Features for various diseases
Painful sensations may have characteristics depending on the disease that causes them.
Myocardial infarction
Poor blood supply to the heart muscle can cause its necrosis, which is manifested by the following symptoms:
- burning sharp pain;
- the attack lasts more than half an hour;
- additional symptoms are present (shortness of breath, nausea, panic and sweating);
- the pain radiates to the left side of the body.
IMPORTANT! With such signs, the patient urgently calls an ambulance, since the opportunity to stabilize the condition will only be 2 hours.
Angina pectoris
Severe pressing pain syndrome. This sensation occurs after a certain amount of tension and persists for half an hour. The main symptom is relief after taking nitroglycerin.
Myocarditis
The condition is characterized by inflammation of the heart muscle, aching pain occurs periodically. The more inflammation spreads, the longer and more intense the pain.
Valve damage
Pain sensations differ in localization (it all depends on the degree of damage to the valves). Usually the pain is aching and dull, occurring periodically, at the same time the heart rate becomes erratic and shortness of breath begins.
Cardiomyopothia
The pathological process is accompanied by contracting, pulling pains, the precise localization of which is difficult to determine. It is not always possible to relieve the syndrome with nitroglycerin.
Heart and blood vessels
The human cardiovascular system is closed. This means that the blood moves only through the vessels and there are no cavities into which the blood flows. Thanks to the work of the heart and the branched system of blood vessels, every cell in our body receives oxygen and nutrients that are necessary for life.
Pay attention to the established name - cardiovascular system. The first place is taken by the heart muscle, which performs the most important function. We move on to studying this unique organ.
Heart
The branch of medicine that studies the heart is called cardiology (from the ancient Greek καρδία - heart and λόγος - study). The heart is a hollow muscular organ that contracts with a certain rhythm throughout a person’s life.
The outside of the heart is covered by a pericardial sac - the pericardium. Consists of 4 chambers: 2 ventricles - right and left, and 2 atria - right and left. Remember that between the ventricles and atria there are leaflet valves.
Between the right atrium and the right ventricle there is a tricuspid (tricuspid) valve, and between the left atrium and the left ventricle there is a bicuspid (mitral) valve.
In the heart, blood moves unidirectionally: from the atria to the ventricles, thanks to the presence of leaflet (atrioventricular) valves (from the Latin atrium - atrium and ventriculus - ventricle).
The largest human vessel, the aorta, with a diameter of 2.5 cm, departs from the left ventricle, in which blood flows at a speed of 50 cm per second. The pulmonary trunk departs from the right ventricle. Between the left ventricle and the aorta, as well as the right ventricle and the pulmonary trunk, there are semilunar valves.
The muscle tissue of the heart is represented by single cells - cardiomyocytes, which have transverse striations. The heart has a special property - automaticity: isolated from the body, the heart continues to contract without external influences. This is due to the presence of special cells in the thickness of muscle tissue - pacemaker cells (pacemaker cells, atypical cardiomyocytes), which themselves periodically generate nerve impulses.
The heart has a conduction system due to which the excitation that arises in one part of the heart gradually covers other parts. The conduction system includes the sinus node, atrioventricular node, His bundle and Purkinje fibers. It is thanks to the presence of these conducting structures that the heart is capable of automation.
Cardiac cycle
The work of the heart consists of three phases successively replacing each other:
- Atrial systole (from the Greek systole - compression, contraction)
- Ventricular systole
- Total diastole (from the Greek diastole - expansion)
Lasts 0.1 sec. During this phase, the atria contract, their volume decreases, and blood flows from them into the ventricles. During this phase, the leaflet valves are open, the semilunar valves are closed.
Lasts 0.3 seconds. The leaflet (atrioventricular) valves close to prevent blood from flowing back into the atria. The muscle tissue of the ventricles begins to contract, their volume decreases: the semilunar valves open. Blood is expelled from the ventricles into the aorta (from the left ventricle) and the pulmonary trunk (from the right ventricle).
