The heart is a muscular pump that ensures continuous movement of blood through the vessels. Together, the heart and blood vessels make up the cardiovascular system. This system consists of the systemic and pulmonary circulation. From the left side of the heart, blood first moves through the aorta, then through large and small arteries, arterioles, and capillaries. In the capillaries, oxygen and other substances necessary for the body enter the organs and tissues, and from there carbon dioxide, metabolic products, are removed. After this, the blood turns from arterial to venous and again begins to move towards the heart. First along the venules, then through smaller and larger veins. Through the inferior and superior vena cava, blood again enters the heart, only this time into the right atrium. A large circle of blood circulation is formed.
Venous blood from the right side of the heart is sent through the pulmonary arteries to the lungs, where it is enriched with oxygen, and returns to the heart again - this is the pulmonary circulation.
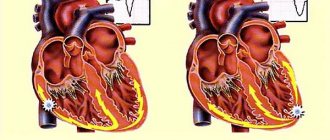
Inside, the heart is divided by partitions into four chambers. The two atria are divided by the interatrial septum into the left and right atria. The left and right ventricles of the heart are separated by the interventricular septum. Normally, the left and right parts of the heart are completely separate. The atria and ventricles have different functions. The atria store blood that flows into the heart. When the volume of this blood is sufficient, it is pushed into the ventricles. And the ventricles push blood into the arteries, through which it moves throughout the body. The ventricles have to do more hard work, so the muscle layer in the ventricles is much thicker than in the atria. The atria and ventricles on each side of the heart are connected by the atrioventricular orifice. Blood moves through the heart in only one direction. In the systemic circle of blood circulation from the left side of the heart (left atrium and left ventricle) to the right, and in the small circle from the right to the left.
The correct direction of blood flow is ensured by the valve apparatus of the heart:
Valves:
- tricuspid
- pulmonary
- mitral
- aortic
They open at the right time and close, preventing blood flow in the opposite direction.
The role of the heart in the body
The heart has a very important task - ensuring blood circulation. Why is this so important? The thing is that every organ in the body, to one degree or another, needs a constant supply of oxygen and nutrients. In addition, “waste” material in the form of carbon dioxide and various metabolites must be removed from the organs. Both provide blood, the movement of which is associated with the work of the heart. Contracting with a certain force and frequency, it maintains constant blood circulation through the vessels. Thus, cardiac arrest or disruption of its functioning leads to oxygen starvation of the entire body.
Is the heart an ordinary muscle?
The myocardium, the main functional component of the heart wall, does consist of muscle fibers, but their structure is significantly different from skeletal muscles. Structurally and biochemically, the myocardium is designed in such a way that fatigue practically does not occur. The heart “rests” only in the periods between contractions. This mode of operation requires a constant supply of oxygen to the myocardium. This explains the fact that if the blood supply to the myocardium is disrupted, a heart attack develops relatively quickly, that is, cell death due to lack of oxygen. Skeletal muscles can remain viable for a long time in the absence of oxygen.
What happens if the heart stops beating?
For clarity, it is enough to imagine a situation where the heart no longer performs its function. In this case, the brain will be the first to be affected. In humans, this organ has reached its highest development and requires an appropriate amount of resources for its work. Therefore, as soon as the blood supply stops, the person almost instantly loses consciousness, which is a sign of a severe violation of brain function. Next, the death of neurons occurs. This process begins from the first minute after cardiac arrest, steadily progressing. After 3 minutes, irreversible changes in brain tissue become possible. Even after successful resuscitation measures, the patient will most likely remain disabled. After 5 minutes, in most cases, the death of the cerebral cortex occurs, which results in the death of the patient. Successful resuscitation at this stage can save life. But can a person’s state in which he is unable to speak, move, breathe or think be called “life”? A longer cessation of blood circulation inevitably leads to death.
Of course, the given time frames are arbitrary. A younger and healthier person will last longer, an older and sick person - less. But one thing is clear: stopping the work of any other organ can hardly cause such a sudden death.
