Frequent ventricular extrasystoles - what is it?
Ventricular extrasystole is an arrhythmia, or disturbance in the heart rhythm.
The disease is associated with the appearance of extraordinary impulses. These areas are called ectopic foci and are found in the wall of the lower parts of the heart (ventricles). Such impulses contribute to the occurrence of extraordinary, partial contractions of the heart. The prognosis of the course of the disease depends on whether the patient has anatomical pathologies of the heart; electrophysiological parameters of extrasystole (frequency of occurrence, degree of premature manifestation, location); the ability of ventricular extrasystole to negatively affect the performance of the heart muscle and the body as a whole.
https://www.youtube.com/watch?v=ED_otx3i2Uc
Used for prognostic assessment of ventricular extrasystoles in intensive care units in patients with coronary artery disease.
0 – no ventricular extrasystoles;
1 – 30 or less ventricular extrasystoles per hour;
2 – {amp}gt; 30 ventricular extrasystoles per hour;
3 – polymorphic (polytopic) ventricular extrasystoles;
4A – paired extrasystoles;
4B – 3 in a row and {amp}gt; ventricular extrasystoles (short episodes of paroxysms of ventricular tachycardia);
5 – ventricular extrasystoles of the “RnaT” type;
Grades 3–5 are considered threatening extrasystoles, since the likelihood of ventricular fibrillation and ventricular tachycardia is high.
Classification of supraventricular arrhythmias
Some atrial tachycardias associated with acute medical conditions.
Some multifocal atrial tachycardias.
The creation of the Lown classification of ventricular extrasystole is an important step in the history of arrhythmology. Using the classification in clinical practice, the doctor can adequately assess the severity of the disease in each patient. The fact is that PVC is a common pathology and occurs in more than 50% of people. In some of them, the disease has a benign course and does not threaten their health, but others suffer from a malignant form, and this requires treatment and constant monitoring of the patient. The main function of ventricular extrasystole, Lown classification, is to distinguish malignant from benign pathology.
1. Monomorphic ventricular extrasystole with a frequency of less than 30 per hour.
2. Monomorphic PVC with a frequency of more than 30 per hour.
3. Polytopic ventricular extrasystole.
4. The fourth class is divided into two subclasses:
- Paired VES.
- 3 or more VES in a row – ventricular tachycardia.
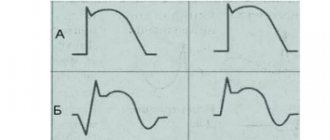
5. VES type R on T. ES is assigned the fifth class when the R wave falls on the first 4/5 of the T wave.
Lown's classification of PVCs has been used by cardiologists, cardiac surgeons and doctors of other specialties for many years. Appeared in 1971 thanks to the work of B. Lown and M. Wolf, the classification, as it seemed then, would become a reliable support for doctors in the diagnosis and treatment of PVCs. And so it happened: until now, several decades later, doctors focus primarily on this classification and its modified version from M. Ryan. Since that time, researchers have not been able to create a more practical and informative gradation of VES.
However, attempts to introduce something new have been made repeatedly. For example, the already mentioned modification from M. Ryan, as well as the classification of extrasystoles by frequency and form from RJ Myerburg.
The occurrence of a pathological focus of excitation in the ventricular myocardium with the formation of premature contraction of the heart is called ventricular extrasystole. They can often occur in healthy people (5% of cases).
In the medical community, the most common classification of ventricular extrasystole according to Lown.
Its last modification was in 1975, but it still has not lost its relevance and contains the following classes:
- 0 (no arrhythmia);
- 1 (extrasystoles less than 30/hour, from one source and one form);
- 2 (one source and form, 30 or more extrasystoles per hour);
- 3 (multifocal extrasystoles);
- 4a (paired extrasystoles from one focus);
- 4b (polymorphic extrasystoles accompanied by other arrhythmias - ventricular fibrillation/flutter, tachycardia paroxysm);
- 5 (early extrasystoles “type R on T”).
The mechanism of development of extrasystoles may differ. There are two main ones - reciprocal and automatic. Reciprocal arrhythmias arise when a vicious circle of intraventricular excitation is formed, the so-called “re-entry” mechanism. Its essence lies in the disruption of the passage of a normal signal, which is associated with the presence of at least two paths for the impulse.
In this case, the signal for one of them is delayed, which causes the formation of an extraordinary contraction. This mechanism plays a role in the formation of such arrhythmias as paroxysm of ventricular tachycardia and extrasystoles, Wolff-Parkinson-White syndrome, atrial/ventricular fibrillation. An ectopic focus of excitation can occur with increased automatism of the pacemaker cells of the heart. Arrhythmias with such a development mechanism are called automatic.
Ventricular extrasystoles are a type of arrhythmia that develops as a result of the emergence of additional foci of excitation in the myocardium. As a result, irregular heartbeats appear, disrupting the normal functioning of the organ and leading to poor blood flow. For clinical purposes of patient monitoring, treatment and further prognosis, the 1975 Lown classification of ventricular extrasystole is best suited.
