Indicator norm
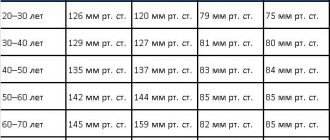
Pulse pressure is the difference between systolic and diastolic blood pressure, which is normally between 40 and 60 mmHg. The meaning is strictly individual, has gender and age differences, presented in the table.
| Age | PBP norms for women in mm Hg. Art. | PBP norms for men in mmHg. Art. |
| From 20 to 25 | 43 | 47 |
| From 25 to 30 | 44 | 51 |
| From 30 to 40 | 46 | 48 |
| From 40 to 60 | 52 | 51 |
| From 60 to 65 | 51 | 50 |
| Over 65 | 47 | 46 |
These are data from the EAC (European Association of Cardiology) based on the results of fifteen years of observation of several groups of patients. If deviations from the norm exceed 10 units, you should look for the cause of the pathological process developing in the body.
conclusions
Pulse blood pressure is considered an important indicator of the condition of the heart and blood vessels; it is normally about 30-50 Hg, but can vary depending on gender, age and weight. This indicator reflects such essential characteristics as the ratio of pumping function and peripheral resistance of large arteries.
Both an increase and a decrease indicate the presence of pathology, even with normal diastolic or systolic pressure numbers. If such deviations are detected, you should immediately contact a specialist to conduct additional examination and establish an accurate diagnosis.
Reasons for low PD
Low pulse pressure is said to occur when the difference between systolic and diastolic readings falls below 40 mmHg, which indicates serious problems with the heart (a drop of 25% from normal SBP threatens disaster).
There are no physiological reasons for this condition. Hypothermia, stress, and physical activity cause slight fluctuations. Serious deviations from the norm have exclusively pathological causes. The main ones:
a – post-infarction large-focal cardiosclerosis; b – focal cardiosclerosis.
- bleeding, most often internal, causing hypovolemia: a drop in blood pressure reduces the pulse difference, as the body strives to compensate for discomfort and normalize tissue nutrition, but at the same time, the lack of nutrients significantly impairs the potential of internal organs;
- myocardial infarction, namely the left ventricle (acute disturbance of blood flow with the development of muscle necrosis) - leads to a sharp drop in PP to critical figures;
- cardiogenic shock - a consequence of a rapid drop in blood pressure due to aortic stenosis, AMI - can be fatal in a short time;
- decompensated heart failure creates a risk of spontaneous development of one of the fatal complications;
- inflammation of the heart muscle of various etiologies from myocarditis to pancarditis;
- hyperreninemia against the background of dysfunction of the hypothalamic-pituitary system, adrenal glands causes renal ischemia as a consequence of vascular spasm, a biochemical imbalance develops, causing a drop in pulse pressure, due to pathological regulation of vascular tone, impaired glomerular filtration, internal blood flow of the organ (prospective - chronic renal failure);
- atrophy of brain neurons with the development of encephalopathy, impaired control of vascular tone, and the formation of hypothalamic syndrome;
- vitamin deficiency, leading to profound changes in the nutrition of tissues and organs;
- various cardiovascular syndromes, for example, Morgagni-Adams-Stokes: a sharp decrease in cardiac blood output with the development of cerebral ischemia.
Understanding the causes of pathological fluctuations is necessary to prevent lethal complications.
Why is it dangerous
What is pulse pressure is clear, but what does it entail? Any “sway” from the norm threatens our health to one degree or another. An organism working as an integral system can patch up even the most serious gaps without causing damage to other organs. But when it comes to vital organs, pathologies cannot go unnoticed.
Patients with abnormal pulse pressure often experience:
- Myogenic dilatation of the heart;
- Stenosis of the aortic ostia - which is fraught with a decrease in the blood volume ejected by the heart;
- Renal ischemia;
- Narrowing of the vascular bed, slowing down the circulation of biological fluid.
But the formation of these ailments is not the fastest process, so if you seek help in a timely manner, diagnoses can be avoided.
Reasons for high PP
Pulse pressure above 60 mmHg is considered to be high; it is caused by a number of reasons associated with disruption of the heart and blood vessels:
Stages of atherosclerosis: prelipid, lipoid, liposclerosis, atheromatosis, calcification
- hyperthermia, accompanied by hypertension with fluctuations in the upper and lower values;
- infections or autoimmune damage to the heart muscle;
- Alzheimer's disease;
- congenital or acquired heart defects, especially aortic valves;
- arterial hypertension of various etiologies, existing for a long time with a predominant increase in systolic pressure;
- decompensated renal failure;
- congestive heart failure, coronary heart disease;
- hyperfunction of the thyroid gland;
- atherosclerosis, which provokes narrowing of the lumen of blood vessels with atherosclerotic plaques;
- lack of vitamins;
- anemia;
- any pathology associated with disorders of the blood coagulation system, changes in its rheological properties;
- total vasospasm of various nature.
