium and magnesium) and increase the heart rate;
- excessive physical activity;
- pregnancy.
Pathological
Reasons that can cause organic changes in organs and tissues against the background of a pulse of 120-125 beats/minute at rest include:
- diseases of the heart, blood vessels, and other vital internal organs (ischemic heart disease, myocarditis, pulmonary embolism (PE), AMI, genetically determined syndromes, cardiomyopathies of various origins);
- tissue hypoxia or ischemia;
- diseases of the bronchopulmonary system;
- dehydration of various origins;
- uncontrolled use of drugs with intoxication;
- dysfunction of the thyroid gland (hyperthyroidism);
- VSD;
- obesity;
- diabetes;
- anemia of any etiology;
- hyperthermia (+ one degree increases the pulse by an average of 10 beats/minute).
Causes of elevated heart rate at rest
Development factors can be both cardiac and non-cardiac.
Problems with the muscle organ
- Arterial hypertension. Both symptomatic, caused, for example, by renal pathologies, and the disease itself, dysregulation of blood vessels and other varieties.
The essence is the same. The patient's blood pressure is steadily rising. Up to what numbers depends on a lot of factors. Including gender, age, condition of blood supply structures, duration of the process. Stages 2-3 lead to a stable increase in the pulse rate.
Recovery appears extremely difficult. Over time, the patient ceases to feel the negative effects of blood pressure at peak levels. The symptoms fade and the person gets used to the abnormal condition.
At the same time, a pulse of 120 beats per minute is not directly related to blood pressure. We are talking about indirect factors. The same etiological moment causes an increase in two vital indicators.
- Myocarditis. Inflammation of the muscle layer of the heart. It is she who is responsible for the functional state of the organ. It occurs relatively rarely, as a complication of third-party pathologies, such as rheumatism. Then we are talking about an autoimmune form or infectious conditions, respectively, we talk about viral, bacterial, fungal types.
Tachycardia accompanies the patient constantly, does not recede for a second, even at night. A resting pulse of 120 or more is a hallmark of myocarditis.
Recovery is carried out urgently in a hospital. Duration from several days to a week. Antibacterial therapy is used, and suppressors may be prescribed.
- Pericarditis. Or inflammation of the pericardial sac. There is a danger due to the likelihood of complications. Which ones? Tamponade as the main threat. This is compression of the muscular organ itself by accumulated effusion.
Urgent surgical intervention is required. Medication is indicated in the early stages, if there are no consequences yet.
- Heart defects. Congenital and acquired. They are found relatively rarely, especially if the state of health does not cause subjective concern. Many processes proceed gradually, for years, without pronounced symptoms from the body. Sometimes the diagnosis is made based on the results of the autopsy.
Tachycardia is a relatively rare occurrence in patients with anatomical defects. Recovery is possible, but at the right time. If you are late there will be nothing to help.
The main treatment is surgical. Contraction frequency is adjusted medically, after the fact, as a secondary measure.
- Atherosclerosis. Conditionally it can be classified as a cardiac pathology. In this case, the coronary arteries and aorta are affected.
Damage to the vessels supplying the myocardium can lead to a heart attack or an acute attack of angina with a heart rate of 120-140 beats per minute. Both options are dangerous. Accompanied by a persistent acceleration of the rhythm.
Another option results in left ventricular dilatation, aortic valve stenosis and decreased overall hemodynamics. Tachycardia occurs regularly, but does not last constantly.
Extracardiac pathologies
- Chronic obstructive pulmonary disease. Gives pronounced disturbances in pulmonary activity. First, the right ventricle suffers, then the entire muscular organ.
Bronchial asthma gives the same symptoms. Especially at the advanced stage of the condition. Recovery requires a lot of ingenuity, since the drugs themselves can provoke an increase in heart rate. This is true for glucocorticoids and bronchodilators, as well as other medications.
The difficulties are obvious, given the duration of therapy - a lifetime, it is necessary to select the optimal regimen. Relatively safe.
- Anemia. Usually iron deficiency. As a result of an insufficient amount of the element in the body, hemoglobin deficiency occurs. Stable anemia and tissue hypoxia occur.
The condition is relatively easy to treat. On the one hand, the root cause is eliminated. This includes constant minor bleeding or nutritional deficiency.
On the other hand, the infusion of iron supplements in a adjusted dosage is indicated. Which one you need to look at based on the severity of the condition.
- Hyperthyroidism. Or a disruption of the normal production of thyroid hormones. Recovery under the supervision of a specialized specialist. The causes of the condition are multiple: tumors, inflammation of an infectious or autoimmune nature, and other issues are possible.
Hormone replacement therapy is required. The duration is relatively short. In case of functional impairment, treatment is limited to this. There is no point in doing anything yet.
Tachycardia resolves on its own after removal of excess thyroid-specific substances.
- Infectious and inflammatory diseases. From colds, ARVI to tuberculosis and other dangerous conditions. A heartbeat of 120 beats per minute is the result of intoxication with waste products of the bacterial flora and excessive stimulation of the heart itself.