The presence of the degree of arrhythmia in the formulation of the diagnosis is very important. The treatment tactics chosen by the doctor will depend on this.
Thus, the presence of extrasystoles of the first gradation in a patient indicates the functional nature of the resulting abnormal contractions. About 60-70% of people have a similar phenomenon, and this is considered the absolute norm. The only thing required is to periodically check the ECG. However, if you have any symptoms of cardiovascular pathologies, you should undergo additional examination, as this may be one of the debuts of the disease.
In the presence of the second gradation without signs of hemodynamic impairment, non-drug treatment is indicated - auto-training, psychotherapy, avoidance of risk factors. If there are accompanying symptoms or the appearance of polymorphic foci is noticed (third gradation), an appropriate course of antiarrhythmic drugs is required.
Finally, grades four and five, as well as grade three refractory to conservative therapy, especially in the presence of hemodynamic disturbances, require surgical treatment. In this case, surgical interventions such as catheter radiofrequency ablation or pacemaker implantation may be indicated.
This classification is also used to make a forecast. Ventricular extrasystole grade 3-5 according to Lown is considered threatening. These are the so-called malignant arrhythmias. They are characterized by a high risk of sudden death. In this case, the patient should be transferred to the intensive care unit.
The location of the lesions also matters. The prognosis is less favorable in the presence of left ventricular arrhythmias
Lown's classification of ventricular extrasystoles is one of the generally accepted ones, but not all doctors use it.
The classification of PVCs by B. Lown - M. Wolf offers five stages of pathology during a heart attack according to the risk of fibrillation.
The first degree of classification of all ventricular extrasystoles according to Lown is characterized by monomorphic extraordinary contractions (no more than thirty per hour).
As for the second degree, at this stage the frequency of contractions is recorded (more than thirty per hour).
The third degree is characterized by polytopic extrasystole. As for the fourth, it is divided into paired and salvo. Fifth degree - the most dangerous type “R on T” in terms of prognosis is registered, which indicates that the extrasystole “climbs” onto the previous normal contraction and the possibility of rhythm disturbance.
The Lown classification of ventricular extrasystoles offers another degree of zero, in which extrasystoles are not observed.
M. Ryan's classification supplemented the previous gradation for patients without a heart attack. Points one through three are completely identical to Lown’s interpretation. The remaining ones have been slightly changed.
Class 4 ventricular extrasystoles according to Lown are considered in the form of paired extrasystoles in polymorphic and monomorphic variations. Class 5 includes ventricular tachycardia.
Ventricular extrasystole according to Lown, which belongs to the first class, does not have any symptoms or ECG signs of organic pathology.
The remaining classes II-V are very dangerous and belong to organic extrasystoles.
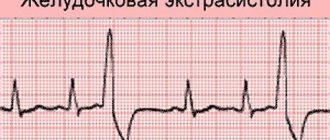
Signs of ECG monitoring of PVCs:
- A change in the QRS complex that appears in advance.
- Deformation and strong expansion of the extrasystolic complex are noted.
- Absence of R wave.
- The likelihood of a compensatory pause.
- There is an increase in the interval of internal deviation in the right chest leads with left ventricular extrasystole and in the left with right ventricular extrasystole.
In addition to the classification of ventricular extrasystole according to Lown, there is also a classification depending on the number of extraordinary impulses. Extrasystoles can be single or paired. In addition, allorhythmia is also distinguished - extrasystole with severe rhythm disturbance. Since in this case there is an increasing appearance of impulses from additional foci, such a rhythm cannot be called completely sinus.
Allorhythmia is represented by three types of disorders: bigeminy (after one normal contraction there is one extrasystole), trigeminy (an extrasystole appears after two contractions), quadrigeminy (after four contractions).
When contacting a cardiologist, in addition to dizziness, malaise and headaches, there are complaints of a feeling of “fading or turning over” of the heart, as well as “thrusts in the chest.”
There are several forms of pathology. According to the number of sources of excitability, extrasystoles are monotopic and polytopic, and according to the time of occurrence - early, interpolated and late. By frequency, group or volley, paired, multiple and single ventricular extrasystoles are distinguished.
Complications
With physiological extrasystole that occurs benignly, without hemodynamic disturbances, complications rarely arise. But if it is malignant, then complications occur quite often. This is precisely why extrasystole is dangerous.
The most common complications of extrasystole are ventricular or atrial fibrillation, paroxysmal tachycardia. These complications can threaten the patient's life and require urgent, emergency care.
In severe forms of extrasystole, the heart rate can exceed 160 beats per minute, which can result in the development of arrhythmic cardiogenic shock and, as a consequence, pulmonary edema and cardiac arrest.
