Indications for surgery
Surgery to remove varicocele is indicated in the following cases:
- painful sensations in the scrotal organs;
- deviations in spermogram parameters;
- changes in the size and density of the testicle, identified as a result of an external examination or ultrasound diagnosis.
The timing of the operation is determined by the indications. In case of dilated vessels, it is better to perform the operation as quickly as possible, without waiting for complications. If there are no visible changes or discomfort, then surgical intervention can be postponed, supportive therapy can be used, and periodic monitoring can be carried out using ultrasound diagnostics.
Marmara operation for varicocele
It is considered the most effective among the possible options. Compared to other types of surgical intervention, it has the lowest percentage of relapses and the minimum number of complications. This is a low-traumatic operation that is safe for neighboring tissues. Microsurgical intervention is performed through a small incision in the projection of the inguinal canal, mobilizes the spermatic cord and ligates the dilated veins. A cosmetic suture is applied, and after a few hours the patient can go home.
Contraindications
Varicocele surgery is not recommended in the following cases:
- period of puberty in a teenager. At an age when the body is rapidly developing, relapses are possible. In this case, the operation is recommended to be performed when the patient reaches 18 years of age;
- with an asymptomatic course of the disease and no complaints of discomfort from the patient. The operation may not be performed if the patient does not plan to become a father, for example in old age;
- with hemophilia and diabetes mellitus in a state of decompensation.
Strict contraindications are acute conditions in the abdominal cavity, such as appendicitis, peritonitis.
Postoperative period
After completion of the Marmara operation, the patient is placed in a ward for some time under the supervision of medical staff. After a follow-up examination, he can leave the clinic with an extract and recommendations.
The next day, I conduct another follow-up examination and a demonstration dressing change (in which I demonstrate the sequence of actions for the patient). Patients usually perform the rest of the dressings themselves at home. After 10-12 days, I once again monitor the healing of the wound and remove the stitches. At the request of the patient (for example, a nonresident who finds it difficult to come for an examination in 10 days), I apply self-absorbing sutures.
Restrictions after Marmara surgery are limited to the exclusion of heavy physical activity for a period of 1 to 3 months.
In general, the postoperative period after Marmara surgery is easy. The patient does not become incapacitated and can return to daily activities the very next day. Pain is not typical for this operation, and the need to take painkillers is extremely rare.
A final examination, including ultrasound of the scrotum and spermogram analysis (if the Marmara operation was performed for infertility), is carried out 3 months after the operation.
Preparing for surgery
Varicocele surgery in men is planned, so before performing it it is necessary to undergo a standard examination, which includes:
- general blood and urine tests;
- blood test to identify pathogens of genitourinary infections;
- blood biochemistry;
- coagulogram;
- ECG;
- spermogram.
Be sure to inform your doctor if you are allergic to any medications.
5–7 days before varicocele surgery, it is advisable to stop blood thinning medications. If they are prescribed for health reasons, you must inform your doctor about this.
During the consultation, ask the doctor all the questions you have about how the operation is performed, how long it lasts, and what the prognosis is in your particular case.
Gonadal vein embolization
We are talking about thrombosis of a damaged vein. A special catheter is inserted through a puncture of the vein in the thigh; it is gradually brought to the renal and then to the spermatic vein. Using contrast, the doctor determines which vessels need to be turned off. Using a catheter, a substance is injected that embolizes and “turns off” pathologically dilated veins.
Embolization requires virtually no downtime because the entire operation is performed through a small puncture. This is an effective and modern treatment method.
The choice of treatment method for varicocele depends on the patient’s wishes, his state of health, and the availability of medicine.
To receive treatment for varicocele at the highest level, contact the Urology Clinic named after R. M. Fronshtein of the First Moscow State Medical University named after I.M. Sechenov (State Urology Center). September 9, 2020
Akopyan Gagik Nersesovich - urologist, oncologist, doctor of medical sciences, doctor of the highest category, professor of the department of urology of the Federal State Autonomous Educational Institution of Higher Education First Moscow State Medical University named after. THEM. Sechenov
Clinic of Urology named after R. M. Fronshtein of the First Moscow State Medical University named after I.M. Sechenov invites you to an appointment with experienced urologists. To get an appointment with a qualified specialist, just fill out a short online application. Be sure to fill out all the fields, including a brief description of the symptoms (the “Information” column), specify whether you are interested in a secondary or primary appointment.