Other reasons are possible, including the formation of aneurysms of large vessels, changes in their course due to various pathological transformations.
Symptoms of falling or increasing PP
Clinically, a drop in the difference between SBP and DBP is characteristic of hypotension, but a possible variant that occurs with a stable level of systolic and high diastolic pressure is isolated diastolic hypertension. High pulse pressure is formed against the background of long-standing hypertension and is associated mainly with fluctuations in the systolic rate. Symptoms of pathological fluctuations in men and women are presented in tables.
| Symptoms of falling PD | Symptoms of increased PD |
| Throbbing headache, often in the temporal region - a nonspecific symptom, reminiscent of migraine | Headache, usually in the back of the head |
| Lightheadedness, dizziness, loss of orientation in space | Nausea, vomiting caused by insufficient nutrition of the brain due to vascular spasm |
| Sweating, hypothermia due to disruption of the thermoregulation center | Hyperthermia, redness of the cheeks, hot flashes, redness of the facial skin - failure of the preoptic nucleus of the hypothalamus |
| Encephalopathy with ataxia (unsteady gait), orthostatic disorder | Vascular psychoses requiring correction in a special psychoneurological hospital |
| Cyanosis of the nasolabial triangle, shortness of breath | Speech disorders, slow movements |
| Loss of sensation in limbs | Paralysis, paresis |
| Drowsiness, apathy | Nervousness, tearfulness |
| Meteosensitivity | Meteor dependence |
| Bradycardia | Tachycardia |
This symptomatology may be accompanied by other nonspecific symptoms associated with vascular spasm or intoxication, but the main marker of the problem remains pulse pressure indicators.
Possible consequences and complications
Dissonance between pulse and blood pressure is dangerous for the functional state of the body, since with a rapid heartbeat, hypoxia of tissues and organs occurs, which entails the development of irreversible changes in them.
With a simultaneous increase in diagnostic indicators, the following very dangerous conditions may occur:
- disorder of the digestive tract;
- ischemic brain damage;
- necrosis of the cardiomyocyte area;
- arrhythmic shock.
A prolonged and constant increase in heart rate can significantly reduce the performance of a hypertensive patient. The patient experiences a feeling of irritability and complains of causeless weakness and malaise.
Under conditions of excessive load, the myocardium requires more oxygen, which leads to its increased waste. In vessels of small diameter, a deficiency of nutrients occurs, provoking the formation of cardiomyopathy.
Danger of pathology
Fluctuations in pulse pressure are dangerous for the development of fatal complications in men and women, such as:
- acute heart failure resulting in stroke or heart attack;
- chronic heart failure with symptoms of stagnation in the systemic and pulmonary circulation, dystrophy of internal organs;
- myocardial ischemia;
- pre-fainting, traumatic fainting;
- acute and chronic kidney failure;
- dementia, vascular psychoses, Alzheimer's disease;
- visual impairment.
To prevent such conditions, timely diagnosis and preventive treatment are needed.
What will make the current situation worse?
The heart and blood vessels create a system that is very sensitive to the lifestyle that you lead. Not a single bad habit will go unnoticed by her. A variety of factors provoke pressure surges. But it’s one thing when they occur rarely, one-time, but it’s quite another thing if they make up your way of life.
These factors can be divided into:
- External. These include obesity (a provocateur of many somatic diseases), physical inactivity, iron deficiency anemia, chronic stress, fasting and exhausting diets, overwork, increased anxiety, and sudden weight loss. These also include bad habits - smoking and drinking, overeating, destabilization of sleep patterns.
- Internal. This list includes diabetes mellitus, cardiosclerosis, heart block, dermatitis, adrenal burnout, endocrine abnormalities, liver cirrhosis, serious allergic reactions, etc.
People with the above ailments should not only be attentive to their health: they need to understand that their illness makes adjustments to their lifestyle. And you shouldn’t resist this; you need to calmly change your routine, habits, and sacrifice something for the sake of maintaining your health. And the goal of all this is to improve the quality of life, and not self-destruction, as is often the case.
First aid
It is impossible to stop a large or small pulse difference on your own; an ambulance is needed. Before her arrival:
| With high blood pressure | At low pressure |
| Do not take any medications unless previously approved by your doctor | |
| Do not drink or eat anything (fainting, vomiting, aspiration of vomit), you can take sedative drops: Corvalol, Valocordin, Valerian | Eat something salty, drink a couple of glasses of water, a cup of coffee, green tea |
| Take a comfortable position, open the windows for oxygen flow, loosen tight clothes | |
| Carry out tonometry, record the results for the doctor | Tonometry every 10 minutes with accurate recording |
The doctor may suggest hospitalization, the patient has the right to refuse, but it is more reasonable to stop the attack inpatiently, under the supervision of specialists.