Figure 1. What's good for heart health. Image: MedPortal
Features of muscle tissue are:
- striated striations formed by myofibrils of cardiomyocyte cells;
- the presence of two types of fibers: thin (actin) and thick (myosin), connected by cross bridges;
- the connection of myofibrils into bundles of different lengths and directions, which makes it possible to distinguish three layers (superficial, internal and middle).
The structure of the heart muscle is different from skeletal and smooth muscle muscles, which provide movement and protection of internal organs
The morphological features of the structure provide a complex mechanism of heart contraction.
Where is the heart
The heart is located in the chest cavity directly behind the sternum. Most of it is to the left in relation to the sternum, in the middle and to the right of it is the smaller part. However, it is extremely rare that the heart may, on the contrary, be located more to the right of the sternum. This anatomical feature is called dextrocardia.
The heart is enveloped by the lungs on both sides, in the front it touches the chest in a small area, and in the back there are the spine, blood vessels, nerves, digestive and respiratory tracts. Thus, the heart is, as it were, “walled up” with organs and bone formations on all sides. The space between the lungs, sternum and spine, where the heart is located, is called the mediastinum.
How to distinguish heart pain from others?
Pain due to intercostal neuralgia, pathology of the respiratory system and musculoskeletal system is very similar to pain in the heart. If you do not know some of the features of this type of pain, you can easily mistake the existing sensations for cardiac pathology. Heart problems are unlikely if:
- You can easily indicate the pain point, that is, the source of pain is small.
- Pain occurs when turning the body, sudden movements.
- Taking a full breath increases the intensity of pain.
- Feeling the painful area on the chest increases the pain.
- Taking analgesics such as Nurofen reduces pain.
Despite these seemingly clear differences in pain syndromes, pain due to cardiac pathology can sometimes be atypical. In this case, even a doctor cannot always make a correct diagnosis based only on the characteristics of the pain. For example, there are cases when a patient goes to the dentist about pain in the lower jaw, without even suspecting that in this case it is a symptom of angina pectoris. Other variants of atypical symptoms are also known. Therefore, all newly detected pain in the heart area is a reason to consult a doctor.
A doctor can determine some diseases simply by listening to the heartbeat. Photo: branin / freepik.com
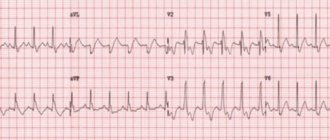
Supraventricular tachyarrhythmias
Rhythm disorders involving the atria are called supraventricular (supraventricular) arrhythmias. This group of rhythm disturbances is the most common, and it is the one that doctors and patients have to deal with most often. There are 5 main types of supraventricular arrhythmias:
• atrioventricular nodal tachycardia;
• Wolff-Parkinson-White syndrome;
• intraatrial tachycardia;
• atrial flutter;
• atrial fibrillation.
Structure and functions of the parts of the heart
The heart is a cone-shaped muscular organ, the apex of which faces downwards. The upper part of the organ, from which the large vessels emerge, is called the base of the heart.
The heart consists of four chambers: two atria, located above, at the base, and two ventricles, located below, forming the apex. To better imagine the structure of the organ and the function of each of its sections, it is convenient to divide the heart into 2 halves, right and left, and consider them separately.
Right side of the heart
On the right, the heart is represented by the right atrium and the right ventricle. The atrium is significantly smaller than the ventricle in size. These formations are delimited from each other by the tricuspid valve.
Mainly the right half of the heart (right heart) is characterized by its connection with the lungs. The right heart transports venous blood from the organs to the lungs, where gas exchange occurs, as a result of which the blood becomes arterial. This happens as follows. Venous blood from all organs and systems of the body flows through the superior and inferior vena cava into the right atrium. Having collected a sufficient volume of blood, the atrium contracts and blood flows into the right ventricle. As soon as the blood pressure in the ventricle reaches the required value, the tricuspid valve leaflets collapse and the walls of the ventricle contract. Venous blood flows from the ventricle into the pulmonary trunk, which divides into two pulmonary arteries and carries blood further to the lungs.