Extrasystole can be accompanied not only by tachycardia, but also by bradycardia. In this case, the heart rate does not increase, but, on the contrary, decreases (there can be up to 30 contractions per minute or less). This is no less dangerous for the patient’s life, since with bradycardia conduction is impaired and there is a high risk of heart block. Source "sosudinfo.ru"
Complications mainly occur with malignant variants with frequent attacks. These include ventricular tachycardia with circulatory failure, ventricular flutter/fibrillation, leading to complete cardiac arrest.
In other cases, the prognosis is often favorable. If all treatment recommendations are followed, even in the presence of concomitant diseases, mortality from this disease is significantly reduced. Source "webmedinfo.ru" The prognosis of VES depends entirely on the severity of the impulse disturbance and the degree of ventricular dysfunction.
With pronounced pathological changes in the myocardium, extrasystoles can cause atrial and ventricular fibrillation, persistent tachycardia, which in the future can lead to death.
If an extraordinary blow during relaxation of the ventricles coincides with contraction of the atria, then the blood, without emptying the upper compartments, flows back into the lower chambers of the heart. This feature provokes the development of thrombosis.
This condition is dangerous because a clot consisting of blood cells, when it enters the bloodstream, becomes the cause of thromboembolism. When the lumen of blood vessels is blocked, depending on the location of the lesion, the development of such dangerous diseases as stroke (damage to the blood vessels of the brain), heart attack (damage to the heart) and ischemia (impaired blood supply to internal organs and limbs) is possible.
To prevent complications, it is important to consult a specialist (cardiologist) in time. Properly prescribed treatment and following all recommendations are the key to a quick recovery. Source "zdorovko.info"
Classification of extrasystole according to Ryan
The modification made changes to grades 4A, 4B and 5 of ventricular extrasystole according to Lown. The complete classification looks like this.
1. Ventricular extrasystole grade 1 according to Ryan – monotopic, rare – with a frequency of less than 30 per hour.
2. Ventricular extrasystole grade 2 according to Ryan – monotopic, frequent – with a frequency of more than 30 per hour.
3. Ventricular extrasystole grade 3 according to Ryan – polytopic VES.
- Ventricular extrasystole grade 4a according to Ryan – monomorphic paired VVCs.
- Ventricular extrasystole grade 4b according to Ryan is a paired polytopic extrasystole.
5. Ventricular extrasystole grade 5 according to Ryan – ventricular tachycardia – three or more VVCs in a row.
general information
Extrasystole means a disturbance in the rhythm of the heart muscle. For various reasons, it may contract prematurely. To determine pathological processes, an electrocardiogram is required. The graph will display an accelerated or premature extrasystolic complex.
It can be parasystolic and extrasystolic
It is important to promptly track these changes to prevent negative consequences and complications. Extrasystole and parasystole are responsible for the work of the main muscle in the body
When their functioning is disrupted, the treatment in both cases is the same.
Extrasystole often occurs in the ventricles of the heart. Pathological processes can occur in the supraventricular region, in the atrium, and atrioventricular muscle.
Ventricular extrasystole - classification according to RJ Myerburg
The Myerburg classification divides ventricular arrhythmias depending on the shape and frequency of PVCs.
Frequency division:
- Rare - less than one ES per hour.
- Infrequent - from one to nine ES per hour.
- Moderate frequency - from 10 to 30 per hour.
- Frequent ES - from 31 to 60 per hour.
- Very frequent - more than 60 per hour.
Division by shape:
- Single, monotopic.
- Single, polytopic.
- Double.
- Ventricular tachycardia lasting less than 30 seconds.
- Ventricular tachycardia lasting more than 30 seconds.
- RJ Meyerburg published his classification in 1984, 13 years later than B. Lown. It is also actively used, but significantly less than those described above.
Ventricular asystole
Ventricular asystole is cessation of electrical and mechanical activity of the ventricles, usually of the entire heart, cardiac arrest. Ventricular asystole leads to cessation of blood circulation and clinical death.
Etiology and pathogenesis. Ventricular asystole is usually caused by severe cardiac
- acute (myocardial infarction, pulmonary embolism) or chronic (ischemic disease
heart disease, hypertension, heart defects, myocarditis, myocardial dystrophy, myocardiopathy, heart surgery), the effects of myocardial depressing antiarrhythmic drugs, excessive vagotonia, reflex effects, electric shock, electric pulse treatment.
In the origin of cardiac
Hypoxia and hypercapnia are of greatest importance. At the same time, the pH of the blood decreases, which causes conduction disturbances up to cardiac arrest. An increase in the tone of the vagus nerve, leading to asystole when the blood pH decreases, also plays a certain role.
Electrolytes are important. Thus, rapid infusion of potassium solutions can lead to asystole.
Along with this, hypokalemia can cause cardiac arrest (more often with intoxication with cardiac glycosides). At the same time, in response to the action of cardiac glycosides, myocardial excitability sharply increases.