Lasts 0.4 seconds. In diastole, the cavities of the heart expand - the muscles relax, the semilunar valves close. Flap valves are open. During this phase, the atria fill with blood, which passively flows into the ventricles. Then the cycle repeats.
We have already discussed the cardiac cycle, but I want to focus your attention on some details. In total, one cycle lasts 0.8 seconds. The atria rest for 0.7 seconds during ventricular systole and total diastole, and the ventricles rest for 0.5 seconds during atrial systole and total diastole. Thanks to this energetically beneficial cycle, the heart muscle gets less tired during work.
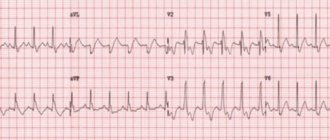
Heart rate (HR) can be measured using the pulse - the jerky vibrations of the walls of blood vessels associated with the cardiac cycle. The normal average heart rate is 60-80 beats per minute. An athlete's heart rate is lower than that of an untrained person. With heavy physical exertion, heart rate can increase to 150 beats/min.
Changes in the heart rate are possible in the form of its excessive slowdown or increase, respectively, they are distinguished: bradycardia (from the Greek βραδυ - slow and καρδιά - heart) and tachycardia (from the ancient Greek ταχύς - fast and καρδία - heart). Bradycardia is characterized by a decrease in heart rate to 30-60 beats/min, tachycardia - above 90 beats/min.
The regulatory center of activity of the cardiovascular system lies in the medulla oblongata and spinal cord. The parasympathetic nervous system slows down and the sympathetic nervous system speeds up heart rate. Humoral factors also have an influence (from the Latin humor - moisture), mainly hormones: adrenal glands - adrenaline (strengthens the heart), thyroid gland - thyroxine (accelerates heart rate).
Vessels
Blood moves to tissues and organs inside the vessels. They are divided into arteries, veins and capillaries. We will discuss their structure and functions in general terms. I would like to note: if you think that venous blood flows through the veins and arterial blood flows through the arteries, you are mistaken. In the following article you will find specific examples that refute this misconception.
Arteries carry blood from the heart to internal organs and tissues. They have thick walls containing elastic and smooth muscle fibers. The blood pressure in them is the highest compared to the veins and capillaries, which is why they have the aforementioned thick wall.
The inside of the artery is lined with endothelium - epithelial cells that form a single layer of thin cells. Due to the presence of smooth muscle cells in the thickness of the wall, arteries can narrow and widen. The speed of blood flow in the arteries is approximately 20-40 cm per second.
For the most part, arteries carry arterial blood, but we must not forget about exceptions: venous blood flows from the right ventricle through the pulmonary arteries to the lungs.
Veins carry blood to the heart. Compared to the arterial wall, veins have fewer elastic and muscle fibers. The blood pressure in them is low, so the wall of the veins is thinner than that of the arteries.
A characteristic sign of veins (which you will always notice on the diagram) is the presence of valves inside the vein. The valves prevent the reverse flow of blood in the veins - they ensure unidirectional blood flow. The speed of blood flow in the veins is about 20 cm per second.
Just imagine: veins lift blood from the legs to the heart, acting against gravity. The aforementioned valves and skeletal muscle contractions help them in this. That is why physical activity is very important, as opposed to physical inactivity, which is harmful to health by disrupting the movement of blood through the veins.
Mostly the veins contain venous blood, but we must not forget about exceptions: the pulmonary veins with arterial blood enriched with oxygen after passing through the lungs approach the left atrium.
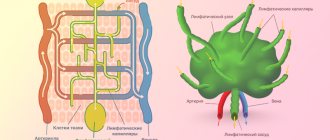
The smallest blood vessels are capillaries (from the Latin capillaris - hair). Their wall consists of a single layer of cells, which makes possible gas exchange and exchange processes of various substances (nutrients, by-products) between the cells surrounding the capillary and the blood in the capillary. The speed of blood movement through capillaries is the lowest (compared to arteries and veins) - 0.05 mm per second, which is necessary for metabolic processes.
The total lumen of capillaries is larger than that of arteries and veins. They are suitable for every cell of our body; they are the connecting link through which tissues receive oxygen and nutrients.
