The cessation of cardiac and respiratory activity leads to a state of clinical death. It defines a short, reversible period between life and death. First aid provided in case of cardiac arrest within seven minutes allows you to return a person to normal existence.
This is possible because irreversible phenomena in brain cells due to hypoxia have not yet occurred. The lost functions are taken over by the remaining undamaged neurons.
You can learn more about the mechanisms of clinical death from this article.
Clinical experience shows that the period of clinical death is individual and can last from two to 15 minutes. And if hypothermia is used (artificial cooling to 8–10 degrees), it extends to two hours.
If cardiac arrest is recorded in a hospital, then doctors certainly have enough skills and resuscitation equipment to take immediate action to save the patient. There is special honey for this. staff of intensive care and resuscitation departments.
However, the place of assistance in the event of sudden death can be a work office, an apartment, a street, or any uncrowded room. Here, a person’s life depends on events carried out by random passers-by and witnesses.
How to give first aid
Every adult should be able to provide emergency first aid. It must be remembered that you only have 7 minutes for all actions. This is a critical period for restoring cerebral circulation. If the victim can be saved later, he faces complete disability.
Those around us are faced with a difficult task:
- provide, using indirect cardiac massage, an imitation of contractions to temporarily support the blood flow system;
- restore spontaneous breathing.
The sequence of actions depends on the number of people taking part in providing assistance. Two will do it faster. In addition, someone should call an ambulance and note the time.
- First you need to make sure that nothing in your mouth can interfere with breathing, clean the oral cavity with your finger, straighten your tongue;
- put the victim on a hard surface (ground, floor), tilt his head back;
- hit the sternum with a fist (a precordial blow can immediately “start” the heart);
- Heart massage is done by jerky pressure on the sternum, keeping your arms straight and resting them on the patient’s chest;
- At the same time, artificial respiration is carried out in the classical way “mouth to mouth” or “mouth to nose”; when breathing into the mouth, you need to pinch your nose with your fingers; it is important to hold the victim’s lower jaw with your hand, pushing it slightly forward (to prevent the tongue from retracting).
The massage continues until cardiac activity is restored and facial skin color returns to normal.
It is recommended to take passive “breaths” after every four compressions on the sternum. For hygienic purposes, a thin scarf or gauze can be applied to the victim’s face.
If the chest begins to rise on its own, it means that your own breathing has appeared. But if the pulse begins to be felt, and there are no respiratory movements, only artificial respiration should be continued.
The critical period for resuscitation is considered to be 20 minutes. After this, the biological stage of death is stated.
The arriving ambulance team will continue resuscitation measures.
GBUZ NO "Pavlovsk Central District Hospital"
Emergency care for acute life-threatening conditions
In our country, up to 80% of deaths occur outside of medical organizations - at home, at work, in the country, in public and other places. Most of them occur suddenly or by the mechanism of sudden death. Statistics show that many patients (or their relatives) call an emergency doctor late, which reduces the likelihood of rescue.
By mastering the necessary first aid skills in the form of self- or mutual assistance (on the part of people surrounding a person who finds himself in such a critical condition), in most cases the patient’s life can be saved.
Often, up to 30-50%, a life-threatening complication with a dangerous fatal outcome may be the first and last manifestation of these diseases (complications).
FIRST AID for a heart attack
Characteristic signs (symptoms) of a heart attack (myocardial infarction):
• sudden (paroxysmal) pressing, squeezing, burning, aching pain in the chest (behind the sternum) lasting more than 5 minutes;
• similar pains are often observed in the left shoulder (forearm), left shoulder blade, left half of the neck and lower jaw, both shoulders, both arms, the lower part of the sternum along with the upper abdomen;
• lack of air, shortness of breath, severe weakness, cold sweat, nausea often occur together, sometimes follow or precede discomfort/pain in the chest; often these manifestations of the disease develop against the background of physical or psycho-emotional stress, but more often with some interval after them.