Pay attention to the “Attach file” button - it allows you to immediately send medical documents to the doctor in electronic form. This may include images, tests and other information that will be important to determine the diagnosis.
Still have questions? Call us by phone or! On a weekday, you can come for a consultation with a doctor within a few hours after filling out the online application. Do not delay visiting a specialist if you are concerned about your genitourinary health!
Varicocele removal methods
Today, several types of surgical treatment of varicocele are practiced.
Classic varicocele surgery using the methods of Ivanissevich and Palomo. Veins are removed in an open manner through incisions measuring 3–5 cm. At the present stage of development of medicine, the methods are considered outdated. The only advantage is the low cost of the operation. There are significantly more disadvantages: a high risk of relapses and complications, a long recovery period.
Laparoscopic varicocele surgery through punctures, which is performed under general anesthesia. The punctures are almost invisible and heal quickly. The method has proven itself well in bilateral pathology. The risk of relapse is minimal.
Endoscopic sclerosis of the affected vessel is performed through a puncture in the femoral vein under the control of a microscope and an X-ray machine. The method is indicated for bilateral pathology, severe pain or asymptomatic disease. The recovery period is very short. The only drawback is the use of x-rays.
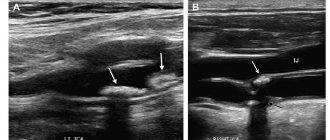
Microsurgical operation Marmara. The manipulation is performed under the control of an electron microscope (photo). It allows you to work only with the damaged vessel, without affecting other veins and lymphatic ducts. Today this is the most progressive method of removing varicoceles. It does not require long-term hospitalization, there is practically no recovery period, the incision heals very quickly, and the likelihood of relapse is extremely low.
Laparoscopic clipping for varicocele
Laparoscopic varicocelectomy has many advantages: cosmetic effect, short rehabilitation period and the ability to quickly return to normal life. But at the same time, there is a high risk of affecting the lymphatic pathways. To prevent this from happening, contrast is used.
The use of an endovideosurgical method for treating varicocele allows one to accurately assess the number of branches of the testicular vein and cut them off completely, leaving the artery intact.
Diagnosis and treatment tactics for varicocele:
Diagnosis of varicocele in our clinic may include examination, palpation tests, ultrasound examination of the scrotal organs, Dopplerography of blood vessels, and spermogram. Such an examination allows you to diagnose varicocele with 100% certainty, determine the extent of the disease and spermatogenesis disorders, and decide on the treatment method. Today, the main method of treating varicose veins is surgery. Indications for surgery are pain that is not amenable to symptomatic treatment, testicular atrophy and infertility. In some cases (1-2 degrees of varicocele, absence of pain and testicular atrophy, which is rare), therapeutic treatment is carried out aimed at identifying and eliminating the causes of varicocele.
Recovery
After completion of the procedure, the patient is transferred to the hospital. If there are no complications, discharge is possible within 2-3 days.
Full recovery takes about a month. During the rehabilitation period, the patient should refuse sexual intercourse and strictly follow all instructions of the attending physician.
Varicocele is a male disease that affects not only the patient’s quality of life, but also deprives him of the opportunity to have children. This is why treatment should not be neglected. Source: Povoroznyuk M.V. Varicocele as a cause of impaired fertility in men with infertility in marriage / M.V. Povoroznyuk // Reproductive health. Eastern Europe. - 2014. - No. 5 (35). — pp. 139-146.
Modern surgical techniques used at SM-Clinic have a high degree of effectiveness and are as safe as possible for the patient. Make an appointment at the SM-Clinic medical center to learn more about the disease and treatment options.
