Sometimes cancer patients require blood transfusions. If the doctor said that he plans to prescribe a blood transfusion, the patient usually has a lot of questions. Why is the procedure needed? Did something terrible happen? How safe is blood transfusion? Can you get HIV and other dangerous infections from a donor? How will the body react to someone else's blood? Will there be any complications? Is it possible to refuse the procedure or replace it with something else? [1,2]
Below you will find answers to many questions.
- What you need to know about blood?
- In what cases do cancer patients need blood transfusions?
- What are the types of blood transfusion?
- Red blood cell transfusion
- Plasma transfusion
- Platelet transfusion
- Cryoprecipitate transfusion
- Leukocyte transfusion
- How is the blood transfusion procedure performed?
- From whom can a blood transfusion be given?
- How is donor blood tested?
- Are there any alternatives?
- How safe is it?
- Is it possible to refuse a blood transfusion?
- Price
What you need to know about blood?
Doctors and scientists often refer to blood as the body's internal environment. It washes all organs. Blood performs many important functions: it carries oxygen, nutrients and hormones, removes waste products of metabolism, provides immune protection, and helps regulate body temperature.
Blood consists of two main parts:
- The liquid part is plasma. It is a solution of salts, ions, proteins and other substances.
- Blood cells. Erythrocytes (red blood cells) contain hemoglobin and transport oxygen. Leukocytes (white blood cells) provide nonspecific and immune protection. Platelets (blood platelets) form a clot when bleeding needs to be stopped. [1,3,4]
Book a consultation 24 hours a day
+7+7+78
In what cases do cancer patients need blood transfusions?
The cause may be the malignant tumor itself or side effects of antitumor treatment.
Some types of cancer, especially tumors of the gastrointestinal tract and tumors of the female genital area (vagina, cervix, uterus), can cause internal bleeding.
With a long course of cancer, various disorders occur in the body, which cause the so-called anemia of a chronic disease.
Some malignant tumors affect the red bone marrow (the main organ of hematopoiesis), or organs that are necessary to maintain a normal number of blood cells (spleen, kidneys). These types of cancer may also require blood transfusions.
Donor blood is needed by patients after complex operations that are accompanied by large blood loss.
Chemotherapy and radiation therapy affect not only tumor cells, but also other rapidly dividing cells in the body. Sometimes they cause quite a lot of damage to the red bone marrow. It disrupts the production of blood cells, which threatens anemia, bleeding, and severe infections against the background of decreased immunity. Blood transfusion helps normalize the patient's condition and prevent complications. [5-7]
What does transfusion help with?
Solid tumors lead to significant changes in the hematopoietic system. Under their influence, anemia and abnormalities in the blood clotting system can develop.
The disintegration of tumors leads to depletion of the bloodstream and blood reserve of the body. Surgical treatment also leads to massive bleeding. All of the above factors lead to the fact that the body’s own reserve is depleted and it requires a blood transfusion from a donor. Due to insufficient blood volume, treatment may be delayed because In case of anemia and thrombocytopenia, chemotherapy cannot be administered.
Chemotherapy drugs can have side effects on blood germs and worsen thrombocytopenia. That is why constant monitoring of red and white blood indicators and coagulation properties is necessary. If any deviations from the norm are noted, blood transfusion is prescribed according to all rules.
Red blood cell transfusion
The main function of erythrocytes (red blood cells) is the delivery of oxygen to tissues and the return transport of carbon dioxide to the lungs. A condition in which the number of red blood cells in the blood decreases is called anemia. Actually, this is an indication for red blood cell transfusion. The doctor makes a decision depending on how quickly the anemia increases:
- With chronic anemia, which increases gradually, there is no need to rush. The doctor monitors the patient’s condition, controls the level of red blood cells and hemoglobin. If these indicators decrease significantly, or the patient’s condition worsens, red blood cells are transfused. For heart and lung diseases that impede oxygen delivery to tissues, transfusions may be required even if there is a relatively small decrease in hemoglobin levels.
- Acute blood loss requires immediate action. This usually happens during surgery. If the doctor is planning a complex operation during which the patient will lose a lot of blood, blood transfusion may be performed in advance. [8]
Red blood cell mass
Evaluation of the effectiveness of the procedure
With the help of properly prescribed blood transfusion, it is possible to normalize the condition of a cancer patient and prevent severe complications of the disease. The result of a properly organized blood transfusion for oncology is visible almost immediately after its completion:
- hemoglobin levels increase;
- platelet count increases;
- the blood is saturated with oxygen;
- the feeling of weakness and chronic fatigue disappears;
- it becomes possible to carry out radiation therapy, chemotherapy, or perform surgery;
- Feeling better after blood transfusion for blood cancer.