Uncharacteristic signs that are often confused with a heart attack:
• stabbing, cutting, pulsating, boring, constant aching pain for many hours and not changing its intensity in the heart area or in a specific clearly defined area of the chest
Algorithm of emergency actions in case of a heart attack (advice to the patient) - a reminder for the patient
If you or someone else suddenly has the above characteristic signs of a heart attack, even with weak or moderate intensity, which last more than 5 minutes, do not hesitate, immediately call an ambulance team. Do not wait more than 10 minutes - in such a situation it is life-threatening.
Remember that being intoxicated in this life-threatening situation is not a reasonable excuse for delaying calling an ambulance. If you have symptoms of a heart attack and there is no way to call an ambulance, then ask someone to take you to the hospital - this is the only right decision. Never drive yourself unless you have no other choice.
In the most optimal scenario, if a heart attack occurs, you must follow the instructions received from your attending physician; if there are no such instructions, then you must act according to the following algorithm:
• Immediately after an attack occurs, sit down (preferably in a chair with armrests) or lie down in bed with the head of the bed raised, take 0.25 g of acetylsalicylic acid (aspirin) (chew the tablet, swallow) and 0.5 mg of nitroglycerin (spray one inhalation dose into the cavity mouth while holding your breath, place one tablet/capsule under the tongue, first bite the capsule, do not swallow); free your neck and provide fresh air (open the vents or windows).
• If after 5-7 min. After taking acetylsalicylic acid (aspirin) and nitroglycerin, pain persists, it is imperative (life-saving) to call an ambulance and take nitroglycerin a second time.
• If pain persists 10 minutes after taking the second dose of nitroglycerin, it is necessary to take nitroglycerin a third time.
• If after the first or subsequent doses of nitroglycerin there is severe weakness, sweating, shortness of breath, you need to lie down, raise your legs (on a bolster, etc.), drink 1 glass of water and then, as with a severe headache, do not take nitroglycerin.
• If the patient has previously taken medications that lower cholesterol levels in the blood from the statin group (simvastatin, lovastatin, fluvastatin, pravastatin, atorvastatin, rosuvoastatin), give the patient his usual daily dose and take the drug with you to the hospital.
Attention ! A patient with a heart attack is strictly forbidden to get up, walk, smoke or eat until the doctor’s special permission;
You should not take aspirin (acetylsalicylic acid) if you are intolerant to it (allergic reactions), as well as with obvious or worsening peptic ulcers of the stomach and duodenum;
Nitroglycerin should not be taken if there is severe weakness, sweating, or if there is severe headache, dizziness, or acute impairment of vision, speech, or coordination of movements.
FIRST AID for acute cerebrovascular accident
The main signs (symptoms) of acute cerebrovascular accident:
• numbness, weakness, “disobedience” or paralysis (immobilization) of an arm, leg, half of the body, distortion of the face and/or drooling on one side;
• speech disorders (difficulties in choosing the right words, understanding speech and reading, slurred and unclear speech, up to complete loss of speech);
• disturbances or loss of vision, double vision, difficulty focusing;
• imbalance and coordination of movements (feelings of “swaying, sinking, body rotation, dizziness”, unsteady gait up to falling);
• unusual severe headache (often after stress or physical exertion);
• confusion or loss of consciousness, uncontrollable urination or bowel movements.
If any of these signs suddenly appear, call an ambulance immediately, even if these manifestations of the disease were observed for only a few minutes
Patient Reminder
1. Call an ambulance immediately, even if these manifestations of the disease were observed for only a few minutes
2. Before the arrival of the emergency medical team:
• If the patient is unconscious, place him on his side, remove removable dentures (food debris, vomit) from the mouth, make sure that the patient is breathing.
• If the victim is conscious, help him to a comfortable sitting or semi-sitting position in a chair or on a bed, placing pillows under his back. Provide fresh air. Unbutton your shirt collar, belt, waistband, and remove tight clothing.
• Measure your blood pressure if its upper level exceeds 220 mmHg. Art., give the patient a drug that lowers blood pressure, which he took before.
