When a man and a woman are just starting to build a relationship, they are unlikely to be interested in each other’s blood type, much less its compatibility. And only when a couple thinks about having a child does this question become relevant. Most often, spouses are tested for groups and Rh factor when the woman is already pregnant. Ideally, undergo a comprehensive examination, including a blood compatibility test upon conception, at the stage of pregnancy planning.
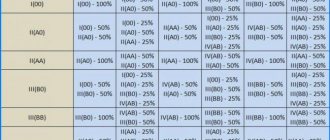
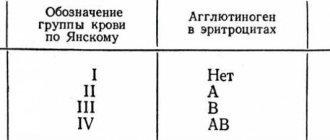
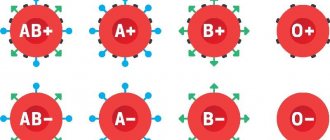
As you know, humans have four types of blood according to their blood group and two according to their Rh factor. The first group is 0 (I), the second is A (II), the third is B (III) and the fourth is AB (IV). In addition, blood can be Rh positive (Rh+) and Rh negative (Rh-).
Blood and Rh compatibility
Doctors say that, as such, blood group incompatibility does not exist. There may be immunological, genetic, HLA incompatibility between spouses, as well as the production of antibodies to the man’s sperm. In this regard, conception may not occur, pregnancies end in miscarriages, the child is born non-viable or dies in the mother’s womb.
As for the blood type of future parents, it has practically no significance when planning pregnancy and does not affect the conception, gestation and birth of offspring.
The situation is different with the Rh factor. In this case, incompatibility of partners with different Rh is possible. As a rule, there are no problems with conception, but there is a possibility of Rh conflict between the woman and the unborn child.
Let’s understand the terms: what is “Rh factor” and “Rh conflict”?
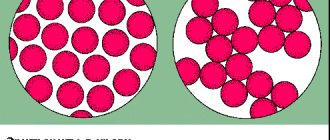
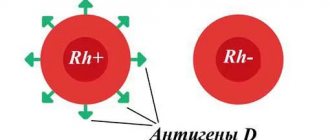
The Rh factor (Rh factor) of a person depends on the presence of D antigens on the membranes of red blood cells. If these antigens are present, then the blood is Rh positive (Rh+); if not, it is negative (Rh-). The vast majority of people are carriers of D antigens, and only 15% of the world's population do not have them.
The Rh factor is a genetic trait that is inherited and remains with a person for life. This feature cannot be changed by any means. Blood Rh does not affect a person’s well-being and health and becomes important in two cases:
- during a blood transfusion;
- during gestation.
Rh conflict (Rh sensitization) during pregnancy is a pronounced immune reaction of the female body to the blood of the fetus. An immune reaction can only occur if the pregnant woman is Rh-, her partner is Rh+, and the child has inherited the father’s Rh-ness.
With any other variants, Rh sensitization cannot appear ⇩⇩⇩
In the fetus, Rh begins to form from 6–8 weeks of gestation. If after this period there is contact between the red blood cells of the mother and the fetus, the pregnant woman’s body will begin to produce antibodies. This process is called sensitization: the female body perceives the fetal red blood cells as “enemies” and turns on immune defense against them. Rh conflict is in many ways reminiscent of an allergic reaction, when the immune system sees a threat in substances that pose no danger to the body.
Maternal antibodies, which are synthesized during Rh conflict, are able to “attack” the red blood cells of the fetus, causing their massive hemolysis (destruction). This leads to the release of indirect bilirubin, a toxic substance that damages fetal tissue.
Due to the danger of Rh conflict, all couples planning a pregnancy are advised to take a blood group and Rh factor test . This simple procedure will not take much time, but will give you valuable information about possible problems after conception. The study is performed in any diagnostic laboratory.
When can Rh conflict occur?
It is possible only in one case - if the mother’s Rh factor is negative, the father’s is positive, and the fetus has inherited the father’s Rh factor.
The conflict arises due to the incompatibility of the mother's Rh-negative blood and the red blood cells of the unborn child, on the membranes of which there is a specific protein. When fetal red blood cells enter a woman’s bloodstream, her body perceives them as foreign and begins to produce antibodies against them.