Clinic. Ventricular asystole leads to a sudden disappearance of the pulse (not only in the radial artery, but also in the carotid artery), heart sounds, and blood pressure. After a few seconds, the patient loses consciousness, turns pale, and stops breathing. 45 s after the cessation of cerebral circulation, the pupils begin to dilate, reaching a maximum after 1 min 45 s, convulsions, involuntary urination and defecation appear. The electrocardiogram shows a straight line (no electrical activity of the heart).
Diagnostics. It should be borne in mind that circulatory arrest and clinical death are more often associated with ventricular fibrillation than with asystole. And the latter is often preceded by ventricular fibrillation. The clinical picture is the same in both cases. Differentiation can be made only by observing the electrocardiogram on the monitor or by recording the electrocardiogram curve. With asystole, there is no electrical activity of the heart, and therefore a straight line is recorded; with ventricular fibrillation, large or small random biphasic waves are recorded.
Treatment: external cardiac
and artificial respiration - should be started immediately after the first clinical signs of ventricular asystole appear. If the patient was not under electrocardiographic monitoring and there is no certainty that this is not ventricular fibrillation, ventricular defibrillation should be performed. If asystole is diagnosed, electrical stimulation of the heart is necessary as soon as possible. If cardiac stimulation is not possible, 0.5-1 ml of 0.1% adrenaline solution and 5 ml of 10% calcium chloride solution are injected intracardially, norepinephrine, sodium bicarbonate (150-200 ml of 5% solution) are administered intravenously.
The prognosis for ventricular asystole is usually unfavorable. Mortality in certain diseases (for example, heart attack
myocardium) reaches 90-95%.
Prevention of ventricular asystole consists of timely and active treatment
diseases that cause it. The risk of early relapse can be reduced by intramuscular administration of ornid (bretylium tosylate) 0.3-0.6 g every 6 hours. If long-term use for prophylactic purposes is necessary, beta-blockers are the drugs of choice: anaprilin (Inderal, Obzidan) 0.02 -0.04 g, oxprenolol 0.04-0.08 g, cordan 0.05 g 3-4 times a day.
All information on the site, including recipes, is posted and distributed “as is” and does not encourage you to take any action. The site administration is not responsible for the correct description of medications and recipes; one incorrectly defined symptom can lead to an error. We strongly recommend that you consult your doctor.
Classification of extrasystole according to JT Bigger
The diagnosis of VES in itself does not say anything about the patient’s condition. Much more important is information about concomitant pathologies and organic changes in the heart. To assess the likelihood of complications, JT Bigger proposed his own version of the classification, on the basis of which one can draw a conclusion about the malignancy of the course.
In the JT Bigger classification, PVCs are assessed according to a number of criteria:
- clinical manifestations;
- VES frequency;
- the presence of a scar or signs of hypertrophy;
- the presence of persistent (lasting more than 30 seconds) or unstable (less than 30 seconds) tachycardia;
- left ventricular ejection fraction;
- structural changes in the heart;
- influence on hemodynamics.
A PVC with pronounced clinical manifestations (palpitations, fainting), the presence of scars, hypertrophy or other structural lesions, a significantly reduced left ventricular ejection fraction (less than 30%), a high frequency of PVC, the presence of persistent or non-sustained ventricular tachycardia, a minor or pronounced effect is considered malignant. on hemodynamics.
Potentially malignant PVC: mildly symptomatic, occurs against the background of scars, hypertrophy or other structural changes, is accompanied by a slightly reduced left ventricular ejection fraction (30-55%). The frequency of PVCs can be high or moderate, ventricular tachycardia is either unstable or absent, hemodynamics suffer slightly.
Benign PVC: not clinically manifested, there are no structural pathologies in the heart, the ejection fraction is preserved (more than 55%), the frequency of ES is low, ventricular tachycardia is not recorded, hemodynamics do not suffer.
The extrasystole criteria of the JT Bigger classification give an idea of the risk of developing sudden death - the most dangerous complication of ventricular tachycardia. Thus, with a benign course, the risk of sudden death is considered very low, with a potentially malignant course - low or moderate, and the malignant course of VES is accompanied by a high risk of developing sudden death.
Sudden death refers to the transition of PVCs to ventricular tachycardia and then to atrial fibrillation. With the development of atrial fibrillation, a person goes into a state of clinical death. If resuscitation measures are not started within a few minutes (best defibrillation with an automatic defibrillator), clinical death will be replaced by biological death and it will become impossible to bring the person back to life.
Symptoms
Single ventricular premature contractions are recorded in half of healthy young people during monitoring for 24 hours (Holter ECG monitoring). They do not affect your well-being. Symptoms of ventricular extrasystole appear when premature contractions begin to have a noticeable effect on the normal rhythm of the heart.