Figure 2. Right half of the heart. Red arrows indicate the course of venous blood. The lungs are shown schematically at the top. Illustration by Danila Melnikov
As can be seen in Figure 1, there is also a valve at the exit of the right ventricle called the pulmonary valve. Both valves are designed to prevent blood from returning to previous parts of the heart during the next contraction of the myocardium.
Left half of the heart
The left half of the heart (left heart) is responsible for transporting arterial blood enriched with oxygen in the lungs to all organs and systems. The left heart is more developed than the right, since in order to move blood into every capillary of the human body, it is necessary to create high blood pressure. Also, unlike the right side, between the left atrium and the left ventricle there is a bicuspid (mitral) valve. Otherwise, the structure of the left parts of the heart is similar to the structure of the right (see Figure 3).
Figure 3. Left half of the heart. Red arrows indicate arterial blood flow. The lungs are shown schematically at the top. Blue vessels are pulmonary veins. Illustration by Danila Melnikov
When describing the direction of blood flow, we focused on the lungs. What happens next? After gas exchange occurs, blood flows through the pulmonary veins into the left atrium. The atrium then contracts, the mitral valve opens, and the left ventricle fills with blood. Having collected the required volume of blood, the ventricle contracts, the aortic valve, located at the base of the aorta, opens, and blood enters the aorta. The aorta, in turn, giving off numerous branches, supplies blood to all organs and systems.
Circulation circles
Having collected the two halves of the heart together, we will see the following picture (see Figure 4). Two circles of blood circulation are formed. The first, small circle, begins in the right ventricle and ends in the left atrium. It is necessary for oxygenation of blood in the lungs. The second, large circle, begins in the left ventricle and ends in the right atrium. Its purpose is to distribute oxygenated blood to the organs, and take venous blood from them to the heart in order to circulate it again in a small circle.
Figure 4. Circulation circles. Designations: R/R - right atrium; R/F - right ventricle; L/R - left atrium; L/F - left ventricle. The liver at the bottom of the picture is an example of a blood-supplying organ. Illustration by Danila Melnikov
As you can see, the heart is inextricably linked by blood circulation circles with all human organs, but first of all with the lungs, because there is a separate circle for them. That is why, with heart pathology, the lungs often suffer.
Cardiac cycle
Adequate blood supply to the body is ensured by the coordinated contraction of the muscle fibers of the heart wall, which determine the organ’s work cycle.
There are two main phases:
- systole – contraction;
- diastole – relaxation.
The different speeds of impulse conduction through atypical cardiomyocytes with the presence of a delay in the atrioventricular node ensure the coordinated functioning of the organ: during atrial systole, blood penetrates into the ventricles. The latter are in the relaxation phase, which forms a sufficient volume to be filled with liquid (up to 100 ml on the left).
During contraction of the ventricles, the valves of the aorta and pulmonary artery open, the valves of the atrioventricular connections are closed - blood flows into the circulation. The pulse is determined in the peripheral vessels, and the heartbeat is determined in the chest area.
At this time, the atria are in the diastole phase and are filled with blood from the hollow (right sections) and pulmonary veins (left).
There is a statement that the heart works half its life and rests half of its life, since the duration of systole and diastole is the same (0.4 seconds each).
How does a person's heart beat?
Like any muscle, the heart is innervated by peripheral nerves, which allows you to regulate the strength and frequency of its contractions. However, the following fact is known. If you denervate the heart, that is, cut the nerves going to it, it will not stop beating. If you do the same with any other muscle, it will no longer be able to contract. Why is this happening?
The thing is that the heart has its own analogue of the nervous system, which is called the cardiac conduction system. It is represented by two nodes and several branches of cells that are somewhat different from ordinary myocardial cells. They are able to continuously generate electrical impulses at a specific frequency that trigger muscle contraction. When doctors install a pacemaker in a patient, they are thereby trying to restore the disrupted functioning of our “congenital pacemaker” - the conduction system of the heart.
But the peripheral innervation, which we “got rid of” in the experiment above, also has an important function. When we are lying down in a calm environment, it is hardly possible to feel our own pulse - we do not feel the heartbeat. But after a short run, you can feel your heartbeat literally throughout your entire body. This phenomenon can be explained by the fact that during physical activity the tone of the sympathetic nerves going to the heart increases. As a result, the strength and frequency of heart contractions increases to meet the increased oxygen demand of working muscles. In a quiet stop or during sleep, the work of parasympathetic innervation prevails, and everything happens the other way around.