The main method for eliminating the pathological condition is to carry out specialized measures to evacuate harmful substances from the bloodstream.
It is most effective to take action in a hospital. If the disease is mild, the deviation goes away on its own.
- Cachexia. It is caused by nutritional disorders for objective reasons (inability to take care of oneself at home, inadequacy), or subjective factors. For example, with a complex known as dysmorphophobia - dissatisfaction with one’s own body. Both options are dangerous.
The first can potentially be stopped by the introduction of nutrient solutions. The second requires long-term work with a psychotherapist. Depletion leads to a stable utilization of one's own resources.
First, fat comes into play, then muscle. The body doesn't last long. The heart begins to fail, it lacks nutrition.
- Disorders of the nervous regulation of the cardiovascular system. Development options are different. From osteochondrosis and intervertebral hernias, to vertebrobasilar incompetence, tumors of cerebral structures and other issues.
Typically, sinus tachycardia with a pulse of 120-128 in a calm state lasts relatively short time. The episode lasts for about half an hour. Rarely more.
Subjective factors
A heart rate of 125-127 beats per minute develops as a result of cardiac and non-cardiac causes. But sometimes the factors are subjective, the patient is able to correct them himself.
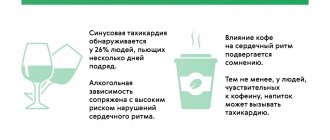
- Smoking. Secondary atherosclerosis occurs. It is caused by vasoconstriction as a result of prolonged consumption of nicotine. Pathological changes begin almost from the first cigarette. For some, progression occurs rapidly, for others it takes much longer, over the course of years. Alcohol habit. Alcohol has no beneficial effect on a person's life. Consuming ethanol is a destructive habit. All myths about benefits are nothing more than lies and misconceptions.
- Obesity. Body weight does not play a primary role. Overweight patients suffer from lipid metabolism disorders. The metabolic factor cannot be completely corrected. It is partly due to unfavorable genetics. Therefore, it is necessary to reconsider your diet. Pills alone won't help matters.
- Constant consumption of coffee and tea, energy drinks. These are psychoactive, although to a minimal extent, products. They tone blood vessels and cause stable stenosis (narrowing) of blood supply structures. They also do not provide any benefits to the body.
- Constant use of diuretics. Young women are guilty of this habit. This is extremely dangerous. Indeed, with the release of excess fluid, a kilogram or two is eliminated. But diuretics are not harmless drugs. In the short term they are planting buds. Recovery is almost impossible. It will only get worse. The only solution will be transplantation. The likelihood of successful treatment is slim.
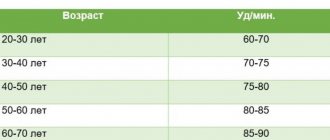
- Age. The older the patient, the higher the risk of developing stable tachycardia against the background of banal wear and tear of cardiac structures. It is necessary to treat the underlying disease that led to pathological changes.
The reasons are considered in the system and eliminated gradually. In the absence of evidence for organic phenomena, they speak of an idiopathic or natural form.
In the end, an acceleration of the pulse to 120 beats or even more is possible due to stress, emotional, and physical stress. All known factors are taken into account.
What is the danger?
A pulse of 120 beats/minute is characteristic of the sinus type, and in itself, existing for a limited time, does not pose a great danger. At the same time, on the one hand, over time, tachycardia creates a risk of transition to extrasystole, or ventricular fibrillation. On the other hand, it indicates the progression of some primary disease, for which fatal complications are quite likely. These dangerous consequences lead to:
- Congenital anomaly of the conduction system (the presence of additional branches of the conduction system of the heart, which duplicate the impulse, interfering with the full functioning of the myocardium, the full release of blood), which leads to brain hypoxia, fainting, and loss of consciousness.
- Acquired pathologies: hypertension, atherosclerosis, hyperthyroidism with the development of atrial fibrillation or ventricular fibrillation. The main danger is the formation of intracardiac blood clots, their separation, and ischemic stroke with a high risk of death.
You can minimize or prevent the danger using special techniques to lower your heart rate:
- periodic holding of breath to activate the vagus nerve, which can tame tachycardia;
- Valsalva maneuver: holding your breath with simultaneous abdominal tension - the essence is the same, activation of the vagus nerve;
- Aschner's test - pressing with fingers on closed eyes, the essence is the same;
These techniques can help slow your heart rate, but they are done either by a doctor, under the supervision of a doctor, or as prescribed by a doctor. Self-medication can lead to unpredictable consequences.
What do these indicators mean?
Usually nothing specific. It is possible to state a fact: heart rate acceleration. The pathological process is almost never primary.
It may be due to the onset of the disease or natural factors. If some third-party diagnosis is to blame, there are plenty of options. Not always cardiac abnormalities. Neurogenic processes and gland dysfunction are possible.
You need to figure it out together with your doctor. You should start with a cardiologist, then involve other specialists as necessary.
Sinus tachycardia, for which typical values are 100-130 maximum, is relatively difficult to tolerate, but the danger to life in the early stages is minimal.
