What kind of disease is this and what are its causes?
The main etiological cause of the development of acute myocardial infarction is atherosclerotic damage to the intima (inner lining) of the coronary arteries.
As a result of the formation of deposits, the lumen of the vessel narrows, and blood begins to flow in limited quantities. This is how IHD begins with angina attacks. When exposed to provoking factors (physical or emotional stress), the artery is completely blocked and permanent ischemia develops with the formation of an area of necrosis. Other (very rare) causes of heart attack are conditions in which blood flow is disrupted:
- rheumatism;
- vasculitis;
- tumors;
- allergy;
During my practice, I often encountered the fact that many patients do not eliminate bad habits and poor nutrition from their lifestyle. But these risk factors for myocardial infarction often lead to fatal consequences.
Deterioration of the blood supply to the heart occurs more often in the elderly: men after 45 years of age and women after 55 years of age should beware of the disease. Psycho-emotional shocks can provoke an attack - many patients come to our department after the death of loved ones, dismissal from work, divorce.
Factors provoking myocardial infarction
Myocardial infarction
There are various reasons for the development of the pathological condition:
- Diabetes. The formation and increase in atherosclerotic plaques occurs more intensely in people suffering from diabetes. This disease is characterized by vascular fragility and metabolic disorders. Atherosclerotic plaques and blood clots more often occur on vulnerable vessel walls.
- Hypertonic disease. High blood pressure causes the walls of blood vessels to thicken. They become dense and lose elasticity. During exercise, altered blood vessels cannot meet the heart's increased need for oxygen.
- Heredity. The tendency to develop hypertension, atherosclerosis and thrombosis can be inherited.
- Floor. Heart attacks occur 4 times more often in men than in women.
- Age. Young people are less likely to develop atherosclerosis and extensive myocardial infarction.
- Tobacco smoking. After inhaling tobacco smoke, a sharp narrowing of blood vessels occurs.
- Lack of movement. In people who lead a sedentary lifestyle, the walls of blood vessels lose their elasticity.
- Obesity. Excess weight creates additional stress on the cardiovascular system
- Alcohol abuse. Alcohol causes dysfunction of the liver, which is responsible for breaking down fats. As a result, fat accumulates in the blood and is deposited on the walls of blood vessels.
- Kidney disorders. In renal failure, the exchange of phosphorus and calcium is disrupted. As a result, calcium is deposited on the walls of blood vessels and thrombosis develops. Many of those suffering from kidney disease have experienced a massive heart attack.
- Stress. Severe psycho-emotional shock or frequently occurring stressful situations can cause a critical narrowing of the lumen of blood vessels.
- Hyperlipidemia. Abnormally elevated levels of lipids and lipoproteins in the blood are a provoking factor for the development of extensive myocardial infarction.
- Excessive physical activity. High myocardial oxygen demand, insufficient elasticity of blood vessels and their spasms can lead to the development of a heart attack during intense sports.
- Trauma or surgery. Pathological narrowing of the lumen of the coronary vessels can occur as a result of injury or surgery.
Classification
Classification of myocardial infarction is carried out according to several principles.
Based on the time of occurrence, they are distinguished:
- first appeared (primary);
- recurrent (repeated within 1.5 months after the first);
- repeated (occurring later than 6 weeks after the primary).
The following types of myocardial infarction are determined by location:
- left ventricle (anterior, posterior, lateral and septal walls);
- extensive, affecting several departments at once;
- right ventricle (occurs extremely rarely, often accompanied by damage to other areas of the heart muscle).
According to the degree of prevalence of ischemia and necrosis, there are the following types of acute myocardial infarction:
- intramural (located deep in the wall of the organ);
- subendocardial (develops in the inner layer);
- transmural (passes through all three layers of the heart);
- subepicardial (disorder in the outer part of the organ).
Diagnosis of heart attack
Ultrasound examination of the heart
Extensive myocardial infarction is diagnosed based on the following points:
- Patient complaints
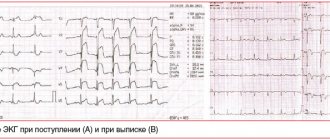
- ECG study in dynamics
- Ultrasound examination of the heart
- Laboratory detection of elevated levels of myocardial enzymes, monitoring them over time
- Coronary angiography according to indications
- Transmural myocardial infarction: what it is, dangers and treatment
How many heart attacks can a person have?