Ventricular extrasystole without concomitant heart diseases is very poorly tolerated by the patient. This condition usually develops against the background of bradycardia (slow pulse) and is characterized by the following clinical symptoms:
- a feeling of cardiac arrest, followed by a whole series of beats;
- from time to time, separate strong blows are felt in the chest;
- extrasystole may also occur after eating;
- a feeling of arrhythmia occurs in a calm position (during rest, sleep or after an emotional outburst);
- During physical activity, the disturbance practically does not appear.
Ventricular extrasystoles against the background of organic heart diseases, as a rule, are multiple in nature, but for the patient they are asymptomatic. They develop with physical activity and go away while lying down. Typically, this type of arrhythmia develops against the background of tachycardia.
Many women during pregnancy experience tachycardia and pain in the left side of the chest. The development of PVCs in an expectant mother is not uncommon. This is explained by the fact that the circulatory system and the heart have a double burden. In addition, one should take into account the physiological changes in hormonal levels, which affect the rhythm of impulses. Such extrasystole is not malignant and can be easily treated after childbirth.
General information
The factors that caused the development of the disease can be of physiological and pathological origin. An increase in the tone of the sympathetic-adrenal system leads to an increase in the occurrence of extrasystoles. Physiological factors influencing this tone include the consumption of coffee, tea, alcohol, stress and nicotine addiction. There are a number of diseases that lead to the formation of extrasystole:
- cardiac ischemia;
- myocarditis;
- cardiomyopathy;
- heart failure;
- pericarditis;
- hypertonic disease;
- osteochondrosis of the cervical spine;
- prolapse of the mitral valve leaflets;
- cardiopsychoneurosis.
There is a certain connection between the patient’s age, time of day and the frequency of extrasystoles. Thus, more often the ventricular type is present in people over 45 years of age. Dependence on circadian biorhythms is manifested in the registration of extraordinary heart contractions, more in the morning hours.
Ventricular extrasystole threatens the patient’s life. Its formation increases the risk of sudden cardiac arrest or ventricular fibrillation.
Prevention of the disease
The following are usually offered as preventative recommendations:
- maintaining a more active and mobile lifestyle;
- giving up bad habits, including smoking, excessive consumption of alcohol and strong coffee;
- regular medical examinations.
Detection of a disease can occur even during a routine preventive examination; for this reason, a health check in a medical institution is a mandatory event for everyone.
Classification of extrasystoles according to Bigger
Bigger's classification provides for the formation of groups of patients according to the degree of increase in the risk of complications.
It includes the following course of extrasystole:
- malignant;
- potentially malignant;
- benign.
With benign extrasystoles, the risk of complications is extremely low. Moreover, such patients have no signs of pathology of the cardiovascular system in the anamnesis and during examination (normal left ventricular ejection fraction, no hypertrophy or cicatricial changes in the myocardium). The frequency of ventricular extrasystoles does not exceed 10 per hour and there is no clinical picture of paroxysmal ventricular tachycardia.
A potentially malignant disease is characterized by a moderate or low risk of sudden death. The examination reveals structural changes in the heart in the compensation stage. Ultrasound of the heart reveals a decrease in LV ejection fraction (30-55%) and the presence of scar or myocardial hypertrophy. Patients complain of a feeling of interruptions in the work of the heart, accompanied by short-term episodes of ventricular tachycardia (up to 30 seconds).
Malignant extrasystoles are those whose manifestation causes a disturbance in the general well-being of the patient (palpitations, fainting, signs of cardiac arrest). Patients exhibit a critical decrease in ejection fraction - less than 30%. Persistent ventricular tachycardia is also noted.
The most dangerous ventricular ecstasystoles include 3 gradations in the Lown classification - 4a, 4b and 5 classes.
Causes
The reasons for ventricular extrasystole appear in heart disease:
- inflammatory nature (myocarditis, endocarditis, intoxication);
- myocardial ischemia (foci of cardiosclerosis, acute infarction);
- metabolic-dystrophic changes in the muscle and conduction system (impaired potassium-sodium electrolyte ratio in myocytes and intercellular space);
- a sharp depletion of the energy supply of cells caused by malnutrition, lack of oxygen in acute and chronic heart failure, and decompensated defects.
Ventricular extrasystoles may appear in people with a healthy cardiovascular system due to:
- irritation of the vagus nerve (due to overeating, insomnia, mental work);
- increased tone of the sympathetic nerve (smoking, physical work, stress, hard work).
If there are two sources of impulse formation in the heart, then the main one is the one that is capable of a higher frequency. Therefore, normal sinus rhythm is most often maintained. But extrasystoles can also occur against the background of atrial fibrillation.
Clinical manifestations
anxiety, pallor, sweating, fear, feeling of lack of air. Frequent (especially early and group) extrasystoles lead to a decrease in cardiac output, a decrease in cerebral, coronary and renal blood flow by 8-25%. With stenosing atherosclerosis of the cerebral and coronary vessels, transient disturbances of cerebral circulation (paresis, aphasia, fainting), and attacks of angina may occur.