The procedure increases the chances of a positive treatment outcome. The duration of the effect of blood transfusion depends on the nature of the oncological process and the individual characteristics of the patient. A positive result is more stable in the absence of constant internal bleeding.
Prescribing and performing blood transfusions in cancer patients requires high professionalism. The further condition of the patient depends on the procedure, especially during blood transfusion for stage 4 cancer, so it is necessary to undergo it in a safe place. Oncology provides a range of services related to oncology. Contact our center, here you can get advice, undergo an examination or additional examination, and receive the necessary treatment.
Plasma transfusion
Plasma, the liquid part of blood, appears as a clear, yellowish liquid. It contains blood clotting factors - substances that are necessary for the formation of a blood clot and stop bleeding. Plasma also contains substances that protect the body from infection.
Plasma can be stored frozen for up to 12 months. When necessary, it is thawed and the resulting fresh frozen plasma is transfused into the patient.
The main indication for plasma transfusion in cancer patients is increased bleeding. The procedure is also necessary for DIC syndrome (disseminated intravascular coagulation syndrome) - a serious condition in which blood clots form in small vessels, ultimately depleting the entire supply of platelets and coagulation factors, and there is a risk of severe bleeding. [9-10]
Blood plasma transfusion
Types of blood transfusions
There are several methods of blood transfusion:
- indirect;
- direct;
- exchange;
- autohemotransfusion.
Several routes of administration are used:
- into the veins - the most common method;
- into the aorta;
- into an artery;
- into the bone marrow.
The most commonly used method is the indirect method. Whole blood is used extremely rarely today, mainly its components: fresh frozen plasma, erythrocyte suspension, erythrocyte and leukocyte mass, platelet concentrate. In this case, a disposable blood transfusion system is used to administer the biomaterial, to which a container or bottle with a transfusion medium is connected.
Direct transfusion is rarely used - directly from the donor to the patient. This type of blood transfusion has a number of indications, including:
- prolonged bleeding in hemophilia that cannot be treated;
- lack of effect from indirect transfusion in a state of shock of 3 degrees with blood loss of 30-50% of blood;
- disturbances in the hemostatic system.
This procedure is carried out using a device and a syringe. The donor is examined at the transfusion station. Immediately before the procedure, the group and Rh of both participants are determined. Tests for individual compatibility and bioassays are carried out. During direct transfusion, up to 40 syringes (20 ml) are used. Blood transfusion follows the following scheme: a nurse takes blood from a vein from a donor and hands the syringe to the doctor. While he is injecting the material into the patient, the nurse is drawing the next portion and so on. To prevent clotting, the first three syringes are filled with sodium citrate.
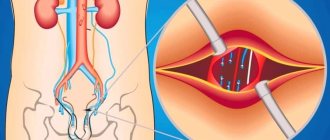
Exchange transfusion is used for poisoning, hemolytic disease of the newborn, acute renal failure, and transfusion shock. In this case, blood is partially or completely removed from the patient’s bloodstream and at the same time the same volume is replaced.
During autohemotransfusion, the patient is transfused with his own material, which is taken during the operation immediately before the procedure or in advance. The advantage of this method is the absence of complications during blood transfusion. The main indications for autotransfusion are the inability to select a donor, a rare group, and the risk of severe complications. There are also contraindications - the last stages of malignant pathologies, severe kidney and liver diseases, inflammatory processes.
Platelet transfusion
Platelets, or blood platelets, take part in the formation of a blood clot and stop bleeding. Their levels may drop due to chemotherapy, radiation therapy, or if the tumor has replaced normal red bone marrow tissue. Platelet transfusions are usually required for cancer patients in one of three cases:
- if the level of platelets in the blood has fallen below a critical value;
- if there is increased bleeding, risk of bleeding;
- if you are undergoing surgery during which significant blood loss is expected. [11,12]
Platelet mass
Blood for transfusion and its components
Human blood consists of blood cells and plasma. Various drugs are prepared from these components, although this process cannot be called easy in technological terms.
The most common blood components that are obtained from whole blood are white blood cells, plasma, platelets and red blood cells.
