Published: 09.24.2021 14:15:00 Updated: 09.24.2021
Arrhythmia - a disturbance in the rhythm of heart contractions - is associated with heart disease, but is observed in infectious, endocrinological, neurological diseases, injuries, and can also occur in practically healthy people.
Arrhythmias are typically reported in adults, with an aging population suggesting an increase in the prevalence of cardiac arrhythmias. Arrhythmias are often asymptomatic and are more often recorded with Holter monitoring than with a single ECG.
Arrhythmias in adults and children are also detected in complete health:
- in 7% of cases – sinus arrhythmia;
- in 2.9% – sinus tachycardia;
- in 7.8% – sinus bradycardia;
- in 0.5% - supraventricular and 0.6% - ventricular extrasystole;
- 2% are due to 1st and 2nd degree atrioventricular blocks in healthy people;
- 0.2% are occupied by bundle branch blocks, mainly in men, with incomplete blockade typical for young respondents (0.5%), complete blockade for older respondents (1.2%) [2, 4].
Types and causes of arrhythmias
Normal heart rhythm is called sinus rhythm.
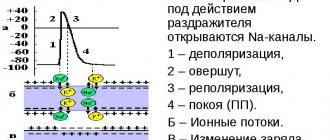
It is determined by the autonomic conduction system of the heart. There are several centers that initiate impulses of electrical activity: normally, the sinus node (the main pacemaker) is of primary importance; the atrioventricular connection (the second pacemaker) is less active; the weakest and most scattered impulses are formed in the His bundles and Purkinje fibers. Arrhythmias are nomotropic and heterotropic, periodic or constant, associated with pathological excitation of myocardial cells. Nomotropic are called dysfunctions of the sinus node, which, however, remains the main pacemaker (sinus arrhythmia). Sinus bradycardia and tachycardia are caused by changes in the rate of impulse occurrence during normal operation of the sinus node.
Sinus tachycardia - increased heart rate. Normal heart rate readings are:
- 90-100 beats per minute. for children under 10 years old;
- 80-90 beats per minute. for children from 10 to 15 years old;
- 64-74 beats per minute. for persons from 15 to 60 years old;
- 50-60 beats per minute. for people over 60 years of age [1].
Causes of sinus tachycardia: physical activity, stress, phobias, neuroses, diseases of the endocrine system, menopause, hypoxia, fever, intoxication, trauma, myocarditis and pericarditis, cardiosclerosis, brain damage.
Sinus bradycardia - a decrease in heart rate - as statistics show, develops mainly in men. In its pathogenesis, hypertonicity of the vagus nerve is important in conditions such as increased intracranial pressure, neoplasms, bruise or concussion, meningitis and encephalitis, hemorrhagic stroke; reflexively hypertonicity of the nerve can develop and lead to arrhythmia - with spasms of renal, gastric, intestinal, or biliary origin.
The activity of the parasympathetic nervous system increases with hypoxia and myocardial ischemia, exposure to quinine, digitalis, morphine, and increased levels of bilirubin and bile acids.
Sinus arrhythmia - the generation of impulses by the sinus node with varying regularity - occurs with an alternate increase in the influence of the sympathetic and parasympathetic nervous systems. The causes of sinus arrhythmia are considered to be changes in the blood levels of oxygen and carbon dioxide, bile acids, lactate, certain medications, hemorrhage in the heart muscle and heart injury.
Heterotopic arrhythmias are associated with failure of the main pacemaker or disruption of their conduction from the sinus node and below. In this case, its functions are taken over by the lower parts of the conduction system, generating replacement rhythms.
Common causes of heterotopic arrhythmias:
- increased activity of the parasympathetic system;
- heart tumors and injuries;
- overstretching of the myocardium (cardiomyopathy);
- poisoning with alcohol, digitalis, quinine, β-blockers;
- infectious diseases (diphtheria, scarlet fever, typhoid fever, influenza and other viral infections);
- hyperkalemia;
- congenital heart diseases.
Arrhythmias of this type are represented by weakness of the sinus node or blockade, mainly in people over 50 years of age;
sinoatrial and atrioventricular blocks, blockade of one or both branches of the His bundle. In these cases, the rhythm of heart contractions is set by weaker pacemakers, since normal conduction is not carried out. The rhythm of heart contractions is disrupted when the excitation of myocardial cells changes. The causes of such violations are: IHD; violations of water-salt balance; hypoxia; chronic intoxication; injuries to the chest, heart, brain; cholecystitis, urolithiasis. Disorganization of the heart rhythm is also associated with abnormalities of large vessels and disorders of neurohumoral regulation. As a result, arrhythmias such as flickering, fluttering and paroxysmal tachycardia are formed. Abnormal automaticity is associated with ischemia or infarction, increased potassium ions and tachycardia.