In most patients, in the absence of damage to the cardiovascular and nervous systems, extrasystole occurs hidden. There are no specific complaints inherent to the disease. Its pronounced clinical picture is usually represented by the following symptoms:
- weakness;
- irritability
- dizziness/headaches;
- feeling of discomfort in the chest (pain, tingling, heaviness);
- heart sinking feeling
- a push in the chest with frequent extrasystoles;
- arrhythmic pulse;
- feeling of pulsation in the veins of the neck;
- dyspnea.
The presence of concomitant cardiac pathology aggravates the course of the disease.
Features in children
If a child has been diagnosed with supraventricular extrasystole, then you should first of all monitor his lifestyle and follow a daily routine
It is important to explain to your child that if he does not follow all preventive measures, serious complications may arise that will negatively affect his health.
The child's diet should be varied and balanced. Food should be rich in amino acids, vitamins, proteins, fats, carbohydrates and minerals. The diet should include fruits, vegetables, dairy products, fish and meat. You should minimize the consumption of sweets and junk food.
In order to prevent further development of the pathological condition, it is necessary for the child to have rational physical activity and spend as much time as possible in the fresh air. The baby's condition may worsen due to a cold or infectious disease.
Important! If the child’s condition worsens, you should immediately contact a pediatrician or cardiologist. In some cases, hospitalization is required.
Diagnostics
Making a diagnosis is based on the results of collecting complaints, the history of the patient’s development and life, data from a comprehensive examination and additional studies. Assessing the patient’s condition, the doctor pays attention to increased pulsation of the neck veins, changes in the pulse wave and auscultatory pattern of heart sounds. A standard set of laboratory tests is prescribed (general blood and urine analysis, blood glucose and biochemical blood test), as well as an analysis of thyroid and pituitary hormones.
To obtain an accurate diagnosis, the mandatory criterion is the result of an ECG and daily Holter monitoring. Using these methods, it is possible to accurately determine the source of the pathological focus, the frequency of extrasystoles, the number and relationship with the load. Echo-CG is performed to identify the left ventricular ejection fraction and the presence/absence of structural changes in the heart. If it is difficult to diagnose the disease, MRI, CT, and angiography may be prescribed.
If there are no patient complaints, with a benign course of extrasystole, only monitoring the state of the cardiovascular system is indicated. Such patients are recommended to undergo examination 2 times a year with mandatory ECG registration. The tactics of patient management depend on the number of extrasystoles per day, the course of the disease, and the presence of concomitant pathology. The dosage of drugs is selected individually by the attending physician.
Antiarrhythmic drugs are divided into 5 classes:
- 1a – Na channel blockers (“Procainamide”, “Disopyramide”);
- 1c – K-channel activators (“Difenin”, “Lidocaine”);
- 1c – Na channel blockers (“Flecainide”, “Propafenone”);
- 2 – beta-blockers (“Metaprolol”, “Propranolol”);
- 3 – K-channel blockers (“Amiodarone”, “Ibutilide”);
- 4 – Ca 2 channel blockers (“Diltiazem”, “Verapamil”);
- 5 – Other drugs with antiarrhythmic effects (cardiac glycosides, calcium, magnesium preparations).
For ventricular extrasystole, class 2 drugs are widely used. They help reduce symptoms of arrhythmia and also have a positive effect on the quality of life of patients.
Scientific studies have proven that beta-adrenergic blockers improve the prognosis regarding the risk of cardiac death in patients with cardiovascular pathology.
Persistent ventricular extrasystole according to Lown, which is not amenable to drug treatment, requires surgical intervention. For the success of the operation, it is necessary to accurately know the source of pathological activity. When it is determined, patients undergo implantation of cardioverter-defibrillators or radiofrequency catheter ablation.
Basic principles of treatment
Regardless of the causes of ventricular extrasystole, first of all, the doctor is obliged to explain to the patient that PVC, in itself, is not a life-threatening condition. The prognosis in each specific case depends on the presence or absence of other heart diseases, the effective treatment of which can reduce the severity of arrhythmia symptoms, the number of extrasystoles and increase life expectancy.
Due to the presence of so-called minor psychiatric pathology (primarily anxiety disorder) in many patients with PVCs accompanied by symptoms, consultation with an appropriate specialist may be required.
Currently, there is no data on the beneficial effects of antiarrhythmic drugs (with the exception of beta blockers) on the long-term prognosis in patients with PVCs, and therefore the main indication for antiarrhythmic therapy is the presence of an established cause-and-effect relationship between extrasystole and symptoms, with their subjective intolerance.
The most optimal means for treating extrasystole are beta blockers. The prescription of other antiarrhythmic drugs, and especially their combinations, is in most cases unjustified, especially in patients with asymptomatic extrasystole.
If antiarrhythmic therapy is ineffective or the patient does not want to receive antiarrhythmic drugs, radiofrequency catheter ablation of the arrhythmogenic focus of ventricular extrasystole is possible. This procedure is highly effective (80-90% effective) and safe in most patients.