Red blood cells
Red blood cells are transfused when there is a shortage of red blood cells. Indications for the procedure are hematocrit levels below 0.25 and hemoglobin levels below 70 g/l.
This can happen under the following conditions:
- Anemia developing in the early postpartum period or in the early postoperative period.
- Severe iron deficiency anemia, which develops in older people due to cardiac or respiratory failure, or in young women while pregnant. In this case, the procedure can be performed before the onset of labor or before an upcoming operation.
- Anemia due to various diseases of the digestive system.
- Intoxication of the body due to severe burns, poisoning, purulent processes. Red blood cells from a donor's blood help rid the patient's body of toxic substances.
- Erythropoiesis, which caused anemia.
If the patient has symptoms that indicate a violation of blood microcirculation, then he is transfused with an erythrocyte suspension. It is a dilute mass of red blood cells.
To minimize the risk of developing undesirable reactions from the body, it is necessary to use red blood cells washed three or five times for transfusion. Using a saline solution, platelets, leukocytes, preservatives, electrolytes, microaggregates and other substances that the sick person’s body does not need are removed from them. If the red blood cell mass has been subjected to a procedure for removing leukocytes and platelets from it, then it is called EMOLT.
The blood that is currently used for transfusion is frozen after collection from the donor. Therefore, the red blood cell mass is washed off on the day when they are going to transfuse it.
EMOLT is infused into patients for the following indications:
- If the patient has previously experienced complications caused by blood transfusion.
- The presence of isoimmune or autoimmune antibodies in the patient’s blood. A similar situation is often observed with hemolytic anemia.
- Washing of red blood cells is required when it is necessary to transfuse a large amount of blood, which reduces the risk of developing massive blood transfusion syndrome.
- Increased blood clotting.
- The patient has renal or liver failure.
Thus, it becomes obvious that EMOLT makes it possible to help a person who has absolute contraindications to whole blood transfusion.
Plasma
Plasma contains a large amount of protein components, vitamins, antibodies, hormones and other useful substances that patients require in a wide variety of situations. Therefore, plasma is a component of blood that is in great demand for transfusions. It can also be used in combination with other blood components.
Plasma is transfused in the following cases: a decrease in the total volume of circulating blood, bleeding, immunodeficiency, exhaustion and other severe health problems.
Platelets
Platelets are platelets that take part in the process of hematopoiesis. They form white blood clots, which are necessary to stop bleeding from the capillaries. The fewer platelets in a person’s body, the higher the risk of bleeding. If their level decreases to a critical zero level, then the likelihood of hemorrhage in the brain increases.
Storing and harvesting platelets is a very complex process. Platelet mass cannot be prepared in advance at all, since it is stored for only a short time and also requires constant stirring. Therefore, platelets are transfused only on the day of collection from the donor. Before this, the blood is urgently checked for infections.
Most often, a person who is a relative of the victim acts as a donor. Alloimmunization develops in those patients who frequently receive platelet transfusions. This condition is also a common companion for women who have suffered a difficult abortion or childbirth, as a result of which they required donor blood.
For platelet transfusion to be successful, it is highly desirable to conduct an analysis to select platelets based on antigens of the leukocyte HLA system. This analysis is very financially expensive and also very labor intensive.
In addition, platelet transfusions carry the risk of another type of disease called graft-versus-host disease. This happens if the donor's platelets contain aggressive T and B cells. Therefore, platelet transfusion is quite a complex task.
Indications for platelet transfusion:
- Thrombocytopathies, which are accompanied by increased bleeding. This pathology can be either acquired or congenital. If the platelet level reaches 60.0*109/l, but there is no hemorrhagic syndrome, then this is not an indication for blood transfusion. The platelet mass is transfused when the platelet level reaches 40*109/l.
- Surgical intervention.
- Preparation for treatment with cytostatics.
Leukocytes
Transfusion of leukocyte mass is an even more complex task compared to transfusion of platelet mass. This procedure is performed to treat leukopenia and is also indicated for patients undergoing radiation or chemotherapy.
This procedure is often abandoned, since it is very difficult to obtain high-quality leukocyte mass. It is mined only using a separator. After being removed from the donor’s body, the leukocytes die very quickly. In addition, leukocyte transfusion is associated with complications such as chills, shortness of breath, tachycardia, increased body temperature, and a drop in blood pressure.
How is the blood transfusion procedure performed?