Laparoscopy technology
Stages of surgical procedures:
- administration of general anesthesia;
- three trocars (tubes through which instruments are inserted) are installed into the peritoneal area through punctures;
- through a Veress needle, the cavity is filled with carbon dioxide (this improves the movement of instruments);
- a laparoscope is inserted through one trocar, the others serve to provide access for surgical instruments to the required area;
- dilated veins are isolated, ligation and excision of diseased areas are carried out, the flow of blood in the affected vessels is stopped;
- the instruments are removed, and an aseptic bandage is applied to the puncture sites.
The laparoscopic revascularization operation lasts from 45 minutes to one hour.
Predicting the results of treatment
The effectiveness of laparoscopic surgery has been proven by the fact that patients return to a full active life after a short period of rehabilitation. Up to 90% of men gain the opportunity to become fathers. The qualitative composition of sperm is restored, sperm become mobile, and their number increases.
The main condition for operated patients is compliance with the rules of the recovery period and careful monitoring of their well-being.
In cases of unpleasant or painful sensations, you should immediately visit a doctor. Signs of concern may include:
- change in the size of the scrotum;
- pain symptoms in the scrotum area;
- body temperature above 37°;
- painful sensations when urinating.
Questions about the article
Ivan
December 4, 2021 at 07:25 pm
Hello!
12 days after the marmara operation, the thickening in my pubic area does not go away and I do not feel touch to the skin. It's like a slight swelling. How serious is this? The stitches have already healed and are not inflamed.
Anton Evgenievich Rotov
December 4, 2021 at 08:44 pm
I don't think it's serious or dangerous. But it’s still better to see a urologist
Arthur
August 28, 2021 at 03:48 pm
Hello! Will it hurt during the operation?
Anton Evgenievich Rotov
August 29, 2021 at 08:56
Of course not! No pain, regardless of the type of anesthesia - general or local!
Fedor
August 4, 2021 at 10:57 pm
Hello! I have a question. What does “avoiding heavy physical activity” mean? For example, lifting a suitcase when traveling? The plane rides themselves?
Anton Evgenievich Rotov
August 5, 2021 at 10:09 am
I usually explain it like this. The first month - only everyday activity (walking, running - without restrictions, weights - no more than 5-7 kg). Next - up to 3 months - exercises with your own weight (push-ups, pull-ups, squats without weights, etc.), weights - up to 10-15 kg. After 3 months - no restrictions.
Dmitriy
May 27, 2021 at 11:54 am
There is no pain, but upon palpation it feels like the spermatic cord is slightly changed, but not always, sometimes it returns to normal, becomes the same as on the right, what could this mean, I had a marmar operation a month ago
Dmitriy
May 27, 2021 at 05:36
Hello, 2 months ago I had an operation according to Ivanasseivich, after which I began to engage in physical activity and a relapse was revealed, then a month after the 1st operation, I had a second operation according to marmara, a month has already passed when I can return to full physical activity, for example swimming , basketball and what can I do now?
Anton Evgenievich Rotov
May 27, 2021 at 10:39 am
Bodyweight exercises (including football, basketball) are acceptable one month after surgery. With weights - after 3 months
How does varicocele manifest?
The disease is characterized by the fact that at first it practically does not bother the patient at all. Varicocele does not cause pain or any other alarming symptoms in 50-60% of patients. However, having been undetected during preventive examinations in adolescence and during subsequent military medical examinations, it becomes a serious problem for men in later years.
About 40% of male infertility is associated with this disease, and in addition, with age, noticeable pain in the scrotum and left groin begins to appear, radiating to the side or thigh. These symptoms worsen after physical activity and prolonged standing. Venous congestion from the testicle is transmitted to the periprostatic area, which leads to congestive prostatitis.
Additional signs of varicocele include:
- dilated veins of the scrotum, tortuous and protruding cords that create relief under the skin, distinguishing it from the healthy half (symptom of “earthworms”);
- if you take a deep breath with your stomach and tense your abdominal muscles, the dilated veins become denser to the touch;
- when standing, after a hot bath and in hot weather, the dilation of the veins of the scrotum becomes more noticeable.