Almost all patients who have had a heart attack once ask me about the risk of another at their appointment. Understanding their concerns very well, I will still say that no specialist will give a definite answer in this case. It is necessary to take into account the location of the scar, the depth and width of the lesion, and the presence of complications. The degree of restoration of cardiac function depends on the development of collateral circulation (additional vascular pathways). I have seen cases where the patient remained alive after the fifth episode, although death can also occur as a result of a primary heart attack.
Prevention of heart attack
Prevention of heart attack is based on reducing modifiable risk factors for coronary heart disease. Changing lifestyle, receiving timely medical care and taking prescribed medications for concomitant diseases (diabetes, hypertension, chronic kidney disease, peripheral arterial disease, high cholesterol), proper nutrition, normalizing weight, regular exercise, giving up bad habits will help prevent heart disease attack (including repeated).
Stages of disease development
The clinical course of a heart attack goes through five main periods:
- Subromal or pre-infarction. It can be short (up to several hours or days) or quite long (1-2 weeks or a month). At this time, pain attacks become more frequent and prolonged. The same option includes a heart attack, which manifests itself against the background of sudden and rapidly progressing angina.
- The sharpest. Consists of persistent ischemia followed by the development of necrosis. Lasts from 20-30 minutes to 2 hours (but no more). Anginal pain by this time becomes weaker or completely disappears. Blood pressure drops, signs of heart failure appear or increase.
- Spicy. Necrosis smoothly progresses into melting of the heart tissue (can last from two days to two weeks).
- Subacute (from 1 to 45 days from the onset of the episode). At this stage, the formation of connective tissue in the affected area begins, and the remaining myocardiocytes adapt to continue further work.
- Post-infarction. The scar is completely organized, granulations appear at the site of necrosis. It takes from the beginning of the acute stage from 1.5 months to six months.
I would like to draw your attention to the fact that the provision of qualified assistance during the deterioration of angina pectoris or during the acute period of myocardial infarction helps prevent the development of necrosis. In this case, the process is reversible and the prognosis is favorable.
Read more about what happens and how to act correctly at each of the above stages of a heart attack here.
Consequences of a heart attack
After a severe heart attack, complications are often recorded. The main consequences of a major heart attack in men and women are as follows:
- heart block;
- pulmonary edema (acute heart failure);
- blood clot formation;
- recurrence of heart attack;
- pericarditis;
- there is a danger of mental disorders;
- disorders of blood circulation in the brain;
- malfunctions of the digestive system;
- heartbreak;
- failure of internal organs;
- Paralysis of the limbs may occur.
How long do they live after a heart attack?
Many people who have suffered a heart attack and their relatives are always interested in how long they live after a major myocardial infarction. Life expectancy depends on the quality and quantity of the consequences of the blow, the size of the lesion of the heart muscle, and the age of the patient. To prolong your life as fully as possible after a heart attack, you need to take prescribed medications, lead a healthy lifestyle, and follow all medical recommendations. According to statistics, about 20% of patients live up to 5 years after a major attack.
Early signs of a heart attack
Most of the patients (approximately 60 to 80%) who were observed by me with this diagnosis indicate that the disease did not begin suddenly in them. It was preceded by precursors of a heart attack, or a prodromal period. The most favorable outcome was observed in those patients who sought help or were brought by the team in the first hours of the attack.
I would like to make a small disclaimer - early signs of myocardial infarction do not always occur, it all depends on the pain threshold and the state of the patient’s nervous system.
But in most cases I have seen the following symptoms:
- Pain along the anterior surface of the chest radiating to the left arm, part of the lower jaw, and scapula.
- The unpleasant sensation is not relieved by taking nitro-containing drugs and goes away only after the administration of narcotic analgesics.
- It has a constant, increasing or wave-like character with periods of subsidence and resumption.
- Lasts more than 20-30 minutes.
- The patient begins to sweat and tries to sit down or lie down as high as possible. This position makes the attack a little easier.
- Shortness of breath develops, the skin becomes pale, and the nasolabial triangle turns blue.
- When it comes to the first signs of myocardial infarction, rhythm disturbances cannot be ignored. According to my observations, they are observed in 90% of cases at the stage of ischemia development and before scar formation.