Although blood transfusion is formally equated to surgical interventions, this procedure is not at all scary and is practically painless. Blood transfusion is carried out through a needle that is inserted into a vein. It is no more painful than a regular intravenous injection. If the patient already has a central venous catheter, donor blood can be administered through it.
The procedure can take different times, depending on which blood components are transfused: from 30-60 minutes (platelet transfusion) to 2-4 hours (red blood cell transfusion).
Indications for transfusion
There are absolute and specific indications for blood transfusion. The absolute ones include the following:
- Acute blood loss - more than 30% within two hours. This is the most common indication.
- Surgery.
- Continuous bleeding.
- Severe anemia.
- State of shock.
For transfusion, in most cases, it is not whole blood that is used, but its components, such as plasma.
Among the specific indications for blood transfusion are the following:
- Hemolytic diseases.
- Anemia.
- Severe toxicosis.
- Purulent-septic processes.
- Acute intoxication.
How is donor blood tested?
A person who donates blood for the first time must fill out a questionnaire, undergo an examination by a therapist, a dermatovenerologist, and take tests for blood type, Rh factor, and infections: HIV, viral hepatitis B and C, syphilis, cytomegalovirus. Sometimes the examination program can be expanded.
If signs of a particular infection are found in the donor’s blood, it is discarded and not used in the future.
The compatibility of the blood of the donor and the recipient is checked using a special test - a cross-blood compatibility test.
Where do they get the material?
Preparation, separation into components, preservation and preparation of drugs are carried out in special departments and at blood transfusion stations. There are several sources of blood, including:
- Donor. This is the most important source of biomaterial. Any healthy person can become one on a voluntary basis. Donors undergo mandatory testing, during which they are examined for hepatitis, syphilis, and HIV.
- Waste blood. Most often it is obtained from the placenta, namely, it is collected from women in labor immediately after childbirth and ligation of the umbilical cord. It is collected in separate vessels containing a preservative. Drugs are prepared from it: thrombin, protein, fibrinogen, etc. One placenta can produce about 200 ml.
- Corpse blood. Taken from healthy people who died suddenly as a result of an accident. The cause of death can be electric shock, closed injuries, cerebral hemorrhages, heart attacks, and more. Blood is drawn no later than six hours after death. The blood that flows out on its own is collected in containers, adhering to all the rules of asepsis, and used for the preparation of drugs. This way you can get up to 4 liters. At the stations where the preparation is carried out, it is checked for group, rhesus, and the presence of infections.
- Recipient. This is a very important source. On the eve of the operation, blood is taken from the patient, preserved and transfused. It is allowed to use blood that has spilled into the abdominal or pleural cavity during illness or injury. In this case, you don’t have to check it for compatibility, various reactions and complications occur less often, and transfusion is less dangerous.
Are there any alternatives?
Sometimes blood disorders can be corrected with medications. For example, colony-stimulating factors are used to increase the number of white blood cells.
However, in cases where blood transfusion is necessary, there are no alternatives. There are no blood substitutes that can provide similar effects. That is why donation is constantly promoted in all countries of the world, including Russia, and donor days are held periodically. It is important. This helps save the lives of many people. [15]
Blood transfusion for a newborn baby
The indications for blood transfusion to a newborn child are similar to the indications for blood transfusion to an adult. The blood dose is selected on an individual basis. Doctors should be especially attentive to children who were born with hemolytic disease of the newborn.
In case of hemolytic jaundice, the child undergoes replacement blood transfusion using EMOLT group 0(I), with a mandatory match of the Rh factor.
Blood transfusion to a newborn baby is a complex process that requires caution and utmost attention from the doctor.
How safe is it?
Can you get an infection from donated blood? Donated blood goes through rigorous testing, but there are still risks, even though they are negligible. Thus, the likelihood of becoming infected with HIV through donated blood is lower than the likelihood of being struck by lightning during a person’s lifetime. The risk of contracting hepatitis C is 1 in 2,000,000. Doctors and scientists are constantly working to reduce the risks to zero. [16]
Can incompatible blood be transfused? Before blood transfusion, the recipient's blood type and Rh factor must be determined; the doctor must make sure that the blood of the donor and recipient are compatible.
But the blood of different people can differ not only in group A0 and Rh factor. It is very difficult to take into account all the nuances. Therefore there is a slight risk of an allergic reaction. Most often it manifests itself in the form of fever, chills, and rash. Such complications are rarely life-threatening. In order to provide assistance to the patient, if necessary, a medical professional is constantly monitoring his condition during the procedure.