Why does the heart beat?
By placing your ear to a person's chest, you can hear a characteristic rhythmic knocking sound.
Normally, it consists of two tones: the first - strong, ringing and the second - quieter. Tones are created by valves when their valves close. When a doctor listens to a patient's heart with a phonendoscope, he can evaluate these sounds and give a preliminary conclusion on the operation of the valve apparatus. Since the sounds of the valves correspond to the next heart contractions, they can be used to characterize the heart rhythm. Various pathological phenomena can change the rhythm, make it irregular, frequent, rare, dull, etc. These characteristics allow the doctor to diagnose some heart diseases by barely hearing the heartbeat.
How does your heart hurt?
Heart pain is most often caused by coronary heart disease (CHD). In this condition, blood circulation in the heart itself is disrupted, and pain occurs due to lack of oxygen. This pain has its own characteristics:
- Localized behind the sternum.
- It is impossible to pinpoint the pain point.
- Accompanied by a feeling of pressure and burning behind the sternum.
- May spread to the left shoulder and upper arm, left arm, lower jaw.
- Often appears due to stress or physical activity.
- The intensity varies: from a feeling of discomfort to unbearable pain.
- With angina, the pain lasts up to 10 minutes.
- With myocardial infarction, it can last for hours, accompanied by suffocation and a feeling of lightheadedness.
There are also pains not associated with coronary artery disease, they are called cardialgia. They may indicate completely different diseases and are not always associated with pathology in the heart. Cardialgia varies in nature, but is rarely pressing and burning, as with ischemic heart disease. Their intensity is also lower.
Important!
If you detect any pain in the heart area, you should contact a cardiologist. If the pain is intense and lasts longer than 10 minutes, this is a reason to call an ambulance. Ignoring heart pain can be life-threatening.
Other symptoms of heart disease
Heart disease makes itself felt not only by pain, but also by other symptoms:
- Shortness of breath occurs not only when the respiratory system is damaged, but also the heart. This is an unfavorable symptom that indicates the neglect of the pathological process. It can be caused by valve defects, arrhythmias, cardiomyopathies and a number of other diseases. Shortness of breath may also indicate chronic heart failure, which can be the outcome of other heart diseases (myocardial infarction, hypertension, myocarditis, etc.)
- The feeling of interruptions in the work of the heart occurs most often with various arrhythmias. It may seem as if the heart is periodically tumbling in the chest, and sometimes there is a feeling that the heart is beating irregularly. The culmination of such symptoms is loss of consciousness due to arrhythmia.
- A rare pulse often indicates a disruption in the conduction system of the heart. Normally, the heart contracts at a rate of 60-89 beats per minute. If, after feeling the pulse on the wrist, it is found that this value is below 55 beats, the presence of the disease is quite likely. The exception is professional athletes, whose rare pulse is normal.
During physical activity, the strength and frequency of heart contractions increases, and we feel our own pulse well. Photo: axesor/Depositphotos
How to eat to keep your heart healthy?
A healthy diet allows you to achieve prevention against two of the most common cardiovascular pathologies: hypertension and coronary heart disease. The most effective measures are the following³:
- Reduce your intake of saturated fatty acids. They are found in large quantities in many cheap confectionery products. It is better to choose products that do not contain palm, palm kernel and coconut oil.
- Olive oil, nuts, fatty fish, and seafood are preferred sources of fat. These foods contain mono- and polyunsaturated fatty acids, the consumption of which reduces the risk of cardiovascular disease (CVD).
- Minimize foods fried in oil in your diet, especially fast food. The trans fats contained in the latter increase the risk of CVD diseases.
- It is not recommended to regularly consume sugar-containing drinks such as lemonade, soda and juice. They do not satisfy thirst, which leads to uncontrolled consumption. Simple sugars in such drinks increase the risk of both diabetes and coronary heart disease.