Any suspicion of a heart attack requires an immediate ECG, which will reveal all signs of ischemia, and at a later stage, necrosis and scar formation. Read more about what changes will be visible on film here.
Causes
The most common cause of myocardial infarction is long-term atherosclerotic damage to the walls of blood vessels (narrowing of the lumen of the arteries due to the deposition of atherosclerotic plaques consisting of cholesterol and lipoproteins on their walls), which provokes insufficiency of blood supply to the myocardium. A heart attack can cause vascular thrombosis; prolonged spasm of the coronary artery (not affected by atherosclerosis), associated with taking drugs, stress, painful shock, exposure to cold, smoking; lack of oxygen in the blood (hypoxia); heart disease; blockage of an artery during surgery.
Consequences and complications
In any period from the onset of an acute infarction to its resolution in the form of the formation of a connective tissue scar, the following complications may be observed:
- cardiogenic shock;
- heart failure;
- ventricular fibrillation;
- wall rupture due to myomalacia;
- formation of a parietal thrombus and thromboembolism;
- pericarditis.
The lethal outcome of this disease is recorded in the early stages in approximately 35% of cases. Its cause is rhythm disturbance, cardiogenic shock and acute heart failure. Later death may occur as a result of the formation of an aneurysm with rupture, thromboembolic complications, or acute pericardial tamponade.
After the acute period, the heart muscle adapts to new working conditions, but there remains a high risk of repeated episodes.
Features and advantages of treatment of myocardial infarction at the Rassvet clinic
Dawn cardiologists are engaged in primary and secondary prevention of cardiovascular diseases, including myocardial infarction.
Our clinic is equipped with modern equipment for diagnosing heart disease and identifying increased risk of cardiovascular pathologies, including digital electrocardiographs, digital X-rays, high-end ultrasound and echocardiography. For patients diagnosed with CVD, our doctors develop secondary prevention measures aimed at preventing complications and relapse of the disease. Cardiovascular pathologies are treated according to the protocols of European and American Heart Associations with proven effective drugs.
Author:
Amelicheva Alena Aleksandrovna medical editor
Treatment
Treatment of myocardial infarction should be carried out in an intensive care unit with qualified personnel and special equipment. But assistance should begin at the prehospital stage.
This is usually done by the ambulance crew.
After taking an ECG and establishing a presumptive diagnosis, you should:
- put a Nitroglycerin tablet under your tongue;
- give 300 mg of Aspirin to drink;
- administer narcotic analgesics to eliminate pain;
- if necessary, use intravenous antiarrhythmic drugs;
- carry out resuscitation measures in case of cardiac arrest and clinical death.
Read more about how to properly provide emergency care to a patient with a heart attack here.
Drug therapy
After the patient is admitted, my colleagues and I provide care according to the established protocol. All measures are aimed at relieving pain, limiting the area of necrosis, preventing the development of complications, and restoring blood flow through the coronary arteries.
Treatment of myocardial infarction begins with the elimination of pain. Since conventional drugs are ineffective in this case, doctors use intravenous administration of the narcotic analgesics Promedol or Morphine. This helps normalize a person’s emotional state, lower the heart rate and equalize blood pressure. When discomfort is relieved, the likelihood of reflex cardiogenic shock decreases.
Acute myocardial infarction is a coronary thrombosis. Therefore, the patient is administered a direct anticoagulant, thereby performing the procedure of thrombolysis - dissolving the blood clot.
The modern and most effective approach is considered to be a stenting procedure, which allows you to instantly restore blood flow in the affected heart vessel. After this, Clopidogrel with Acetylsalicylic acid is prescribed for 2 years to prevent platelet aggregation and the development of a recurrent attack.
The use of beta blockers can reduce the load on the heart and also prevent the development of arrhythmia. Treatment of myocardial infarction necessarily includes prolonged nitrates (“Kardiket”). They allow, by dilating the coronary vessels, to improve blood flow to the heart and limit the area of necrosis.
An important point is the prescription of high doses of statins (“Rosuvastatin” up to 40 mg, “Atorvastatin” up to 80 mg) - drugs. Their use can reduce the degree of inflammatory reaction.
Symptoms of myocardial infarction and their characteristics are also taken into account during treatment. In case of severe anxiety, the patient is given sedatives; if the pressure remains high, antihypertensive drugs are used.