As blood passes through the capillaries, it loses oxygen and becomes saturated with carbon dioxide. Therefore, in the picture above you see that at first the blood in the capillaries is arterial, and then venous.
Hemodynamics
Hemodynamics is the process of blood circulation. An important indicator is blood pressure - the pressure exerted by blood on the walls of blood vessels. Its magnitude depends on the force of heart contraction and vascular resistance. There are systolic (on average 120 mm Hg) and diastolic (on average 80 mm Hg) blood pressure.
Systolic blood pressure refers to the pressure in the bloodstream at the moment of contraction of the heart, diastolic - at the moment of its relaxation.
With physical activity and stress, blood pressure rises and heart rate increases. During sleep, blood pressure decreases, as does your heart rate.
Blood pressure level is an important indicator for a doctor. Blood pressure may be elevated in a patient with kidney or adrenal disease, so it is extremely important to know and control its level.
Increased blood pressure, for example 220/120 mmHg. Art. doctors call arterial hypertension (from the Greek hyper - excessively; to say hypertension is not entirely correct, hypertension is increased muscle tone), and a decrease, for example, to 90/60 mm. rt. Art. will be called arterial hypotension (from the Greek hypo - under, below).
All of us have probably experienced orthostatic hypotension at least once in our lives - a decrease in blood pressure when suddenly rising from a sitting or lying position. It is accompanied by slight dizziness, but can also lead to fainting and loss of consciousness. Orthostatic hypotension can (within normal limits) occur in adolescents.
There is a nervous regulation of hemodynamics, which consists in the action on the vessels of fibers of the sympathetic nervous system, which constricts blood vessels (pressure increases), and the parasympathetic nervous system, which dilates blood vessels (pressure decreases accordingly).
The lumen of blood vessels is also affected by humoral factors that spread through the fluids of the body. A number of substances have a vasoconstrictor effect: vasopressin, norepinephrine, adrenaline, another part has a vasodilator effect - acetylcholine, histamine, nitric oxide (NO).
Diseases
Atherosclerosis (Greek athḗra - gruel + sklḗrōsis - hardening) is a chronic disease of the arteries that occurs as a result of a violation of the metabolism of fats and proteins in them. With atherosclerosis, a cholesterol plaque forms in the vessel, which gradually increases in size, ultimately leading to complete blockage of the vessel.
The plaque narrows the lumen of the vessel, reducing the amount of blood flowing through it to the organ. Atherosclerosis often affects the vessels that supply the heart - the coronary arteries. In this case, the disease may manifest itself as pain in the heart with minor physical exertion. If atherosclerosis affects the vessels of the brain, the patient’s memory, concentration, and cognitive (intellectual) functions deteriorate.
At some point, an atherosclerotic plaque may burst, in which case the incredible happens: the blood begins to clot right inside the vessel, because the cells react to the rupture of the plaque as if the vessel is damaged! A blood clot forms, which can block the lumen of the vessel, after which blood completely stops flowing to the organ that this vessel supplies.
This condition is called a heart attack (Latin infarcire - “to fill, stuff”) - a sudden cessation of blood flow due to artery spasm or blockage. A heart attack is expressed in the death of organ tissue due to an acute lack of blood supply. A cerebral infarction is called a stroke (Latin insultus - attack, blow).
© Bellevich Yuri Sergeevich 2018-2021
This article was written by Yuri Sergeevich Bellevich and is his intellectual property. Copying, distribution (including by copying to other sites and resources on the Internet) or any other use of information and objects without the prior consent of the copyright holder is punishable by law. To obtain article materials and permission to use them, please contact Yuri Bellevich
.
How to distinguish heart pain from neuralgia
Heart pain is often confused with neuralgic pain. Among the main characteristic symptoms of neuralgia are the following:
- the ability to determine a clear localization;
- unpleasant sensations are concentrated at one point;
- the nature of the pain is shooting, aching or stabbing;
- lasts for several days;
- the intensity of sensations does not depend on the time of day;
- worsens with twisting, sneezing or coughing, walking, palpation of intercostal areas;
- nitroglycerin is ineffective;
- the ability to breathe only superficially;
- often occurs after hypothermia;
- accompanied by impaired sensitivity of the skin;
- in the affected area, motor activity is significantly reduced.