Extrasystoles - additional, outside the main rhythm, heart contractions, followed by a longer pause - can be single, paired, multiple, associated with the rhythm. Paroxysmal tachycardia is a temporary sudden increase in heart rate, followed just as suddenly by its normalization. During this period, the heart is less well supplied with blood due to a decrease in minute volume, blood pressure decreases, dizziness, heart pain, and loss of consciousness are possible. Paroxysmal supraventricular tachycardia is registered 2 times more often in women, paroxysmal ventricular tachycardia – in men. Flutter - very frequent regular contractions of the atria (up to 380 per minute) and ventricles (up to 300 per minute) - are associated with the appearance of re-entry foci in the right atrium.
Atrial fibrillation has a more severe course. Fibrillation - irregular contractions of the atria or ventricles due to erratic electrical activity of the heart - is caused by multiple re-entry foci generating impulses at a very high frequency. Blood stagnates in the atria and blood clots form. Atrial fibrillation is characterized by the appearance of several foci generating frequent impulses, but no actual contraction of the ventricle occurs. Atrial fibrillation never occurs in healthy people.
When do interruptions in the functioning of the heart of organic origin occur?
As for extrasystoles of organic origin, this is the result of pathological changes in the heart itself in the form of the following diseases:
- IHD, such as previous myocardial infarction
- myocardial dystrophy
- cardiosclerosis
- various channelopathies (long QT syndrome, Brugada syndrome)
- the presence of congenital additional pathways (for example, WPW syndrome)
- dilated cardiomyopathy
- atrial enlargement
- myocarditis
- acquired and/or congenital heart defects (for example, atrial septal defect or aortic valve stenosis)
- pericarditis and other heart diseases
The reason for this extrasystole is the presence of a focus, for example, scar tissue, which has an unfavorable prognostic value.
The causes of paroxysmal (episodic) heart rate accelerations are approximately the same. With all the components, supraventricular rhythm disturbances are safer, in contrast to ventricular ones.
Symptoms of arrhythmia
- Feeling of interruptions and sinking heart.
- Palpitations, “fluttering” in the fingertips.
- Pain in the heart area.
- Dyspnea.
- Edema.
- Increased fatigue.
- Fear.
- Presyncope and fainting.
- Sleep disorders.
Children may have a delay in the rate of psychomotor development, tearfulness, and chest deformation.
Children experience vomiting, anxiety, shortness of breath, refusal to eat, and cold sweat. In some cases, arrhythmias are signs of life-threatening conditions:
- arrhythmic collapse or shock;
- heart failure;
- myocardial ischemia (acute coronary syndrome);
- sudden cardiac death.
Arrhythmia in children
Arrhythmias in children can appear at any age, but are more common during the neonatal period, at 4-5, 7-8 years and in adolescents [3].
In many cases, arrhythmias are asymptomatic and are detected during routine examinations. The higher prevalence of arrhythmias in children of pubertal age is associated with hormonal age-related changes. In this case, children complain of palpitations during exercise or at rest, weakness, fatigue, headaches, insomnia, periodic chest pain and increased blood pressure. Heart failure develops quickly, especially in children of the first year of life, and can lead to sudden cardiac death syndrome. Other causes of arrhythmia in childhood:
- damage to the nervous system in the perinatal period;
- congenital dysregulation (immaturity) of autonomic regulation of cardiac activity;
- childhood infections or previous congenital infections;
- endocrinological diseases;
- dehydration with prolonged vomiting, diarrhea, sweating;
- hypo- and hyperthermia;
- congenital and acquired heart defects and conduction tract anomalies.
Complicated pregnancy and childbirth, fetal malnutrition, prematurity, intrauterine infections contribute to arrhythmias in children, and, as a rule, in children with a history of arrhythmias, various cardiac diseases are detected in close relatives.
When do interruptions of functional origin occur?
The functional nature of extrasystoles is spoken of when a person does not have significant heart damage, and the main cause of interruptions is a temporary change in the electrolyte composition of the heart.