An allergic reaction can occur not only immediately during the transfusion, but also within 48 hours after it. You should immediately tell your doctor if your body temperature rises above 38°C, chills, rash, itching, redness of the skin, shortness of breath, difficulty breathing, nausea, lower back pain, blood in the urine, weakness. The most dangerous symptom is chest pain, which requires immediate attention. If you are at home, you should immediately call an ambulance. [5]
Algorithm for blood transfusion
ABO system The main antigens of the ABO system are 2-A and B. As separate specificities, 2 more antigens are distinguished in it - A, B and A1. The absence of these 4 antigens on red blood cells is designated O. Anti-A and anti-B antibodies are of natural origin. They are designated by the Greek α and β. There are 4 blood groups formed by combinations of antigens A and B with isohemagglutinins α and β. On red blood cells of the first group O (I), antigens A and B are absent, the plasma contains antibodies α and β. In the second blood group A (II), the erythrocytes have antigen A, and the plasma contains β antibodies. The third group B (III) contains the B antigen and α antibodies. In the fourth group AB (IV), antigens A and B are present; isohhemamaglutinins α and β are absent in the blood serum.
Rh factor
Rh factor is an antigen found in the red blood cells of 85% of people, as well as in Macaus rhesus monkeys. The blood of people whose red blood cells contain Rh is called positive. There are several different antigens of the Rh system, including the Hr group, which forms a common system with Rh. Rh-Hr Including -3 varieties of Rh agglutinogen (C, D, E) -3 varieties of Hr agglutinogen (c, d, f) and other rarer species. Agglutinogen Hr is found in the red blood cells of 83% of people. The Rh factor is inherited as a dominant trait and does not change throughout life. The transfusion of blood components has the right to be carried out by: - The attending physician or the doctor on duty. -During the operation, the surgeon or anesthesiologist (not involved in the operation or anesthesia). -Doctor of the blood transfusion department or room. -Transfusiologist.
Determination of blood group according to the ABO system (Using coliclones) - 2 drops (0.1 ml) of the reagent and next to one drop of red blood cell sediment (0.02 - 0.03 ml) - Serum and red blood cells are mixed with a glass rod - The plate is periodically shaken, observing the progress of the reaction for 5 minutes (allows you to identify the weak agglutinogen A2) - interpret the results
Difficult to determine blood types
Blood subgroups. Antigen A, contained in erythrocytes of groups A (II) and AB (IV), can be represented by two variants (subgroups) - A_1 and A_2. Antigen B has no such differences. Nonspecific agglutination of erythrocytes. It is judged on the basis of the ability of erythrocytes to agglutinate with sera of all groups, including AB (IV). Nonspecific agglutination is observed in autoimmune hemolytic anemia and other autoimmune diseases accompanied by the adsorption of autoantibodies on erythrocytes, in hemolytic disease of newborns, whose erythrocytes are loaded with maternal alloantibodies.
Blood chimeras. Blood chimeras are the simultaneous presence in the bloodstream of two populations of red blood cells that differ in blood type and other antigens. Transfusion chimeras arise as a result of repeated transfusion of red blood cells or suspension of group 0 (I) to recipients of another group. True chimeras occur in heterozygous twins, as well as after allogeneic bone marrow transplantation. Other features. Determining the AB0 blood group and Rhesus affiliation can be difficult in patients due to changes in the properties of red blood cells in various pathological conditions (in patients with liver cirrhosis, burns, sepsis). Determination of Rh-belonging
Apply a large drop (about 0.1 ml) of reagent to the plate. A small drop (0.02-0.03 ml) of the red blood cells being tested is placed nearby. Mix the reagent with red blood cells thoroughly using a glass rod. Rock the record gently. The reaction results are taken into account 3 minutes after mixing. If agglutination is present, the blood being tested is labeled as Rh positive; if not, it is marked as Rh negative.
Compatibility test on a plane at room temperature
To conduct tests for individual compatibility, the patient’s blood (serum) is used, taken before transfusion or no more than 24 hours before, provided it is stored at a temperature of +4+2°C.