• Measure your body temperature. If the temperature is 38° or more, give the patient 1 g of paracetamol (2 tablets of 0.5 g, chew, swallow), (if paracetamol is not available, do not give other antipyretic drugs!).
• Put ice on your forehead and head, you can take food from the freezer, put in waterproof bags and wrapped in a towel.
• If the patient has previously taken medications that lower cholesterol levels in the blood from the statin group (simvastatin, lovastatin, fluvastatin, pravastatin, atorvastatin, rosuvastatin), give the patient the usual daily dose.
• If the victim has difficulty swallowing and saliva drips from his mouth, tilt his head towards the weaker side of the body and blot the dripping saliva with clean tissues.
• If the victim is unable to speak or has slurred speech, reassure and reassure him that the condition is temporary. Hold his hand on the non-paralyzed side, stop him from trying to talk, and don't ask questions that require an answer. Remember that although the victim cannot speak, he is aware of what is happening and hears everything that is said around him.
FIRST AID for hypertensive crisis
Hypertensive crisis is a condition manifested by high blood pressure (BP) (systolic or “upper” blood pressure, usually more than 180 mm Hg; diastolic or “lower” blood pressure - more than 100 mm Hg) and the following main symptoms:
• headache, often in the occipital region, or heaviness and noise in the head;
• flashing “flies”, a veil or a net before the eyes;
• nausea, feeling of exhaustion, overwork, internal tension;
• shortness of breath, weakness, constant monotonous aching pain/discomfort in the heart area, sometimes the appearance or increase of pastiness/swelling of the skin of the face, arms, legs.
Algorithm for emergency actions in case of hypertensive crisis
(advice to the patient) – a reminder for the patient
If symptoms of a hypertensive crisis appear, you must:
• remove bright light, ensure peace, access to fresh air (unbutton your shirt collar, ventilate the room, etc.);
• measure blood pressure (see the method for measuring blood pressure at the end of this section) and if its “upper” level is higher than or equal to 160 mm Hg, you must take an antihypertensive drug previously recommended by your doctor. In the absence of an antihypertensive drug recommended by a doctor or when a blood pressure level is registered above 200 mm Hg. urgently need to call an ambulance.
• before the arrival of emergency medical services, it is necessary, if possible, to sit in a chair with armrests and take a hot foot bath (put your feet in a container of hot water).
Attention! A patient with a hypertensive crisis is prohibited from any sudden movements (suddenly standing up, sitting down, lying down, bending over), pushing hard or any physical activity.
• 40-60 minutes after taking the medicine recommended by the doctor, it is necessary to re-measure blood pressure and if its level has not decreased by 20-30 mm Hg. from the initial state and/or the condition has not improved - urgently call an ambulance.
• If you feel better and your blood pressure decreases, you need to rest (lie in bed with the head of the bed raised) and then contact your local (family) doctor.
When talking with your doctor, you need to clarify which medications you need to take if a hypertensive crisis develops, clearly write down their names, dosage and time sequence (algorithm) for taking them, and also check with your doctor for what manifestations of the disease you need to urgently call an ambulance.
All patients with hypertension need to create an individual mini-first aid kit for a hypertensive crisis and carry it with them at all times, since a hypertensive crisis can develop at any time and anywhere.
FIRST AID for acute heart failure
Acute heart failure (AHF) is a severe pathological condition that develops in patients with various heart diseases and hypertension. This is one of the most common reasons for calling an ambulance and hospitalization of patients, as well as mortality in our country and around the world.
The main manifestations (symptoms) of acute heart failure are:
• heavy, frequent (more than 24 per minute) noisy breathing - shortness of breath, sometimes reaching the level of suffocation, with predominant difficulty in inhaling and a clear increase in shortness of breath and cough in a horizontal position. A sitting position or a lying position with the head of the head raised up alleviates the patient's condition;
• often when breathing, wet, squelching wheezing/sounds, interrupted by coughing, become audible; in the terminal stage, breathing takes on a bubbling character with the appearance of foam at the patient’s mouth;
• characteristic sitting posture of the patient, resting his straight arms on his knees or on the seat (to facilitate breathing)
Acute heart failure can develop very quickly and lead to the death of the patient within 30-60 minutes. In most cases, 6-12 or more hours pass from the first clinical signs to severe manifestations of AHF, but without medical care, the vast majority of patients with AHF die.
