“How many days do they stay in intensive care?” - this is the question I am often asked by people whose relatives are in intensive care for various reasons. So I’ll say right away that there is no clear answer to this question. Everything is very individual. A person can spend from a day to several months in intensive care, and this will depend on many factors:
- the patient's condition;
- reasons for entry;
- concomitant diseases;
- age, weight, individual characteristics.
The word “resuscitation” itself is scary, this is due to superficial knowledge of various fields of medicine (which is absolutely normal for an ordinary person), and also to the fact that our respected media very often intimidate people even more by distorting medical facts, either out of ignorance, either by his journalistic “calling”.
My specialty is anesthesiology and resuscitation, I am the doctor by whose decision the patient is transferred to the intensive care unit and the one who subsequently monitors the patient there and makes the decision on discharge. Therefore, I will tell you first-hand what and how it works there, why and why we transfer patients there, what kind of care there is and what prognosis can be given if your relative is admitted to the intensive care unit.
Why are patients transferred to intensive care?
Severe patients are transferred to the intensive care unit in agreement with the head of the department.
Reasons for translation:
- underlying disease (worsening condition - respiratory failure, critical circulatory disorder, confusion or loss of consciousness).
- condition after surgery (if an anesthesiologist-resuscitator notices that after surgery a person has not fully recovered vital functions, a decision may be made to transfer to intensive care, this minimizes risks, and the patient is under observation.
- emergency conditions - people from the ambulance can also be admitted to the intensive care unit (the criteria are the same) - acute heart attack, stroke, trauma, burns, frostbite, drowning.
How to be brought out of an induced coma
Bringing a patient out of an induced coma is an extremely complex procedure that requires special training. The administration of medications that support the patient's medicated sleep is stopped gradually.
Relatives of the patient need to understand that recovery from a coma and further rehabilitation can last many months.
The patient's consciousness is restored gradually, periods of delirium, memory impairment, speech impairment and motor activity are possible.
For reference. During rehabilitation, patients gradually learn to eat, get out of bed, and walk on their own. Restoring memory, speech and motor activity can take from several months to a year.
How many people can stay in intensive care?
In order for you to understand how individual everything is, I will tell you several cases from my practice - you will find out how and why people ended up in intensive care and what happened then.
There are standard periods for a patient to remain in intensive care: Orders, Orders of the Ministry of Health. But in reality this is not always the case. All these documents are a pretty picture, but real life is a little different. It is not always possible for a hospital to keep a patient, for example, with a stroke for a whole month - there simply is not enough staff.
Case from practice: I worked in one of the cities near Moscow. It’s a small hospital, where the intensive care unit is designed for only two people. A husband and wife came to my duty after an accident (they crashed into a tree). I am one anesthesiologist-resuscitator, there is no one to replace me. The man had a ruptured spleen, an emergency operation was performed, the second patient (a woman) was in a coma and was placed in intensive care and transferred to mechanical breathing. They were under my supervision for two days; there was simply no one to replace me. On the first day it was somehow still possible to work, but on the second day I couldn’t even sit, then they sent a team and transferred the patients to the nearest larger hospital, after which I was able to complete my shift. What is shown in the movies is beautiful and interesting, but in real life everything is different.
We also recommend reading: Pulmonary embolism, what is it?
Transfer to intensive care for pneumonia
Not everyone and not always are admitted to intensive care with pneumonia. If the condition is satisfactory, treatment in a hospital is possible. We will consider a case of severe pneumonia, in which transfer of the patient to the intensive care unit is directly indicated, because by all indications there was a serious threat to the patient’s life.
Case from practice. I was called to the therapy department, where a patient was admitted with suspected pneumonia. The patient is a man, 42 years old. On examination - shortness of breath (30-40 breaths per minute), pulse approximately 120, blood pressure 80/40, cyanosis of the nail plates and nasolabial triangle, acrocyanosis.
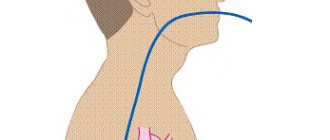
I assess the condition as extremely serious - I transfer the patient to intensive care, and immediately begin resuscitation measures. We insert the subclavian vein (in this case on the right), and begin anesthesia.
Tracheal intubation is performed, the patient is transferred to mechanical ventilation. In addition, be sure to place a catheter in the bladder.
A catheter is placed in the bladder to control diuresis (urine volume). Normally, it should be at least 30 ml/hour, and the doctor also evaluates the color of the urine. Kidney function is extremely important!