I would like to note that treatment after a heart attack does not end. The patient will need to take blood thinners and cholesterol-lowering drugs (statins) throughout his life. Read about how to properly undergo rehabilitation after an attack here.
Surgical methods
In the absence of treatment effectiveness and in order to prevent the recurrence of a heart attack in the same area, the following operations are used:
- Coronary artery bypass grafting. It consists of restoring the passage of blood through the heart arteries by creating an artificial anastomosis.
- Balloon angioplasty. A tube with a ball at the end is inserted into the lumen of the vessel. Having reached the point of application, it is inflated and the atherosclerotic plaque is pressed against the wall, restoring normal blood flow.
Only in hospital
Acute coronary syndrome is a collective concept that includes unstable angina and acute myocardial infarction. The treatment strategy for this condition is to quickly restore blood flow, which saves the myocardium and the life of the patient. And such assistance can only be provided in a hospital or vascular center, provided that the patient is delivered within two hours from the moment the vessel is blocked. Statistics confirm this: mortality in hospitals from myocardial infarction is 13–14%, in vascular centers – even lower.
Correct routing of patients and stenting are a real opportunity to reduce mortality from heart attacks, Maria Glezer emphasized. According to her, the introduction of a system of vascular centers made it possible to reduce hospital mortality from acute heart attack in the Moscow region by 60% - an impressive figure. But the problem is that people don't call an ambulance. 40–50% of patients die at home, Maria Glezer laments: “When I ask why they were sitting at home, they answer: they thought it would go away on its own, it would resolve.” So one of the main tasks is the education of the population.
Repeated myocardial infarction is a real threat. It ranges from 10 to 20%. It is very important for people who have suffered it to be told about secondary prevention measures that can prevent rhythm disturbances and the development of such a serious pathology as heart failure, which often leads to death, says Professor Glezer.
“If the patient is lucky and survives the first time, he will not necessarily survive the second or third time,” warns the deputy director for scientific work of the medical research and educational center of Moscow State University. Lomonosov, member of the Presidium of the Russian Cardiological Society, corresponding member of the Russian Academy of Sciences, Professor Simon Matskeplishvili . “But, unfortunately, it very often happens that doctors did everything in their power to save the patient’s life: they performed primary coronary intervention, placed a stent and eliminated the cause of acute coronary syndrome or treated it conservatively. And upon discharge, they gave instructions that were designed to preserve the life and health of the patient. But, after being discharged from the hospital, he goes to the clinic, where his treatment is completely changed.”
It often happens that patients take their own medications off, and instead of really effective drugs prescribed in the hospital, they ask the doctor at the clinic to prescribe drugs from a very limited list of subsidized medications. Or worse, they switch to dietary supplements.
Heart attack is inherited. Why the heart stops in young people Read more
Clinical case
A patient was admitted to the hospital with severe chest pain and other typical symptoms of myocardial infarction.
He was sent from the clinic, where a cardiogram was taken, which revealed large-focal necrosis in the acute stage of development along the anterior wall of the left ventricle. He notes that lately there have been warning signs of a heart attack - angina attacks became stronger and were poorly controlled with Nitroglycerin. The patient was referred for percutaneous coronary intervention—stenting. On the second day after the procedure, the patient felt much better, and therefore he was transferred to the general cardiology department. Recommendations were issued: follow a diet with limited fluid and salt, as well as the exclusion of fatty foods and foods high in cholesterol, lifelong use of Aspirin and statins, adequate physical rehabilitation.
Risk of heart attack and effectiveness of coronary stenting
A few words about acute myocardial infarction
Acute myocardial infarction is necrosis, that is, death of a section of the heart muscle, developing as a result of a sudden, acute disturbance of blood flow in the coronary (cardiac) artery system. Blockage of a branch of the coronary artery can be caused by its thrombosis, less commonly by embolism or prolonged persistent spasm.
The most common cause of heart attack is atherosclerosis
Atherosclerosis is a disease when atherosclerotic plaques form on the walls of blood vessels, which narrow the lumen of the coronary arteries and also contribute to the destruction of their walls, which provokes the formation of blood clots and blockage.
What does a heart attack lead to?