Algorithm of emergency actions for acute heart failure
(advice to the patient) – a reminder for the patient
When the above symptoms of AHF appear in patients with hypertension or heart disease (but not the lungs or bronchi), it is necessary:
• call an ambulance
• give the patient a sitting position, preferably in a chair with armrests on which he can lean and engage the intercostal muscles in the act of breathing
• provide physical and psycho-emotional peace and fresh air by ventilating the room
• place your feet in a large container (basin, tank, bucket, etc.) with hot water
• in extremely severe cases, tourniquets are applied to the legs in the groin area, compressing the superficial veins, but not the deep arteries, which reduces blood flow to the heart and thereby facilitates its work
If the patient or the person providing first aid has experience in the use of nitroglycerin, it is prescribed in a dose of 0.4 (0.5) mg (inhalation into the oral cavity is carried out under the root of the tongue, the tablet/capsule is placed under the tongue, the capsule must first be bitten, do not swallow). If the patient’s well-being improves after using nitroglycerin, it is reapplied every 10-15 minutes until the arrival of the emergency medical team. If there is no improvement in the patient’s well-being after the next dose of nitroglycerin, it is no longer used.
Attention! A patient with AHF must exclude all physical activity; it is strictly forbidden to walk, smoke, drink water and take liquid food until special permission from the doctor; Nitroglycerin should not be taken if blood pressure is less than 100 mm Hg. with severe headache, dizziness, acute impairment of vision, speech or coordination of movements.
All patients with hypertension or heart disease with shortness of breath and swelling in the legs should discuss with their doctor what medications should be taken if AHF develops, clearly write down their names, dosage and time sequence (algorithm) for taking them, and also check with the doctor for which manifestations of the disease, it is necessary to urgently call an ambulance.
Each such patient needs to create an individual first aid kit for AHF and constantly have it with him.
FIRST AID for sudden death (advice to eyewitnesses)
Most often, sudden death occurs due to cardiac arrest.
activities.
The main signs (symptoms) of sudden death:
• Sudden loss of consciousness, often accompanied by agonal movements (a standing or sitting person falls, convulsive muscle tension, involuntary urination and defecation are often observed; a lying person sometimes makes a convulsive attempt to sit up or turn on his side)
• Sudden complete cessation of breathing, often after a short period (5-10 seconds) of agonal pseudobreathing: the patient makes wheezing and/or gurgling sounds, sometimes similar to a convulsive attempt to say something.
Algorithm for urgent actions of eyewitnesses to the sudden death of a person
• If a person suddenly loses consciousness, immediately call an ambulance team (if there are other people nearby, they call an ambulance). Next, shake the patient by the shoulder and ask loudly, “What’s wrong with you?” If there is no response, active patting is performed on the patient’s cheeks; if there is no reaction, immediately begin closed cardiac massage.
• The patient is placed on a hard, flat surface (floor, ground, flat hard area and similar places, but not on a sofa, bed, mattress and other soft surfaces), and the front part of the chest is freed from clothing. Determine the location of the hands on the patient’s chest as indicated in the figure. One palm is placed in the place indicated in the figure, and the palm of the second hand is placed on top of the first in exact accordance with the image of the hands in the figure.
Rice. Illustration of the technique of closed cardiac massage
• With straight arms (not bent at the elbows), vigorous rhythmic compression of the victim’s chest is performed to a depth of 5 cm with a frequency of 100 compressions on the chest per minute
• When signs of life appear (any reactions, facial expressions, movements or sounds made by the patient), cardiac massage must be stopped. If these signs of life disappear, heart massage must be resumed. Stops of cardiac massage should be minimal - no more than 5-10 seconds. When signs of life resume, the heart massage stops, and the patient is provided with warmth and peace. If there are no signs of life, cardiac massage continues until the arrival of an emergency medical team.