We also take other tests, ECG, chest x-ray. All this is done to clarify the diagnosis. We make sure to check that the endotracheal tube is positioned correctly. A little later we put in a gastric tube for feeding (this is not so urgent). The initial diagnosis was confirmed. The condition was stabilized. The patient spent 5 days in intensive care, during which time the underlying disease was treated as prescribed by the therapist + what the resuscitator prescribed.
On the 6th day, extubation was performed, the patient regained consciousness, and it took about two days to recover. After complete restoration of consciousness and vital functions, the patient was transferred to the ward and subsequently discharged.
That is why be vigilant, monitor your health and seek medical help in a timely manner.
Resuscitation after caesarean section
Normally, a caesarean section operation lasts about 30 minutes. It can be performed under general anesthesia or spinal (epidural) anesthesia. It depends on the wishes of the woman in labor, her individual characteristics and other factors.
In what cases may resuscitation be required after a caesarean section? This may be if the patient’s condition raises concerns among doctors, if something went wrong during the operation or if some complication occurred.
Again, a case from my medical practice. Maternity hospital, 9.30, woman, 29 years old, was taken to the operating room for a planned caesarean section. Operation was successfully completed. The child’s condition is good, the mother is conscious, but her condition causes me concern (pale skin color, weakness). At this moment, labor begins in the next department, they call me there. I leave this patient under the supervision of a nurse anesthetist. Everything is fine in that department, they urgently call me back (to the first patient).
We also recommend reading: Anesthesia for the elderly. Consequences and risks
The woman is pale, rolls her eyes, loses consciousness. The blood pressure is not determined, the pulse is 140, I put the subclavian in place, and we begin anesthesia. An operation is being carried out, donors are invited for a warm blood transfusion. 00.30 - completion of the operation. The result is removal of the uterus, the patient is alive.
The reason for the sharp deterioration of the condition is DIC syndrome (disseminated intravascular coagulation - in other words, this is a very rare, dynamic process when a large number of blood clots form in the vessels in combination with blood incoagulability, which leads to numerous hemorrhages).
No one could have predicted such an outcome, so I want each of us to understand that doctors are not Gods. And we cannot predict anything, each organism is individual and it is simply impossible to predict how it will behave with any, even small, intervention. But our task is to do everything possible to save the patient’s life!
Resuscitation after stroke, heart attack
Stroke patients can stay in intensive care for up to 21 days. With stable hemodynamics and sufficient breathing, they are transferred to a specialized department.
If their condition is stable, then they are discharged home, and their relatives take care of them.
In case of an acute heart attack, if less than 6 hours have passed since the attack, patients are taken urgently to the operating room in the radiology department for angioplasty and stenting. After the operation, such patients can be discharged home after 3-4 days.
Forecast for recovery
The prognosis is always extremely serious. First of all, due to the fact that patients are put into an artificial coma only in the presence of severe pathologies.
The further prognosis for rehabilitation and recovery depends on the main diagnosis, the duration of the medically induced coma, the patient’s age, the presence of concomitant pathologies and complications.
Important. The longer the patient is in an induced coma, the longer the further recovery period and the lower the likelihood of full recovery.
The most optimistic prognosis is observed in patients who were put into a short-term medical coma - up to several hours. There is also a good prognosis for complete rehabilitation in patients who have been in a medical coma for up to several days.
Why is anesthesia administered in intensive care?
You can often hear on TV or radio: “the patient has been placed in an induced coma.” This is not entirely true - the patient is under anesthesia, but not in an “induced coma”. Why do we give anesthesia? Firstly, if you or your relative end up in intensive care, it is not at all necessary that he will be there under anesthesia, but for seriously ill patients - yes, we really do provide anesthesia.
The goal is to help the patient cope with all disorders in the body, because in order to be conscious he needs to consume a lot of energy. In this case, it is simply a medical procedure. This is a guided medical intervention that makes breathing muscles and other organs easier to work with. This state can be maintained for as long as desired.
After extensive operations (for example, on the heart, lungs, with massive injuries), patients are definitely transferred for further treatment to prolonged mechanical ventilation. After relatively short and simple operations (up to an hour), it doesn’t matter if the anesthesiologist sees that at the end of the operation there is no restoration of elements of consciousness, attempts to breathe, interruptions in cardiac activity, pressure changes are observed, also for confidence and safety, the anesthesiologist transfers the patient to intensive care.
Do not be alarmed if, after surgery, a person is transferred to intensive care - there the patient is under the strict control of doctors and monitoring systems, and there is very good care there.
How long does an induced coma last?
The duration of drug-induced sleep is different for each patient and depends on the initial severity of his condition and diagnosis. Since the likelihood of complications directly depends on the duration of the induced coma, doctors try to reduce its duration as much as possible.