As a rule, during the first pregnancy the amount of antibodies in the blood is small, so they do not affect the developing fetus. In addition, during the first pregnancy, the red blood cells of the unborn baby should not normally enter the mother’s blood, since this is prevented by the blood-placental barrier. Fetal blood enters a woman's bloodstream only during natural childbirth or during a caesarean section.
However, in some cases, it is possible for fetal red blood cells to reach the mother, including:
- Abortion.
- Ectopic pregnancy.
- Miscarriage.
- Taking amniotic fluid for analysis to diagnose fetal pathologies.
- Chorionic villus biopsy is the taking of its villi for analysis to diagnose fetal diseases.
- Bleeding during pregnancy.
- Rh+ blood transfusion.
When a child’s red blood cells come into contact with the mother’s blood, her body begins the process of producing Rh antibodies, which is called sensitization. If none of this has happened to a woman, most likely there will be no conflict during her first pregnancy, and the contact between the blood of mother and child, which occurs during the first birth, does not affect the health of the latter in any way. But if sensitization occurred for the above reasons or during the first birth, then this is irreversible. In subsequent pregnancies, treatment is necessary to prevent Rh conflict.
What are the reasons for the incompatibility?
This type of infertility can be caused by:
- autoimmune diseases (a situation where your own immunity begins to fight the body);
- marriages between close relatives;
- genetic disorders;
- presence of antisperm bodies.
If there is genetic incompatibility during the division of the nuclei of sperm and eggs, there is a high risk of the appearance of cells with an incorrect set of chromosomes. Genetic incompatibility occurs due to:
- incest (marriages between close relatives);
- hereditary pathologies;
- strong dose of radiation;
- poor environmental situation.
With age, the risk of chromosomal mutations in women increases, especially after 40 years.
Why is Rh conflict dangerous?
Antibodies that are produced to foreign proteins upon contact between the blood of a woman and the fetus destroy the red blood cells of the unborn child. He develops anemia and also increases bilirubin levels, which usually occurs when red blood cells break down. Bilirubin is toxic and has a negative effect on the brain. The bone marrow of the unborn baby cannot cope with the production of new red blood cells; the spleen and liver are involved in the process. As a result, they increase in size, and this leads to an increase in pressure in the veins, swelling of the subcutaneous fat and other tissues. Such disturbances in fetal development are called hemolytic disease, which can lead to brain pathologies and even intrauterine death. Thus, Rh conflict has the following consequences for the child:
- swelling (dropsy);
- jaundice;
- hypoxia;
- anemia;
- mental retardation;
- intrauterine death.
For the health of the mother, Rh conflict does not pose a danger and manifests itself as an allergic reaction.
Ways to deal with incompatibility
If immune infertility is diagnosed, lymphocytoimmunotherapy can be performed, which is combined with taking hormones. The main goal of treatment is to change the mother's immune response to the embryo.
When antisperm bodies are detected, therapy involves sexual activity using barrier contraception for the time prescribed by the doctor. In parallel, immunotherapy with allergens is prescribed.
In case of genetic incompatibility, the use of ART is indicated.
Treatment
Thanks to medical advances, even Rhesus-incompatible spouses can produce healthy children.
At the first visit to the antenatal clinic, the pregnant woman is immediately sent for a blood test for the Rh factor. If the expectant mother is Rh negative, the future father must also donate blood. If he is Rh negative, then the conflict will not occur, but if he is positive, special monitoring of the woman and the developing fetus is required, since it can inherit the father’s blood. The expectant mother will have to periodically donate blood for Rh antibodies. If their production has begun, special treatment is required. If sensitization is detected in time and timely therapy is started, the child will be born healthy.
First, the doctor constantly checks the condition of the unborn child in order to detect symptoms of Rh conflict. If signs appear, treatment will depend on their severity. The main thing is to support the vital activity of the fetus, which is to combat oxygen starvation and developmental delays. It is important to increase the level of red blood cells in the blood, which may require intrauterine blood transfusion through the umbilical cord vein under ultrasound guidance. But more often a blood transfusion is given to a child after birth. Sometimes this even requires early birth.
If no antibodies are detected in a pregnant woman when donating blood, it means that sensitization has not occurred, but prevention is still required. To prevent the production of antibodies when fetal red blood cells come into contact with maternal blood, anti-Rhesus immunoglobulin is prescribed in a special course, which prevents fetal red blood cells from being recognized as foreign, thus preventing sensitization.