Most often in this situation, extrasystoles occur in the following cases:
- Emotionally labile persons with signs of neurocirculatory dystonia
- Severe mental or physical stress
- Smoking
- Coffee abuse
- Alcohol abuse
- Use of narcotic drugs
- Energy
They may also occur against the background of the following diseases and conditions:
- Stomach ulcer
- Cholelithiasis
- Hiatal hernia
- After a large meal
- In a dream
- Hormonal disorders (for example, thyroid dysfunction in the form of hyper/hypothyroidism)
- Cervical osteochondrosis
- When taking certain medications
Diagnostics
Of course, the central role in the diagnosis of arrhythmias is played by electrocardiogram analysis, single ECG recording or 24-hour (Holter) monitoring.
An ECG with stress and functional studies are performed. Sometimes a revil-implantable device is installed that continuously records the ECG for several months. Additionally, an electroencephalogram, genetic testing, MRI or CT scan of the heart, and echocardiography are performed. Laboratory methods for diagnosing arrhythmias in order to identify electrolyte disturbances and signs of inflammation deserve special attention. Blood, urine, nail or hair tests are taken to determine the levels of magnesium, potassium, sodium, and chlorine. Blood tests are more revealing.
You can perform a complex laboratory test "Cardiorisk", including determination of troponin levels, NT-pro BNP; C-reactive protein, homocysteine, triglycerides, lipoprotein, creatine kinase, LDH, cholesterol, low and high density lipoproteins, D-dimer.
To monitor the effectiveness of treatment, a study of the level of drugs amiodarone, lidocaine, procainamide in the blood is prescribed using high-performance liquid chromatography.
Prevention
To prevent attacks of nocturnal tachycardia from occurring, the best way out is to reduce the load from both physical labor and emotions, adhere to an active lifestyle that can enhance the reserve capabilities of the human body and bring the pulse back to normal.
You need to take control of the number of hours spent motionless (at the computer), remove all “nicotine poisoning sessions” from the regime, and avoid drinking 8 cups of coffee a day, especially before going to bed.
It is better to avoid heavy meals before bedtime and reduce the amount of quickly digestible carbohydrates. The body should receive almost the entire daily dose of calories in the first half of the day. Before going to bed, you should not engage in physical activity; it is better to take a walk or take a relaxing shower.
Treatment of arrhythmia
Treatment can be conservative or surgical.
In severe cases, surgical interventions are performed to install an artificial pacemaker, cardioverter-defibrillators, radiofrequency and cryoablation (destruction of the focus generating pathological impulses with electricity or deep freezing). In emergency cases, intravenous administration of antiarrhythmic drugs is prescribed. First aid for arrhythmia in children is to provide fresh air, clear the airways and ensure rest. In the first minutes, you can apply an ice pack to the child’s face, tilt his head down for a couple of minutes, and press on the root of the tongue. Drug therapy is used as prescribed by the doctor. The choice of drug depends on the type of arrhythmia and the individual characteristics of the patient. Tablets for arrhythmia are prescribed by a cardiologist or therapist; you cannot take them yourself. Besoprolol, amiodarone, nadolol, atenolol or other β-blockers are prescribed.
Bibliography
- Guzovskaya, E.V. Pathophysiology of the heart: textbook/ / E.V. Guzovskaya, S.F. Nepomnyashchy; GBOU VPO IGMU of the Ministry of Health of Russia - Irkutsk, IGMU - 48 p.
- Zatonskaya, E.V. Epidemiology of arrhythmias (review of literature data)/ E.V. Zatonskaya, G.V. Matyushin, N.G. Gogolashvili, N.N. Novgorodtseva - Text: direct // Siberian Medical Review, 2021.- No. 3.- P.5-16.
- Sozonov, A.V. The role of a single-channel electrocardiogram at home in the diagnosis of heart rhythm disorders in children / A.V. Sozonov, Yu.A. Trunova, O.S. Pokusaeva-text: direct // Russian Journal of Cardiology, 2021.-No. 24 (add.) – P. 18-19.
- Hingorani P., Natekar M., Deshmukh S., Karnad DR, Kothari S., Narula D., Lokhandwala Y. Morphological abnormalities in baseline ECGs in healthy normal volunteers participating in phase I studies // Indian. J. Med. Res. - 2012. - Vol. 135. - P. 322-330.
Author:
Pugonina Tatyana Alekseevna, Therapist