How to help yourself at home?
What to do if your heart rate suddenly increases or decreases? First aid measures are not specific. You can't do anything on your own. Qualified medical assistance is required.
It is advisable to call an ambulance, and until the doctors arrive, follow the following rules:
- Do not take any pills under any circumstances, on the advice of your brother, matchmaker, neighbor, etc. All people are different, there are many reasons for the development of a pathological condition. There is a risk of making things worse. A diagnosis is needed, only after that can some measures be taken to normalize the condition.
- Don't drink or eat. Fainting and vomiting are possible. It costs nothing to choke on vomit.
- You need to take a half-sitting position and calm down. Breathe evenly, do not hold your breath.
- Ensure a flow of fresh air into the room, remove constrictive jewelry and tight clothing items (loosen the collar, remove the tie).
Upon arrival, doctors tell you about your condition and follow the recommendations. Hospitalization may be required, but you should not refuse.
Diagnostics
The diagnostic algorithm for men and women is standard; after collecting an anamnesis, physical examination, and consultation with specialized specialists (if necessary), the following is carried out:
- tonometry with calculation of pulse difference;
- UAC, OAM, biochemistry;
- 24-hour blood pressure monitoring;
- ECG, EchoCG, cardio-ultrasound;
- Dopplerography of the vessels of the neck, head;
- blood testing for hormones;
- Ultrasound of the kidneys.
Additionally, any laboratory or instrumental examination may be prescribed to determine the cause of pathological fluctuations.
Diagnostic measures
To diagnose a pulse pressure disorder and the cause of its occurrence, you need to consult a therapist. The therapist will conduct a general examination and write a referral to a cardiologist, endocrinologist, neurologist, nephrologist. A comprehensive examination will help to accurately determine the cause of the deviation of pulse pressure from normal values. After a comprehensive examination, the doctor will prescribe appropriate treatment according to indications.
Diagnostic methods:
- neuromonitoring, checking the functioning of the kidneys and thyroid gland;
- physical diagnosis;
- collecting information about the development of the disease, concomitant diseases, and other abnormalities;
- measuring blood pressure using a tonometer;
- continuous recording of heart dynamics on ECG throughout the day;
- ECG;
- Ultrasound of the heart;
- Doppler examination of the vessels of the neck and head;
- analysis of thyroid hormones;
- Ultrasound of the kidneys;
- clinical urine analysis;
- general blood analysis;
- blood chemistry.
The types of diagnostic tests are determined by the attending physician after assessing the general condition of the patient.
ECG is one of the most accessible diagnostic methods
Features of treatment
Deviations of normal blood pressure in any direction require identification of the root cause of the pathology and its elimination (relief). Without this, treatment is either useless or dangerous, since what helps with one disease can cause death in another.
Minor fluctuations in blood pressure do not require any intervention. They are most often one-time and physiological: temperature changes, climate zone changes, physical or psychological overload. The maximum that needs to be done is to consult a cardiologist in case of recurring abnormalities.
The doctor can prescribe folic acid - vitamin B9, which will support the heart and eliminate overload. The vitamin is produced by intestinal microflora and is responsible for cell growth and DNA preservation. During hyperloads, it is not enough, therefore, to stabilize the immune system, metabolic processes, and vascular elasticity, additional supply from the outside is necessary.
Patients with extra pounds and high pulse pressure are prescribed diuretics to normalize the total volume of circulating blood: from Furosemide, Diacarb, Hypothiazide to Triampur, Veroshpiron, Spironolactone. The treatment regimen is strictly individual, depending on the degree of obesity, blood pressure levels, and concomitant pathology.
In the presence of atherosclerosis, statins are added that normalize cholesterol metabolism: Atorvastatin, Rosuvastatin, Pitavastatin. They use nicotinic acid (niacin, vitamin PP, vitamin B) - a lipid-lowering agent, ion exchange resins (hemodialysis) or bile acid sequestrants: Cholestyramine, Colestipol, which reduce low-density lipoproteins that can destroy the arterial wall.
Age-related myocardial degeneration is stopped by prescribing cardiac glycosides: Digoxin, Celanide, Strophanthin. To reduce the diastolic index, Papaverine, calcium inhibitors: Amlodipine, Norvasc, Lacidipine, antispasmodics: Platiphylline, Scopolamine, Spazgan are prescribed.
To maintain vital functions, adrenergic drugs are used: Isadrin, Dobutamine, Dopamine. They act quickly, but only for a short time. For acute heart failure - intravenously - Amrinon and Milrinone.
Hormone replacement therapy can be used, and in extreme cases, surgical intervention: heart disease, aneurysms, total vascular atherosclerosis.