In most cases, the patient is put into medicated sleep for several hours or days. Less commonly, a medically induced coma can last up to several months.
Why aren't relatives allowed there?
They are allowed, but very rarely. Basically, doctors are really against relatives coming there.
Firstly, this is a very difficult sight for an unprepared person and we don’t know how he will behave there.
In the department (in one room) there are different patients, of varying severity, without clothes, equipment, sensors, alarming sounds all around. This is not a place where you need to come, sit, communicate. (even though this is how they usually show it in films). The doctor must always be ready - after all, at any moment a situation may arise when it is necessary to urgently resuscitate a patient who is there, no one needs the presence of strangers,
We also recommend reading: Jugular vein
Secondly, there is the risk of infection. Yours will be even higher than the patients there.
If you are admitted to intensive care
If you have received approval to go to see your relative who is in serious condition in intensive care, then try to follow some rules; I can’t call them simple, because... I understand that for an ordinary person this is a stressful situation.
- Prepare mentally and tune in to what you will see there (think several times whether it’s really worth going there - are you ready to see your loved one in a completely different form).
- If you are impressionable, you should avoid visiting;
- Do not bring anything from home (medicines, food) - this can be fatal for the patient;
- Communicate quietly, you are not alone in the department;
- Be polite to medical staff and try to listen to their advice.
Why is an induced coma dangerous?
The most common complications of an induced coma are bedsores. In order to avoid their development, the patient’s relatives and medical personnel must periodically change the position in which the patient is, give him a gentle massage, and carefully monitor skin hygiene.
Attention. Due to muscle relaxation, lack of consciousness and impaired swallowing, an induced coma can be complicated by severe aspiration pneumonia associated with the reflux of gastric contents into the lungs.
It is also possible to develop:
- laryngeal stenosis and pulmonary edema (against the background of constant mechanical ventilation (artificial ventilation));
- acute cardiovascular failure;
- collapse;
- renal failure;
- infectious and inflammatory processes in internal organs;
- sepsis.
After the patient is brought out of a medically induced coma, there may be a temporary decrease in memory, impaired speech and motor activity, and lethargy.
The duration of the rehabilitation period in this case will depend on the duration of the induced coma and the severity of the resulting disorders.
For reference. It should be noted that during the first year after drug-induced sleep, approximately every 10 patient manages to return to normal life. In other cases, the period of complete recovery takes a longer period of time.
Care of patients in intensive care
The intensive care unit has pretty good care (of course, there are cases when it is not always possible to carry out everything in full and the reason is trivial - lack of staff).
- prevention of bedsores is carried out (massage of the back and other protruding places, where bedsores often begin), nurses must turn the patient over at certain intervals;
- postural drainage is done (this is a complex of actions - tapping, stroking, etc. to remove stagnant fluid (mucus, sputum) from the respiratory tract;
- tube feeding for those who cannot swallow on their own;
- Intravenous infusion of solutions, vitamins;
- Patients have their nails cut, their face and body wiped, and in general all necessary hygiene procedures are carried out.
Severity of patients in intensive care
In any case, the definition of a condition is a rather subjective assessment of the doctor, but it is customary to distinguish the following conditions by severity:
- Satisfactory condition - in this case the patient is not transferred to intensive care, and if he was there, he is discharged and observed in a regular ward. The patient's life is not in danger. The disease occurs in a mild form, or the process of recovery begins.
- Moderate severity - in this case, the signs of the disease appear quite pronounced, a decision may be made to transfer to intensive care for more careful monitoring of vital signs. There may be fever, weakness, and pallor, but the person is conscious.
- Severe - the condition is defined as severe if there is depression of consciousness, sometimes the person may become delirious, fever, pale skin, cyanosis, the person cannot care for himself. If you are told that your condition is stable and serious, what does this mean? This means that the patient is not showing signs of improvement.
- Extremely severe - a life-threatening condition, the person is unconscious, pale skin, cold sweat is possible.
That's probably all on this topic, if you still have questions, you can ask me in the form below. Be healthy.
Coma state
During a medically induced coma, the following occurs:
- slow breathing;
- decreased heart rate;
- reduction in blood and intracranial pressure;
- muscle relaxation;
- decrease in body temperature;
- slowing down metabolic processes in tissues;
- vasoconstriction;
- decreased kidney function;
- decrease in the amount of fluid in the body;
- decrease in cerebral blood flow rate.
Another indicative manifestation of drug-induced sleep is the patient’s lack of consciousness.
For reference. Breathing during an induced coma is supported by a ventilator.