In some patients, even in the absence of symptoms, antiarrhythmic drugs or radiofrequency ablation may be necessary. In this case, indications for intervention are determined individually. Source "mertsalka.net"
To achieve a good therapeutic effect, you must adhere to a healthy diet and regimen. Requirements that a patient suffering from cardiac pathology must comply with:
- give up nicotine, alcoholic beverages, strong tea and coffee;
- eat foods with a high concentration of potassium - potatoes, bananas, carrots, prunes, raisins, peanuts, walnuts, rye bread, oatmeal;
- in many cases, the doctor prescribes the drug “Panangin”, which contains “heart” microelements;
- give up physical training and hard work;
- during treatment, do not adhere to strict diets for weight loss;
- if the patient is faced with stress or has restless and intermittent sleep, then light sedatives (motherwort, lemon balm, peony tincture), as well as sedatives (valerian extract, Relanium) are recommended.
The treatment regimen is prescribed on an individual basis and depends entirely on morphological data, the frequency of arrhythmias and other concomitant cardiac diseases.
Antiarrhythmic drugs used in practice for PVCs are divided into the following categories:
- sodium channel blockers - “Novocainamide” (usually used for first aid), “Giluri”;
- beta-blockers - “Cordinorm”, “Carvedilol”, “Anaprilin”, “Atenolol”;
- potassium channel blockers - Amiodarone, Sotalol;
- calcium channel blockers - Amlodipine, Verapamil, Cinnarizine;
- if the patient’s extrasystole is accompanied by high blood pressure, then antihypertensive drugs are prescribed - “Enaprilin”, “Captopril”, “Ramipril”;
- to prevent blood clots - Aspirin, Clopidogrel.
A patient who has started treatment is recommended to have a control electrocardiogram after 2 months. If extrasystoles become rare or disappear altogether, then the therapeutic course is canceled.
In cases where the result has improved slightly during treatment, treatment is continued for several more months. In the case of a malignant course of extrasystole, drugs are taken for life.
Surgery is prescribed only in cases of ineffective drug therapy. Often this type of treatment is recommended for patients who have organic ventricular extrasystole.
Types of cardiac surgery:
- Radiofrequency ablation (RFA). A small catheter is inserted through a large vessel into the cavity of the heart (in our case, these are the lower chambers) and using radio waves, problem areas are cauterized. The search for the “operated” zone is determined using electrophysiological monitoring. The effectiveness of RFA in many cases is 75-90%.
- Installation of a pacemaker.
The device is a box equipped with electronics, as well as a battery that lasts ten years. Electrodes extend from the pacemaker and are attached to the ventricle and atrium during surgery. They send electronic impulses that cause the myocardium to contract. The pacemaker essentially replaces the sinus node, which is responsible for rhythm. An electronic device allows the patient to get rid of extrasystole and return to a full life. Source "zdorovko.info"
Treatment goals:
- Identification and treatment of the underlying disease.
- Decrease in mortality.
- Reduced symptoms.
Indications for hospitalization:
- Newly diagnosed PVC.
- Prognostically unfavorable PVC.
Benign ventricular extrasystole, which patients subjectively tolerate well. It is possible to refuse to prescribe antiarrhythmic drugs.
Benign ventricular extrasystole:
- poor subjective tolerability;
- frequent PVC (including idiopathic);
- potentially malignant PVC without pronounced LVH (LV wall thickness not more than 14 mm) of non-ischemic etiology.
Class I antiarrhythmic drugs (allapinine, propafenone, etacizine, moracisine) can be prescribed.
Phenytoin is prescribed for PVCs due to digoxin intoxication. Drugs are prescribed only during the period of subjective sensation of extrasystoles.
It is possible to prescribe sedatives and psychotropic drugs (phenazepam, diazepam, clonazepam).
The prescription of class III antiarrhythmic drugs (amiodarone and sotalol) for benign PVCs is indicated only when class I drugs are ineffective.
Contraindications to the use of class I antiarrhythmic drugs:
- post-infarction cardiosclerosis;
- LV aneurysm;
- LV myocardial hypertrophy (wall thickness >1.4 cm);
- LV dysfunction;
- CHF.
In patients with reduced LV ejection fraction, the prescription of class I antiarrhythmic drugs, aimed only at reducing the number of PVCs, worsens the prognosis by increasing the risk of SCD.
When taking class IC antiarrhythmic drugs (encainide, flecainide, moricizine) to suppress PVCs in patients who had an MI, mortality significantly increased (2.5 times) due to the proarrhythmic effect.
The risk of proarrhythmic action also increases with severe LV myocardial hypertrophy and active myocarditis. All antiarrhythmic drugs of class IA and C must be prescribed with caution in case of conduction disturbances along the bundle branch system and distal AV block of the first degree; in addition, they are contraindicated when the QTc interval is prolonged by more than 440 ms of any etiology.