Apply 2-3 drops of the recipient's serum to the plate and add a small amount of red blood cells so that the ratio of red blood cells to serum is 1:10. Next, the red blood cells are mixed with the serum, and the plate is gently rocked for 5 minutes. Compatibility test using 33% polyglucin
Add 2 drops (0.1 ml) of recipient serum, 1 drop (0.05) ml of donor erythrocytes into the test tube and add 1 drop (0.1 ml) of 33% polyglucin.
The test tube is tilted to a horizontal position, shaking slightly, then slowly rotated so that its contents spread over the walls in a thin layer. Contact of erythrocytes with the patient’s serum while rotating the tube should continue for at least 3 minutes.
After 3-5 minutes, add 2-3 ml of physiological solution to the test tube and mix the contents by inverting the test tube 2-3 times without shaking.
The result is taken into account by viewing the test tubes with the naked eye or through a magnifying glass. Agglutination of red blood cells indicates that the blood of the recipient and the donor are incompatible; the absence of agglutination is an indicator of the compatibility of the blood of the donor and recipient.
Technical errors
Incorrect order of reagents. Temperature conditions (blood group determination is carried out at a temperature not lower than 15°C and not higher than 25°C) The ratio of reagents and red blood cells being studied. Duration of observation. (allows us to identify weak agglutinogen A_2, characterized by delayed agglutination)
Biological sample
The biological test is carried out regardless of the volume of the blood transfusion medium and the speed of its administration.
If it is necessary to transfuse several doses of blood components, a biological test is carried out before the start of the transfusion of each new dose. Technique for conducting a biological test: 10 ml of blood transfusion medium is transfused once at a rate of 2 - 3 ml (40 - 60 drops) per minute
observe the recipient for 3 minutes, monitoring his pulse, breathing, blood pressure, general condition, skin color, and measure body temperature
This procedure is repeated twice more. The appearance during this period of even one of the clinical symptoms such as chills, lower back pain, a feeling of heat and tightness in the chest, headache, nausea or vomiting requires immediate cessation of the transfusion and refusal to transfuse this transfusion medium.
The urgency of transfusion of blood components does not exempt one from performing a biological test!!!
The doctor performing the transfusion of blood components is obliged to:
1. Determine the indications for blood transfusion therapy, taking into account contraindications.
2. Obtain informed voluntary consent of the recipient or his legal representative to conduct blood transfusion therapy in the prescribed form.
3. Conduct an initial determination of the patient’s blood group according to the ABO system.
IT IS STRICTLY PROHIBITED TO USE DATA ABOUT GROUP MEMBERSHIP FOR THE ABO AND RHESUS SYSTEMS FROM THE PASSPORT, PREVIOUS ILLNESS HISTORY AND OTHER DOCUMENTS.
4. Include in the referral to the clinical diagnostic laboratory (form No. 207/u) information about the result of determining the blood group according to the ABO system, a series of diagnostic tests, transfusion and obstetric-gynecological history. Sign the direction
5. Familiarize yourself with the conclusion of the clinical diagnostic laboratory. Transfer data about the group and Rh affiliation of the patient to the front part of the inpatient medical card, indicating the date of the analysis and your last name.
6. Prepare a pre-transfusion epicrisis.
7. Conduct a macroscopic assessment of laboratory gelatin and diagnosticums.
8. Conduct a macroscopic assessment of each dose of blood transfusion medium.
9. Immediately before transfusion, determine the recipient’s blood group according to the ABO system.
10. Determine the blood group according to the ABO system with erythrocyte-containing medium.
11. Check the compliance of passport data.
12. Conduct a compatibility test between the recipient’s blood and the donor’s blood (transfusion medium) according to the ABO and Rh systems.
13. Record the results of isoserological studies in the protocol of the blood transfusion operation.
TESTS FOR INDIVIDUAL COMPATIBILITY ACCORDING TO THE ABO AND RHESUS SYSTEM DO NOT REPLACE EACH OTHER.
ARE CARRIED OUT IN ALL CASES WITH BLOOD SAMPLES FROM EACH CONTAINER.
MANDATORY EVEN IF THE ERYTHROCYTE MASS OR SUSPENSION IS SELECTED FOR THE RECIPIENT INDIVIDUALLY IN A SPECIALIZED LABORATORY.