Immunoglobulin is usually prescribed in the following cases:
- if antibodies are not detected at the 28th week of pregnancy;
- such therapy is required after the birth of an Rh-positive child to prevent postpartum sensitization (during the first 72 hours);
- after cases such as abortion, ectopic pregnancy, miscarriage, taking chorionic villi and amniotic fluid for analysis and other risk factors.
The effect of immunoglobulin does not last long - about 12 weeks, so each subsequent pregnancy of an Rh-negative woman requires repeating the course.
Diagnosis and treatment of incompatibility
In case of severe genetic disorders, the body itself rejects the embryo with mutations, resulting in a frozen pregnancy or miscarriage. If this situation occurs a second time, the help of a geneticist is required. As part of the consultation, the following may be prescribed:
- expert spermogram;
- karyotyping;
- test for mutations in specific genes;
- FISH study of germ cells.
Unfortunately, the listed diagnostic methods do not always help identify the cause of incompatibility. In such cases, a detailed DNA test can be performed - an expensive but very effective way to determine the cause of infertility.
References
- Pavlova N.I. Association of type 1 diabetes mellitus with polymorphic alleles of HLA class II genes in the Yakut population. //Pavlova N.I., Kurtanov Kh.A., Dyakonova A.T., Solovyova N.A., Sydykova L.A., Aleksandrova T.N., Filippova N.P., Nikiforova M.E., Dodokhov V.V. - Modern problems of science and education, 2021. No. 1. P.62.
- Batdyeva A.Kh. The importance of HLA system genes in predicting multifactorial diseases.// Batdyeva A.Kh., Popov A.A. – Bulletin of medical Internet conferences, 2021. No. 6. P. 1069.
- S.Vojvodic. – Association of class II HLA antigens and insulin-dependent diabetes mellitus in the population of Vojvodina. Jan-Feb 2003;56(1-2):26-31. Doi: 10.2298/mpns0302026v.
What blood types go together?
Blood group compatibility is primarily important to consider when transfusing donor blood to a patient. If the wrong group is infused into the patient, this will cause red blood cells to stick together, which form a blood clot and blockage of blood vessels, which can lead to death. To understand why blood incompatibility may occur due to an inappropriate group, you need to know how separation occurs.
Plasma and red blood cells (erythrocytes) contain two types of protein antigens, which are conditionally separated (in plasma a and b, in red blood cells A and B). But at the same time, only one type of antigen A or a, as well as B or b can be present in the blood.
As a result, the following division into groups occurs:
| Blood type | Plasma antigen | Red blood cell antigen |
| 1 (0) | a and b | — |
| 2 (A) | b | A |
| 3 (B) | A | B |
| 4 (AB) | — | AB |
There is no ideal group that will be compatible with all blood groups, both for transfusion and for receiving. When determining blood compatibility, the presence of antigens (A/a or B/b) is taken into account. The following is a discussion of which groups are allowed to be combined during transfusion and why:
First group
In blood group 1 (0), antigens of both types are present only in plasma and are absent in erythrocytes. Therefore, this group is an ideal donor (suitable for groups 1,2,3 and 4), but can only accept its own blood type. Zero (1) blood group is the most common.
Second group
In the “A” (2) blood group, antigens are contained in both plasma and erythrocytes. Therefore, a person with this group can only accept O (1) and A (2) blood groups. And give “A” (2) and “AB” (4) to the group.
Third group
The "B" (3) blood type also contains antigens in the plasma and blood, so it can only accept "0" (1) and its own blood type. Transfusions of “B” (3) blood group can only be given to those with “B” (3) and “AB” (4) groups.
Fourth group
Patients with “AB” (4) blood group are also considered universal, but not donors, but recipients (patients receiving blood). This property is justified by the fact that antigens in people with “AB” (4) group are contained only in erythrocytes, and are absent in plasma. As a result, owners of this group can accept any blood group, but can only give it to patients with the “AB” (4) group.
It is important that, despite the existing compatibility of some blood groups, if a transfusion is necessary, preference is given to the victim’s blood group. In the absence of one, compatible groups are used.