Verapamil and β-blockers are ineffective in the vast majority of ventricular arrhythmias.
β-Blockers do not have a direct antiarrhythmic effect in ventricular arrhythmias and do not affect the frequency of PVCs. However, by reducing sympathetic stimulation, anti-ischemic effects and preventing catecholamine-induced hypokalemia, they reduce the risk of developing ventricular fibrillation.
β-Adrenergic blockers are used for primary and secondary prevention of SCD; they are indicated for all patients with coronary artery disease and PVCs (in the absence of contraindications). Malignant and potentially malignant ventricular extrasystoles.
Amiodarone is the drug of choice.
Sotalol is prescribed when amiodarone is contraindicated or ineffective.
The addition of β-blockers or co-administration with amiodarone (especially for coronary artery disease) reduces both arrhythmic and overall mortality. Source "cardioplaneta.ru"
Principle of classification
There are many factors that characterize a particular disease. As for extrasystoles, the following signs are distinguished:
- number of ectopic areas (mono-, polytopic);
- form of arrhythmia (mono-, polymorphic);
- frequency of occurrence (rare, moderately frequent, frequent);
- localization (right, left ventricular);
- pattern of abbreviations (ordered, unordered);
- frequency (spontaneous, regular).
In accordance with these parameters, many options were proposed: according to Bigger, Mayerburg. However, the Laun-Wolff classification turned out to be the most practical and popular. Ventricular extrasystole according to Laun is determined using so-called gradations, each of which is assigned one number:
- 0 – no arrhythmias during the last 24 hours of observation;
- I – no more than 30 arrhythmias are observed during an hour of monitoring, monotopic and monomorphic;
- II – more than 30 per hour of the same type;
- III – polymorphic extrasystoles appear;
- IVa – paired monomorphic;
- IVb – paired polymorphic;
- V – characterized by the presence of ventricular tachycardia (extrasystoles that occur more than 3 times in a row).
How to treat ventricular asystole
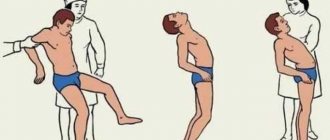
Treatment of asystole or cardiac arrest occurs in three stages:
- emergency help;
- emergency assistance with medications;
- surgical treatment.
First emergency aid in case of cardiac arrest must be provided immediately, since it determines whether the person will survive. First you need to perform an indirect cardiac massage, which is performed by punching the chest area. If special equipment is available, it is necessary to perform defibrillation, connect the victim to a ventilator and provide him with pure 100% oxygen using a mask or endotracheal tube.
If the first emergency aid does not bring the person back to his senses, special medications must be used. These drugs include adrenergic agonists, antiarrhythmic drugs, and M-blockers. Such drugs will help improve the conduction of impulses throughout the organ, thereby increasing the number of heart contractions and restoring normal heart rhythm.
As for surgical treatment, it consists of pericardiocentesis and puncture of the pleural cavity.
Extrasystole against the background of other heart diseases: the role of classification
It is worth noting that the above prognostic signs are correct only in the absence of concomitant diseases, such as myocarditis, valve defects or coronary heart disease. Often they themselves are the causes of abnormal heart contractions.
Extrasystoles of 3, 4, 5 gradations can lead to significant hemodynamic disturbances. Cardiac output decreases, supply to the coronary vessels and brain deteriorates. All this forms a certain vicious circle, which contributes to the further progression of IHD. Also, the presence of this pathology is an indication for a significant change in treatment tactics.
In general, the presence of ischemic disease (especially previous myocardial infarction) significantly worsens the prognosis for a patient even with arrhythmias of grade 2-3 according to Lown.
Ventricular extrasystole is a common heart disease in which myocardial automatism is disrupted. If individual extraordinary contractions are functional in nature and can be present in healthy people, then an increase in frequency and the appearance of several foci indicates the organic nature of the lesion.
For the purposes of differential diagnosis, prognosis and choice of treatment, a simple and effective Lown classification was proposed, which has been successfully used since 1975 to this day.
Traditional methods
If the extrasystole is not life-threatening and is not accompanied by hemodynamic disturbances, you can try to defeat the disease on your own. For example, when taking diuretics, potassium and magnesium are removed from the patient’s body. In this case, it is recommended to eat foods containing these minerals (but only in the absence of kidney disease) - dried apricots, raisins, potatoes, bananas, pumpkin, chocolate.
Also, to treat extrasystole, you can use an infusion of medicinal herbs. It has cardiotonic, antiarrhythmic, sedative and mild sedative effects. It should be taken one tablespoon 3-4 times a day. For this you will need hawthorn flowers, lemon balm, motherwort, heather and hop cones. They need to be mixed in the following proportions:
- 5 parts each of lemon balm and motherwort;
- 4 parts heather;
- 3 parts hawthorn;
- 2 parts hops.
Important! Before starting treatment with folk remedies, you should consult your doctor, because many herbs can cause allergic reactions.