14. Conduct a biological test. Record its result in the protocol of the blood transfusion operation.
15. Monitor the condition of the recipient, the rate of administration of the transfusion medium.
16. If the patient’s condition changes, first of all, exclude a post-transfusion complication.
17. Assess blood pressure, pulse, thermometry results.
18. Register blood transfusion:
•in the observation diary of the medical record of an inpatient;
• in the register of registration of blood transfusions and its components (form No. 009/u);
•fill out the blood transfusion protocol
19. Conduct a macro-assessment of the first portion of urine.
20. Prescribe clinical blood and urine tests the next day after blood transfusion.
21. Assess daily diuresis, water balance, results of urine and blood tests.
22. Observe the patient and reflect the observation results in the medical history diary. If clinical symptoms and laboratory parameters change before the patient is discharged from the hospital, first of all exclude a post-transfusion complication.
Complications - Immune complications (acute hemolysis, hyperthermic non-hemolytic reaction, anaphylactic shock, non-cardiogenic pulmonary edema)
-Non-immune complications (acute hemolysis, bacterial shock, OSHF, pulmonary edema)
- Immediate complications (alloimmunization with antigens of erythrocytes, leukocytes, platelets or plasma proteins, hemolysis, graft-versus-host disease, post-transfusion purpura)
Long-term complications
-Immune (hemolysis, Graft-versus-host disease, Post-transfusion purpura, Alloimmunization with antigens of erythrocytes, leukocytes, platelets or plasma proteins
Literature:
A. G. Rumyantsev, V. A. Agranenko. Clinical transfusiology-M.: GEOTAR MEDICINE, 1997.
E. B. Zhiburt. Transfusiology-S.: PETER, 2002.
Regulations and audit of blood transfusion. Guide for doctors. -M. , RANS, 2010.
Ragimov A. A. Transfusiology . National leadership-M.: GEOTAR Media, 2012.
S. I. Donskov, V. A. Morokov. Human blood groups: Guide to immunoserology - M.: IP Skorokhodov V. A., 2013.
Zhiburt E. B. Patient blood management//Healthcare. -2014.
Algorithms for studying erythrocyte antigens and anti-erythrocyte antibodies in difficult to diagnose cases. Methodological recommendations N 99/181 (approved by the Ministry of Health of Russia on May 17, 2000)
Order of the Ministry of Health of Russia dated November 25, 2002 N363 “On approval of the Instructions for the use of blood components”
Order of the Ministry of Health of Russia dated 04/02/2013 N183н “On approval of the rules for the clinical use of donor blood and (or) its components”
Is it possible to refuse a blood transfusion?
The patient always has the right to refuse prescribed treatment, be it chemotherapy, surgery or blood transfusion. But you need to remember some points:
- A doctor will not prescribe a procedure, especially one as serious as a blood transfusion, just like that. If the doctor decides to perform a blood transfusion, then there are good reasons for this, and first of all it is in the interests of the patient.
- Large blood loss during surgery and significant blood disorders can lead to death or serious complications and impair the effectiveness of antitumor treatment.
- There are some risks during blood transfusion, but they are negligible, and the procedure often helps save the patient's life.
Euroonko clinics officially cooperate with the largest blood banks in the country. We operate on the basis of a license for “transfusiology in outpatient and inpatient settings” issued by the health departments of Moscow and St. Petersburg.
Contraindications
Practice has shown that blood transfusion is a very responsible tissue transplant operation with possible tissue rejection and subsequent complications. There is always a risk of disruption of important processes in the body due to blood transfusion, so it is not indicated for everyone. If a patient requires such a procedure, doctors are required to consider contraindications to blood transfusion, which include the following diseases:
- stage III hypertension;
- heart failure caused by cardiosclerosis, heart defects, myocarditis;
- purulent inflammatory processes in the inner lining of the heart;
- circulatory disorders in the brain;
- allergies;
- protein metabolism disorder.
Disposable systems are used for transfusion
In cases of absolute indications for blood transfusion and the presence of contraindications, transfusion is carried out with preventive measures. For example, they use the blood of the patient himself for allergies.
There is a risk of complications after blood transfusion in the following categories of patients:
- women who have suffered miscarriages, difficult births, or given birth to children with jaundice;
- people with malignant tumors;
- patients who have had complications with previous transfusions;
- patients with long-term septic processes.
Price
- Consultation with a transfusiologist - 5100 rub.
- Complete blood count (CITO) - 2400 rub.
- Compatibility test before blood transfusion - 3,200 .
- Erythrocyte suspension, depleted of leukocytes (filtered) - 24,000 rub.
- Transfusion of blood components - 5300 rub.
- The cost of fresh frozen plasma (1 dose 250 ml) is 25,300 rubles.