An acute heart attack causes irreversible changes in the heart muscle: the death of part of the functional muscle cells of the heart (necrosis) and their subsequent replacement with connective tissue, that is, the formation of a post-infarction scar. The scar on the myocardium remains for life. It cannot resolve, and the heart always remembers the heart attack. Subsequently, disruption of the blood supply to the myocardium can lead to cardiac dysfunction: heart failure develops, that is, the heart does not perform its functions fully. Thus, for the full existence of the entire organism there is simply not enough “power”.
In simple terms, due to an acute circulatory disorder, the heart gradually begins to “die”, and in order to save a person’s life, it is necessary to restore blood circulation as soon as possible. If medical care is not provided in a timely manner, a person with a heart attack may die within the first 24 hours. In general, the prognosis of the outcome of a heart attack depends on the size of the myocardial lesion, the severity of the course, the age of the patient, and the development of complications. But in any case, the prognosis of the disease is influenced by the timeliness of the start of treatment and its adequacy.
In Kyrgyzstan, this disease remains one of the main causes of premature death. For a long time, the treatment of acute infarction in our area was far from the most advanced strategy. According to indications, thrombolytic therapy was carried out, that is, the administration of drugs that resolve the blood clot and restore the patency of the vessel. Such assistance was provided both by emergency medical teams before hospitalization and in intensive care units of hospitals. The success of treatment often depended on the correct choice of drug and the timely start of its use. Of course, there was no talk of the high effectiveness of drug therapy: a very high percentage of deaths (about 16−20%), and if a person remained alive, he became disabled, his heart could not work properly.
Coronary stenting
Coronary stenting is the most effective way to treat acute myocardial infarction due to the complete elimination of circulatory disorders through direct and immediate impact on the infarction.
The essence of the method
The essence of the method is to install a special stent into the affected vessel through the radial artery (on the wrist) in order to restore blood flow.
A stent is a metal mesh structure that resembles a hollow tube of small diameter. Using a special balloon, a folded stent is inserted into the artery, under the control of an X-ray machine, it is delivered to the site of narrowing of the vessel, then, when the balloon is inflated under pressure, it is expanded and implanted, expanding and supporting the affected vessel in the area of blockage or critical narrowing and restoring blood flow. Also, in order to make the intervention most effective and safe, a wide range of special drugs are used.
Benefits of stenting
The advantages are that this operation is low-traumatic, practically painless, has a small number of complications, reduces the length of hospital stay from 15-17 to 7-11 days, makes it possible for the patient to become active early and refer him for rehabilitation in a sanatorium-resort setting.
Thanks to stenting in acute myocardial infarction, mortality has decreased by almost half, and today it is about 6%. But the most important thing is that after a heart attack the patient can return to a normal, fulfilling life, to his work.
When is stenting effective?
During a heart attack, approximately half the thickness of the heart muscle dies in the first three hours; in the next three hours, the entire thickness of the muscle dies. Therefore, stenting in the acute period of myocardial infarction is effective if it is performed as early as possible, no later than the first 6 hours from the onset of the infarction, optimally - up to 2-3 hours. Restoring blood flow in a clogged artery in this time period, before the development of irreversible changes in the myocardium, sharply reduces the area of the infarction, and sometimes makes it possible to “interrupt” its development.
How not to “live to have a heart attack”
There are major risk factors that can lead to the development of myocardial infarction. We can influence some of them, but not others. You cannot influence, for example, gender (men are more susceptible to coronary heart disease), age, family history, or hereditary predisposition. However, we can significantly reduce the adverse effects of factors such as arterial hypertension, smoking, diabetes, high cholesterol, excess weight, and a sedentary lifestyle. All these factors, both in combination and each independently, provoke the development of atherosclerosis, which, as I have already said, is the main cause of myocardial infarction.
Prevention of myocardial infarction
The number of patients in whom a heart attack is not associated with atherosclerosis, but is most likely caused by a sharp spasm of the coronary artery against the background of severe stress or a large loss of fluid and, as a consequence, thickening of the blood and the formation of a blood clot, is very, very small in the study group.
People think little about their health, they ignore alarming symptoms due to an irresponsible attitude towards themselves or out of ignorance, although there is enough necessary information in the media and on the Internet, there are very good social advertising videos. But citizens simply do not pay attention to this.
Today, medical capabilities make it possible to save the lives of patients even with severe heart attacks. But not only doctors, but also ordinary people should be wary in this regard. Without this, no technology will help.