- Increase the amount of dietary fiber in your diet. Grains, fruits and vegetables will help with this.
- Reduce table salt consumption. Recommended figures are up to 5 g/day, but according to new standards, the maximum reduction in CVD risk is achieved by consuming 3 grams of salt per day. This aspect of diet plays a large role in the context of hypertension.
- Foods high in potassium are beneficial. This element is found in large quantities in fresh fruits and greens and helps lower blood pressure. It is recommended to eat 400-600 g of vegetables, fruits and berries daily.
Tachyarrhythmia
This is an abnormally fast heart rate (usually 100 to 400 beats per minute, which occurs either in the upper chambers of the heart (atrial fibrillation, supraventricular tachycardia) or in the lower chambers (ventricular fibrillation, ventricular tachycardia)).
Causes of tachyarrhythmia:
• Heart diseases such as high blood pressure, coronary artery disease (atherosclerosis), heart valve disease, heart failure, cardiomyopathy, tumors and infections.
• Other medical conditions, such as thyroid disease, some lung diseases, electrolyte imbalances, and alcohol and drug abuse.
• Caused by abnormal accessory pathways or extrasystoles.
Tachyarrhythmias occur when the impulse contracting the heart muscle arrives earlier than normal heart rhythm would suggest. Tachyarrhythmias can begin in the upper or lower chambers of the heart.
Tachyarrhythmia includes various types of cardiac arrhythmias:
• Supraventricular tachycardia.
• Ventricular tachycardia (VT).
• Ventricular fibrillation (VF).
Preventing proper heart function
When it comes to preventing cardiovascular diseases, physical activity is the first thing to think about. Research figures unanimously confirm this.
Regular physical activity, compared with a sedentary lifestyle, is associated with a 22–36%² reduction in all-cause mortality and a 25–35%² reduction in cardiovascular mortality.
In people already diagnosed with coronary heart disease, exercise training reduced the risk of overall mortality by 19–58%² and cardiovascular mortality by 20–62%². Even 1 hour of walking per week already reduces the above risks². What if you walk for an hour every day? A correlation was also found with walking speed: the faster the step, the higher the result of prevention. Thus, in order to significantly reduce the risk of heart disease, it is enough to spend half an hour to an hour of intense walking every day.
Physical activity is a good preventive measure for heart disease. The faster the step, the better the result. Photo: Kzenon/Depositphotos
Is the heart really that vulnerable?
In fact, the heart has a large number of adaptive reactions. They can maintain its normal activity for a long time even in the face of a large number of negative factors such as poor diet, inactive lifestyle and obesity. Under conditions of increased load, the myocardium increases in size and compensates for it. If the conduction system is disrupted, the heart does not stop contracting—second-order pacemakers come into play and continue to send impulses, albeit at a lower frequency. With valve defects, due to disturbances in hemodynamic parameters, the heart contracts more strongly and also increases in size. There are many such examples.
The problem is that these adaptive responses only help for a while. Over the course of several years, they turn against the heart and irreversible damage begins. Moreover, the symptoms, unfortunately, appear just at a time when it is already too late - the changes that have arisen are irreversible, and the disease becomes chronic.
Sources
- Prives M. G., Lysenkov N. K., Bushkovich V. I. / Human Anatomy. — 12th ed., revised. and additional - St. Petersburg: Publishing house SPbMAPO, 2006. - 720 p., ill.
- Krivoshapova Kristina Evgenievna, Tsygankova Daria Pavlovna, Barbarash Olga Leonidovna Low physical activity as a risk factor for cardiovascular morbidity and mortality // Systemic hypertension. 2021. No. 3.
- Smetneva Natalya Sergeevna, Pogozheva Alla Vladimirovna, Vasiliev Yuri Leonidovich, Dydykin Sergey Sergeevich, Dydykina Irina Stepanovna, Kovalenko Alexey Anatolyevich The role of optimal nutrition in the prevention of cardiovascular diseases // Nutrition Issues. 2020. No. 3.
- Yakushin S.S., Filippov E.V. Physical activity and its importance for the prevention of cardiovascular diseases // Clinician. 2015. No. 3.