- Platelet concentrate (1 dose) - 86,100 rub.
In accordance with the legislation of the Russian Federation (Law of the Russian Federation of June 9, 1993 N 5142-I “On the donation of blood and its components”), the procurement of blood, the receipt of blood components and their storage are carried out exclusively by state budgetary institutions. Blood transfusions to our patients are carried out on the basis of licenses for “transfusiology in outpatient and inpatient settings”.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- G.I. Kozin. Practical transfusiology. Practical medicine, Moscow 2005.
- Igonina M. E. Donate blood to save a life // BMIK. 2013. No. 2.
- O. A. Rukovitsyn. Hematology. National leadership. GEOTAR-Media.
- S. M. Lewis, B. Bain, I. Bates. Practical and laboratory hematology. Moscow, GEOTAR-Media, 2009.
- Seth Lotterman; Sandeep Sharma. Blood Transfusion. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
- Sandhya Yaddanapudi and LN Yaddanapudi. Indications for blood and blood product transfusion. Indian J Anaesth. 2014 Sep-Oct; 58(5): 538–542. doi: 10.4103/0019-5049.144648.
- Lawrence Tim Goodnough, MD and Anil K. Panigrahi, MD, PhDa. Blood Transfusion Therapy. Med Clin North Am. Mar 2021; 101(2): 431–447. Published online 2021 Dec 24. doi: 10.1016/j.mcna.2016.09.012.
- Giancarlo Liumbruno, Francesco Bennardello, Angela Lattanzio, Pierluigi Piccoli, and Gina Rossetti. Recommendations for the transfusion of red blood cells. Blood Transfus. 2009 Jan; 7(1): 49–64. doi: 10.2450/2008.0020-08.
- Ryan A. Lawless, MD and John B. Holcomb, MD Plasma Transfusion. Trauma Induced Coagulopathy. 2015 Dec 11: 323–337. Published online 2015 Dec 11. doi: 10.1007/978-3-319-28308-1_20.
- Giancarlo Liumbruno, Francesco Bennardello, Angela Lattanzio, Pierluigi Piccoli, Gina Rossetti, and as Italian Society of Transfusion Medicine and Immunohaematology (SIMTI) Working Party. Recommendations for the transfusion of plasma and platelets. Blood Transfus. 2009 Apr; 7(2): 132–150. doi: 10.2450/2009.0005-09.
- Atif I. Khan; FaizAnwer. Platelet Transfusion. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
- Neil Blumberg, Joanna M Heal and Gordon L Phillips. Platelet transfusions: trigger, dose, benefits, and risks. F1000 Med Rep. 2010; 2: 5. Published online 2010 Jan 27. doi: 10.3410/M2-5.
- B. Nascimento, L. T. Goodnough, and J. H. Levy. Cryoprecipitate therapy. Br J Anaesth. 2014 Dec; 113(6): 922–934. Published online 2014 Jun 27. doi: 10.1093/bja/aeu158.
- Juan Gea-Banacloche, MD. Granulocyte Transfusions: A Concise Review for Practitioners. Cytotherapy. 2021 Nov; 19(11): 1256–1269. Published online 2021 Sep 12. doi: 10.1016/j.jcyt.2017.08.012.
- A. A. Kerimov Blood transfusion: is there an alternative? // Biomedicine (Baku). 2004. No. 3.
- Polunina N.V., Gubanova M.N., Zhiburt Evgeniy Borisovich Risk of infection transmission during blood transfusion // Russian Medical Journal. 2021. No. 6.
Compatibility
It is believed that different groups can be compatible if there is no agglutination reaction during transfusion, in which antibodies attack foreign red blood cells and they stick together.
- The first is considered universal, that is, suitable for everyone, since it does not contain antigens. At the same time, people with this group cannot be given any other transfusion, only the first one.
- The second contains antigen A, so it can be transfused to people with II and IV, and to a person with such groups - I and II.
- The third blood contains antigen B. It can be transfused to people with III and IV, and people with this group - I and III.
- The fourth contains both antigens, so it can only be transfused into an IV, but any one is suitable for a person with this group.
As for Rh, it is believed that a Rh-positive person can be transfused with negative blood, but this cannot be done in the reverse order.
All this is true only theoretically, since today it is forbidden to use other blood for transfusion. In emergency cases, the first one can be used as a universal one, but only if it is Rh-negative.