Give up bad habits and “fast food”, add more physical activity to your life, devote at least 30 minutes a day to physical exercise and walking in the fresh air. Also, do not skip medical examinations and consult a doctor on time.
How to choose a stent?
The choice of a stent is up to the doctor who will install it. However, the patient may be offered an alternative between a plain stent and a drug-eluting stent. If the doctor, due to the patient’s characteristics of atherosclerotic lesions, advises using a covered stent, this is worth listening to. But in some cases, you can get by with a simple stent when a more expensive covered stent is not necessary. The main thing is to be sure that you are consulting on this matter with a highly qualified specialist with extensive experience in intravascular operations, since only he can take into account all the features of your condition, the influence of concomitant diseases, and the tolerability of medications that are necessary after stenting. If you suspect that your doctor is choosing a stent based on other considerations, such as the cost of the stents, you may want to consult with another specialist. Therefore, the patient’s problem is the choice of a competent and responsible doctor, and not the method of treatment. If necessary, BOSTI is ready to help with this.
What is the main reason why experts recommend the use of drug-eluting stents?
It is known that in some cases (with severe types of vascular lesions, concomitant diabetes mellitus, etc.) the likelihood of developing restenosis, that is, repeated stenosis developing inside a simple metal stent, is quite high. In such cases, drug-eluting stents are used. However, it should be borne in mind that after the installation of covered stents, the requirements for taking antiplatelet drugs are much stricter, and the duration of their course is longer - until the release of the drug from the surface of the stent ends (12 months). If these requirements are not followed, conditions may be created for stent thrombosis throughout this time, and this is a very dangerous complication.
Dr. BOSTI recommends high-quality stents from the German company BIOTRONIK
The German company BIOTRONIK is a world leader in the production of coronary stents, introducing innovative and high-tech methods of diagnosis and treatment. In 2015, the highest level in this area was achieved - they put the Magmaris bioabsorbable stent into production and implantation. This stent consists of a magnesium alloy, which is not foreign to the human body. Magmaris gradually dissolves inside the vessel; after 12 months it is almost completely dissolved (95%), this time is enough for us to “heal” the place of narrowing and/or occlusion. And in terms of its parameters (patency, deliverability, flexibility, strength and efficiency), Magmaris is in no way inferior to conventional stents.
1) Orsiro drug-eluting stent from Biotronik containing a biodegradable polymer
The advanced crimping technique gives the stent a very small cross-section (0.99 mm/0.039″) and ensures stable retention of the stent on the balloon without damaging the BIOlute® coating.
- Thanks to our state-of-the-art balloon technology, delivery of the stent to the lesion site is effortless and easy. The shaft with the Enhanced Impact Transmission (EFT) system gives this high-quality device greater ability to move, also through tortuous vessels.
- The Orsiro stent system is based on PRO-Kinetic Energy, our sixth generation metal stent. The stent material is a cobalt-chromium alloy, which makes the ribs of the structure thinner while maintaining optimal radial strength and radiopacity. The diameter of the thin ribs of the stent is only 60 microns, which provides exceptional flexibility and ease of movement to the installation site - even in the most complex vessels.
A unique solution for the treatment of coronary artery stenosis, a hybrid design with a combination of passive and active components.
Passive component:
Passive PROBIO® coating covers the stent frame and eliminates interaction between the metal parts of the stent and surrounding tissues.
Active ingredient:
BIOlute® is a polymer matrix that is absorbable in the body and releases a drug from the limus group in a controlled manner. Over time, only the PROBIO® covered stent remains in the patient's body.
2) Magmaris scaffold
The Swiss Magmaris scaffold is recognized as a physiological and high-quality scaffold - its wall thickness is 150 microns.
The surgeon performs the entire operation under local anesthesia, through a small puncture in the artery on the thigh or arm.
When straightened, the scaffold restores normal blood flow in the vessel and prevents its walls from closing again. Oxygen and nutrients begin to flow to the affected area of the heart muscle - the development of a heart attack stops.
You can purchase high-quality coronary stents Orsiro, Magmaris. They are also available for order throughout Kyrgyzstan.
You can find detailed information about them on our website, as well as
consult
about treatment with BOSTI - call or write to the following.
numbers: 0555 71 08 85 0555 71 08 18 0551 71 77 13