If the first aid provider has special training and experience in performing cardiopulmonary resuscitation, he can perform artificial ventilation in parallel with closed cardiac massage. In the absence of special training, artificial ventilation of the lungs and determination of the pulse in the carotid artery should not be performed on the patient, since special scientific studies have shown that such procedures in inexperienced hands lead to an unacceptable loss of time and sharply reduce the frequency of revival of patients with sudden cardiac arrest.
remember, that
- emergency medical care only called in the first 10 minutes from the onset of a heart attack or stroke allows full use of modern highly effective methods of inpatient treatment and many times reducing mortality from these diseases
- acetylsalicylic acid (aspirin) and nitroglycerin taken in the first minutes can prevent the development of myocardial infarction and significantly reduce the risk of death from it
- state of alcohol intoxication is not a reasonable basis for delaying calling an ambulance in the event of a heart attack and acute cerebrovascular accident - about 30% of people who suddenly (within an hour from the onset of symptoms) died at home were intoxicated.
- closed cardiac massage performed in the first 60-120 seconds after sudden cardiac arrest allows up to 50% of patients to be brought back to life.
Print Email
What can emergency doctors do?
At the ambulance stage, first aid is provided in case of cardiac arrest.
Ventilation of the lungs is carried out through a mask using an Ambu bag. To achieve full contact with the trachea and press the tongue, intubation is performed or a special tube is inserted, connecting it to the bag. Compression achieves the supply of air mass into the lung tissue.
If special equipment is available, the heart is defibrillated with an electric current.
The effect of the discharge can be enhanced by the administration of Adrenaline and Atropine. These are drugs that sharply increase myocardial excitability. After their introduction intracardially, a second attempt at defibrillation is made.
In the absence of a defibrillator, indirect massage continues.
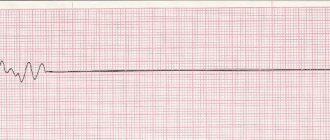
In a car with an ECG device, it is possible to take an electrocardiogram, at least a single lead. It can be used to judge the presence of asystole or fibrillation.
Possible causes of cardiac arrest
Poor general health and atmospheric pressure can play a bad joke on heart patients, but there are other factors that can stop the heart muscle from working.
- First aid algorithm for cardiac and respiratory arrest
Figure 3. What is Thrombosis
Cardiac arrest, causes:
- Coronary circulation disorders caused by excessive physical exertion or severe emotional shock;
- Poisoning and serious breathing problems;
- Acute allergic reactions, anaphylactic shock;
- Thrombosis (Figure 3), stroke and heart attack.
Sudden cardiac arrest can also be caused by other external influences on the human body:
- Mechanical injuries of the chest;
- Heavy blood loss of large volumes;
- Heat or sunstroke (Figure 4);
- Electric current discharge;
- By drowning or suffocation.
Figure 4. External factors that may cause cardiac arrest.
It is important to know and take into account which drugs cause cardiac arrest, these include:
- Beta blockers - bisoprolol, atenolol, bisoprolol and calcium antagonists - verapamil, diltiazem - they lower blood pressure, but they are strictly forbidden to be taken by those whose pulse is equal to or below 60 beats per minute; they are prescribed by doctors only for hypertension;
- Antibacterial agents - roxithromycin, azithromycin, related to macrolides - these antibiotics double the risk of tachycardia and can contribute to sudden death; they are not suitable for the elderly and those who suffer from heart disease.
All drugs that cause cardiac arrest can be divided into seven main groups:
- Antibiotics;
- Cardiac glycosides;
- Muscle relaxants;
- Potassium;
- Psychotropic drugs (Figure 5);
- Tablets and mixtures for heartburn;
- Vitamins. Figure 5. Drugs and antidepressants can cause cardiac arrest.
After delivering the patient to the hospital
If the heart rhythm is successfully restored, urgent measures are taken to stabilize contractions and eliminate the metabolic consequences of clinical death.