Why is it developing?
There are several factors that may cause the disease:
- hypertension;
- kidney disease;
- coronary heart disease (angina pectoris);
- viruses or infections that affect the heart;
- drug or alcohol abuse;
- genetic factors, since the symptom sometimes occurs in newborns or fetal children;
- development of a heart valve with abnormalities;
- consequences of pregnancy and childbirth.
Article on the topic
Don't give in to pressure. How to protect yourself from hypertension
Therefore, those who are at risk for such triggers should undergo regular examinations with a cardiologist to identify the problem in a timely manner. Any disease detected as early as possible is easier to correct.
When to see a doctor
A routine examination by a cardiologist should occur annually. If pain is present, but it is mild, occurs occasionally, does not affect activity, and is not accompanied by additional symptoms of heart disease (high blood pressure, arrhythmia, or shortness of breath), under no circumstances should you cancel your scheduled visit. At your appointment, do not refuse additional tests - Holter monitoring, ECG, ultrasound of the heart, blood tests. This will help the doctor assess your condition and prescribe more accurate treatment.
You should immediately contact a cardiologist if you have the following symptoms:
- irradiation and localization of pain is characteristic of a heart attack;
- active increase in pain;
- unpleasant sensations persist for more than half an hour;
- the pain becomes unbearable, stabbing in nature;
- occurs again after a short period of time;
- Fainting and surges in blood pressure occur.
Diaphragm
Directly below the heart is a large, dense, elastic septum called the diaphragm.
The diaphragm is the membrane that separates the chest cavity from the abdominal cavity. It has the appearance of a dome, which faces its convexity towards the chest. The diaphragm consists of muscle tissue and dense fibrous tissue.
The diaphragm not only separates the two largest cavities of the human body, it also takes an active part in breathing. The edges of the diaphragm are tightly fixed to the inside of the chest, and its dome-shaped top moves freely up and down.
When the dome of the diaphragm moves down, the chest and lungs expand, and inhalation occurs. When the diaphragm rises, the chest, and with it the lungs, decrease in size. Exhalation occurs. It’s not for nothing that the diaphragm is also called the respiratory muscle: its role in the act of breathing is very significant.
The heart rests on the diaphragm. One of the surfaces of the heart (lower) is called the diaphragm.
So the diaphragm is below the heart, but below the diaphragm, there are several organs below the heart.
Preventive actions
As with any other disease, it is better to try to prevent it than to treat it later. And here the issue of preventing “bull’s heart” is important.
When an enlarged heart occurs, the consequences can manifest themselves in different ways, so with the least risks you should pay attention to your health. Ideally, you should adhere to the principles of a healthy lifestyle and eliminate bad habits such as alcohol and smoking. A person who does not want to face the consequences of an enlarged heart should constantly monitor blood pressure, consume less salt, engage in suitable physical activity, and lose excess weight. The recommendations are simple, but they will help you keep yourself in good shape.
Pathology therapy
Naturally, many are concerned about the treatment of this problem. And it must also be comprehensive.
First of all, it is necessary to determine the cause of cardiomegaly, that is, to establish the underlying disease. If a person has this pathology, basic therapy is carried out. For example, coronary heart disease or hypertension is corrected.
At the first stage, drug therapy is used to treat cardiomegaly. It includes the prescription of diuretics to remove excess fluid from the body, antithrombotic drugs to reduce the risk of developing a blood clot, and beta blockers to slow the rhythm and reduce the load on the heart.
Article on the topic
No interruptions! How are cardiac arrhythmias treated?
In some cases, surgical interventions are used to restore the damaged valve and improve the performance of blood vessels.
A special pump is also implanted to help the heart work. In some cases, devices are used to regulate the heartbeat: with an enlarged heart, a pacemaker is used to coordinate the contractions of the heart muscle.