In some cases, it is impossible to determine the cause of the condition even after a thorough examination. Then they talk about the idiopathic form of the increase in the indicator.
First aid
If your pulse begins to race, you need to calm down, drink cool water, lie down and take repeated measurements in about twenty minutes. Once your heart rate is normal, there is no cause for concern.
If dangerous symptoms are added to a pulse of 120 beats/minute: hyperthermia, abdominal pain, cardialgia, lightheadedness or fainting, you should call an ambulance. Before doctors arrive, you need to minimize movements and not take any medications. The exception is sedative drops: Valerian, Motherwort, Corvalol, Valocordin and Validol under the tongue. You should open the window and measure blood pressure.
If the cause of tachycardia is well known and attacks occur frequently, there is a drug regimen approved by the doctor, then you need to put Anaprilin under the tongue, take a Cordarone capsule or a Propanorm tablet. For high blood pressure - a common antihypertensive drug.
In all other cases, all medications are excluded before the doctors arrive.
Low blood pressure and high pulse - what does this mean?
Pulse is the frequency with which the ventricles of the heart contract per unit time. Blood pressure is a term used to refer to the volume of blood that moves through the heart during one beat.
When volume, that is, blood pressure, falls, the heart can compensate for this change by speeding up the heart rate, which is observed as an increased heart rate.
Unfortunately, this is not always so simple and only affects healthy people. In the case of patients, for example, with atherosclerosis of arterial vessels, hypertension, anemia and many other diseases, the relationship between pulse and blood pressure is disrupted.
When do you need to call an ambulance?
If the pulse rate of 120-125 beats/minute does not go away within half an hour, you should immediately seek medical help. In addition to tachycardia, the patient may be concerned about:
- chest pain of a pressing or burning nature, of moderate intensity (if this lasts more than half an hour, it is a sign of a developing heart attack);
- shortness of breath, which indicates either increasing heart failure (with complete rest) or impaired gas exchange due to pulmonary pathology;
- cyanosis of the nasolabial triangle against the background of unnatural pallor of the skin;
- a heart rhythm disturbance (extrasystole or fibrillation) can develop in parallel with a rapid heartbeat, with a characteristic feeling of a freezing heart;
- cold, profuse, sticky sweat is a consequence of vegetative-vascular disorders;
- headaches of different nature and genesis are the result of ischemia and hypoxia of brain structures;
- dizziness, sometimes of an orthostatic nature against the background of low blood pressure, loss of orientation in space with a forced lying position;
- increasing ringing in the ears;
- syncope, presyncope and fainting are one of the worst prognostic signs that indicate persistent progressive cerebral ischemia resulting in stroke;
- fear, panic attacks or complete apathy require immediate correction.
Such symptoms are treated only inpatiently and only by qualified specialists. In some cases, time passes by minutes.
Tests needed to identify the root cause
Under the supervision of a cardiologist. The approximate list of events is quite wide:
- Oral questioning of the patient and collection of anamnesis. Aimed at objectifying symptoms and identifying the clinical picture.
- Next, measure blood pressure and heart rate. Statement of the fact of deviation from the norm.
- 24-hour Holter monitoring. Registration of the same indicators for 24 hours. Makes it possible to assess the situation in dynamics, in natural conditions for the patient.
- Electrocardiography. Shows the functional state of the cardiovascular system. Can be prescribed after exercise (bicycle ergometry).
- Echocardiography. Ultrasound technique for tissue visualization. All defects become clearly visible.
If necessary, cardiac tomography and coronography are indicated. It is possible to prescribe vascular Doppler ultrasound (USDG).
A cardiologist does not always cope alone. When the origin of the pathological process is complex, third-party doctors are involved. It is possible to convene a whole council, based on the complexity of the case.
Features of treatment
Therapy for a pulse of 120 beats/minute is usually medicinal. Drugs of different pharmacological groups are used:
- cardiac glycosides: Strophanthin, Korglykon, Digoxin, Celanide - improve myocardial contractility, but are used with great caution, minimal doses and short courses, since they have the ability to accumulate, causing sudden cardiac arrest;
- beta blockers: Betaloc, Concor, Metoprolol, Carvedilol according to indications;
- antiarrhythmics: Anaprilin, Amiodarone - in small courses;
- antihypertensive drugs: Renitek, Ko-Renitek, Norvasc, Enap, Amlodipine - for high blood pressure with a tendency to further increase;
- sedatives: Novo-Passit, Persen, Afobazol - to stabilize the psycho-emotional background.
Surgery with a pulse of 120-125 beats/minute is carried out according to vital indications: heart defects - congenital and acquired, total atherosclerosis requiring balloon angioplasty, stenosis with stenting. It is possible to ablate (cauterize) the focus of pathological myocardial activity with radio waves or install a pacemaker (pacemaker).
In all cases, the heart rate is 120 beats/minute, a priori a change in lifestyle is assumed: giving up alcohol, cigarettes, a balanced diet with salt limited to 5-7 grams/day, dosed physical activity.
With sinus tachycardia 120 beats/minute, using folk remedies is pointless and even dangerous due to the risk of complications (dosage inaccuracy).