The patient is placed in the intensive care unit.
It is connected to a heart rate monitor. This is important because restored heart contractions are prone to changes in rhythm and various disturbances. Antiarrhythmic drugs help compensate for them.
An alkaline solution must be injected drip-wise to eliminate acidosis.
In the hospital, it is possible to conduct an examination and identify the cause of cardiac arrest.
In case of fluid compression and cardiac tamponade, pericardiocentesis is immediately performed with pumping out the exudate. If pneumothorax is detected, installing a drainage to expand the lung helps.
If spontaneous breathing is shallow and congestive wheezing is heard in the lower parts of the lungs, the patient is intubated and transferred to artificial mechanical ventilation with increased oxygen supply
Causes and symptoms
Due to the fact that the heart suddenly stops beating, people of pre-retirement age most often die if they do not receive help. Risk factors for cessation of contractions are the following pathologies:
- pathologies of the circulatory system. Violations may be associated with stress, increased physical activity;
- respiratory problems;
- anaphylactic shock;
- stroke or heart attack;
- the appearance of blood clots.
Timely actions will help avoid complications, but the heart may stop beating due to external factors. These include mechanical damage to the chest area, electric shock, as well as thermal or solar damage, and large blood loss.
You can begin first aid for sudden cardiac arrest if you have the following symptoms of clinical death:
The person stops breathing.
- the person suddenly loses consciousness. At the same time, they note the lack of reaction to any stimuli;
- the pulse disappears. To check for its presence, you need to place two fingers on the carotid artery in the neck;
- the victim is not breathing. This can be understood by the fact that the chest does not move;
- the pupils become wide, and there is no reaction to light;
- the skin becomes pale and may acquire a bluish tint.
If these symptoms are present, then a stop has occurred. It is imperative to call emergency doctors, and before they arrive, try to start the heart on your own.
Examples of specific situations and algorithm for diagnosis and action
To analyze the cases that medical workers and people far from medicine have to deal with, let’s look at examples of situations that allow you to think about your role in resuscitation.
Situation one
The young man fell in front of the employees, without even having time to let go of the briefcase with documents. A lot of people gathered around and they called an ambulance. While waiting for the doctors, everyone groans and remembers various cases of illness from their experience. The result was that the patient died, and the ambulance doctor could only note signs of biological death.
Unfortunately, a similar situation often arises anywhere. When people, instead of taking active pre-medical actions, panic, get lost, and miss time for resuscitation.
And some even start talking about the “prohibition of approaching the corpse until the police arrive.” Who said that the victim is already a corpse? Has anyone even dared to check your pulse and pupils? Such a death remains on the conscience of the crowd.
Imagine that you or your loved ones might find yourself in a similar situation
Situation two
A woman was seen lying on the street with rare breathing movements, unconscious, and her pulse could not be determined. Passers-by called an ambulance. They started doing chest compressions and assisted breathing.
The result is that before the team arrived, it was possible to maintain blood circulation “manually,” which slowed down irreversible changes and reduced hypoxia.
Often people begin to doubt the need for chest compressions due to assumptions about fainting or a stroke. There is very little time left for doubt. When fainting, the pulse is preserved, the pupils react to light. With a stroke, facial asymmetry, changes in the tone of the limbs on one side, and pupils of different widths are possible. The pulsation is also preserved.
Situation three
Ambulance doctors received a call for the cardiology team because the caller correctly described the victim’s symptoms.
Having loaded the patient onto a gurney, she was wheeled into the car; the intensive care vehicle has technical equipment for all activities
The algorithm of actions has been worked out in practice:
- the tongue is attached to the lower jaw with a special curved air duct tube, an Ambu bag for manual artificial respiration is attached to it;
- Adrenaline solution was injected intracardially with a long needle;
- in the absence of pulsation in the carotid and femoral arteries, if heart sounds cannot be heard, defibrillation is indicated;
- indirect massage and artificial respiration last 20 minutes.
During this time, the car reaches the hospital and the question of the advisability of continuing resuscitation measures is decided.
Situation four
Cardiac arrest occurred during intestinal surgery. The anesthesiologist noticed a sudden drop in blood pressure in a patient under anesthesia, and cardiac activity stopped on the monitor. Surgeons note blanching of the internal organs and mesentery.
Algorithm of actions:
- the surgical intervention is terminated;
- Adrenaline solution is injected into the subclavian vein;
- defibrillation is performed;
- in the absence of restoration of heart contractions, the discharge is repeated;
- between shocks, a soda solution is injected in a stream to prevent acidosis;
- the surgeon opens the diaphragm, inserts his hand into the chest cavity and manually massages the heart, squeezing and unclenching it.
The technique is called direct cardiac massage, it is possible with an open chest or from the abdominal cavity
The success of the measures is judged by the resumption of the rhythm on the monitor and the increase in pressure.
Surgeons notice the beginning of bleeding in the wound. The operation ends with minimal mechanical damage after the break. The diaphragm is sutured.
How to evaluate the effectiveness of cardiac massage?
The effectiveness of cardiac massage is assessed according to the following criteria:
- the appearance of a pulse in the carotid, femoral and radial arteries;
- increase in blood pressure to 60–80 mm Hg;
- constriction of the pupils and the appearance of their reaction to light;
- disappearance of bluish color and “deadly” pallor;
- restoration of spontaneous breathing.
If, after 30–40 minutes from the start of cardiac massage, artificial respiration and drug therapy, cardiac activity is not restored, the pupils remain wide, without reaction to light, it can be considered that irreversible changes and brain death have occurred in the body, and it is advisable to stop resuscitation. If obvious signs of death appear (link to card), resuscitation may be stopped earlier.
Alternative resuscitation
The experience accumulated in different countries in resuscitation measures during cardiac arrest allows us to choose the most effective methods. Research in recent years has established the priority of cardiac mechanisms of clinical death (90% of cases) against the background of an intact respiratory system. Therefore, doubts arose about the need for emergency measures to restore breathing.
The state of Arizona uses the MICR methodology. She suggests doing several more intense cycles of chest compressions without mouth-to-mouth breathing.
The rules provide:
- in the first 2 minutes of resuscitation, mandatory 100 chest compressions per minute (200 in total);
- then pulse control, administration of Adrenaline and defibrillation;
- repeat this way 2 more times;
- only after this is tracheal intubation and artificial respiration performed.
The authors excluded cardiac arrest due to noncardiac causes (trauma, drowning) from the studies.
The technique is used by paramedics and firefighters. Comparison of effectiveness in terms of patient survival occurred only in out-of-hospital cases of clinical death. As a result, the percentage of those resuscitated increased from 1.8 (using classical methods of massage and artificial respiration) to 5.4.
The program was included in the recommendations of the Cardiological Association in the USA.
The UNIVERSAL algorithm (named after the first letters of the stages) has been published in Russia and is used by many. In it, artificial ventilation is placed in third place in the step-by-step actions after the precordial stroke and the beginning of chest compressions. For inpatient conditions, pacing is recommended by introducing an electrode into the heart cavity through a subclavian catheter.
How are the consequences of clinical death corrected?
If help is late, then it is not possible to fully restore body functions. The brain suffers the most. A person loses intelligence and memory. Failure is possible after forced hypoxia of the kidneys and liver. It's impossible to fix anything.
Is life necessary in exchange for intelligence? There is no solution to the problem yet
During early recovery, the patient receives long-term maintenance therapy with antiarrhythmic drugs and nootropic drugs for brain cells. He is periodically examined by doctors (a cardiologist and a neurologist) and carried out a follow-up examination. In the absence of complications, the patient can return to work subject to restrictions (physical activity, night shifts, stressful situations, hypothermia are contraindicated).
You should always remember the limited ability of internal organs to restore damaged functions, especially the brain and heart. Nature gave man the opportunity to use them once. Not everyone gets a second chance.