Under normal conditions, in a healthy person, the heart contracts rhythmically. The rhythm is provided by periodically occurring excitation processes in the heart muscle itself, causing contractions of the atria and ventricles in a certain sequence and making up the above-described heart cycle.
An abnormal heart rhythm is called arrhythmia. There are many types of arrhythmias. The frequency, sequence, or strength of contractions may change. Too rare heart contractions (less than 60 per minute) are called bradycardia, and frequent ones (more than 100 per minute) are called tachycardia.
Depending on the location of the source of excitation leading to arrhythmia, supraventricular (atrial) and ventricular arrhythmias are distinguished.
It is not always possible to accurately determine the cause of the disease, because there can be many such causes. Arrhythmia can develop after a myocardial infarction, when damage to the heart muscle makes it difficult to carry out normal impulses. More than 80% of patients with acute myocardial infarction experience arrhythmias. Arrhythmia can be caused by a violation of the metabolism of mineral substances - potassium, magnesium, calcium, sodium, which play an important role in the processes of occurrence and propagation of electrical impulses in the heart. Arrhythmia can also be caused by certain medications, such as cardiac glycosides. Disturbances in the nervous regulation of heart activity can contribute to the development of arrhythmia. If the arrhythmia threatens the health (and in some cases it can threaten the life) of the patient, medications are prescribed to help reduce its manifestations.
Most existing antiarrhythmic drugs can be divided into three main groups according to the predominant mechanism of action:
Rating of drugs for arrhythmia
When selecting appropriate medications, VyborExpert relied on the recommendations of leading cardiologists, after which effective and time-tested drugs were assessed for the following characteristics:
- Form of the disease;
- Presence of concomitant disorders;
- Patient's age;
- Composition of the drug;
- Mechanism of action;
- Presence of additional risk factors;
- Release form, ease of use;
- Contraindications, risks of side effects;
- Safety, bioavailability;
- Course duration, price.
The result of the comparative analysis was a list of drugs for arrhythmia consisting of 9 nominees. For convenience, they were divided into 5 groups according to the principle of action. These are both preventive and therapeutic agents. Thanks to customer reviews, it was possible to determine the strengths and weaknesses of each.
The best membrane stabilizing drugs
A set of therapeutic measures may include membrane-stabilizing medications, the principle of action of which is aimed at blocking the excitability of the heart muscle. Elimination of this cause is appropriate for all types of disease, except for the sinus type, since medications of this type do not affect the cells of the sinus node. 2 nominees received the best reviews, as well as approval from cardiologists.
Lidocaine
The rating opens with a well-known local anesthetic that has found application in the treatment of cardiac arrhythmia. Available in the form of ampoules with a liquid solution for injection, one package contains 10 pieces. It aims to block both open and inactivated sodium channels. At the same time, there is no effect on the internal conductivity of the heart, the time of contraction and widening of the ventricular QRS complex.
The drug is also valued for its selective effect on myocardial tissue and does not affect the tone of the autonomic nervous system or blood pressure. Most often, doctors prescribe Lidocaine for ventricular cardiac arrhythmias in order to restore the membrane after an impulse, including tachycardia and extrasystole. The tablet form is not used for home treatment.
Advantages:
- Stabilizing effect on the membrane;
- Acceleration of recovery after an impulse;
- Anesthetic effect;
- No effect on pressure;
- Minimal contraindications;
- Inexpensive.
Flaws:
- For internal administration only;
- Contraindications.
Hypotension, liver pathologies, and convulsive conditions are considered contraindications. For urgent help, 4 ml of a 2% solution injected into a vein will be sufficient. Subsequently, droppers of 1 ml of 4% are placed.
Propanorm
The sodium channel blocker Propanorm demonstrates good results in the complex treatment of this disease. Its action is aimed at preventing a wave of excitation in the myocardium, thereby normalizing the heart rhythm. The product is available in two forms - a solution for internal administration by injection, tablets for oral administration.
The active substance is propafenone hydrochloride, a local anesthetic. The effect occurs 1 hour after administration, lasting another 12 hours. Most often, doctors prescribe “Propanorm” for ventricular/supraventricular extrasystoles, for the purpose of prevention. The mandatory condition for the patient is the age of majority. Due to its arrhythmogenic effect, overdose is dangerous.
Advantages:
- Anesthetic effect;
- Sodium channel blockade;
- Different forms for administration;
- Performance;
- Prevention of attacks;
- Price.
Flaws:
- Admission restrictions;
- Risks of overdose.
You must take Propanorm as prescribed by your doctor. Much depends on age and weight, for example, if you are 70 kg, 150 mg of the active ingredient three times a day will be enough. Contraindications – severe heart failure, arterial hypotension, heart attack, bradycardia.
Low blood pressure with tachycardia
First aid is as follows:
- you need to lie down and raise your legs,
- drink sweet tea. The use of coffee and caffeinated drinks is prohibited,
- take a deep breath and hold your breath for a while,
- It is possible to use sedatives - motherwort tincture.
If the condition does not improve, lethargy, weakness, and dizziness appear, then it is necessary to urgently call an ambulance.
The hospital will conduct a set of necessary examinations to determine the cause of tachycardia due to hypotension. Based on the data obtained during diagnosis, a diagnosis is made and a treatment plan is prescribed.
Treatment is mainly aimed at eliminating the etiological factor that caused the increased heart rate. The complex of treatment measures also includes taking vitamins and physiotherapeutic procedures.
- Tachycardia folk treatment - healthy lifestyle recipes
The best beta blockers for arrhythmia
Thanks to such means, it is possible to reduce the need of the heart muscle for oxygen supply, as well as stop the functions of catecholamines. Cardiologists prescribe this group of medications to patients with sinus-type disease or caused by insufficient blood microcirculation. The list of beta blocker drugs for cardiac arrhythmia included 2 leaders according to reviews and assessments by cardiologists.
Metoprolol
The first in this category is a drug for normalizing cardiac activity. In terms of composition, it is a beta1-blocker with a wide spectrum of effects, but of a selective type. Another difference from analogues is the prolonged effect. The active substance is metoprolol succinate, which has antiarrhythmic, antihypertensive, and antianginal effects.
That is, proper use of tablets reduces blood pressure, prevents it from jumping, and prevents heart rhythm disturbances and angina attacks. The therapy also helps slow the pulse, muscle contractility, reduce the volume of ejected blood and myocardial excitability. The effect develops gradually, reaching a maximum after 2 weeks of the course.
Advantages:
- Large list of indications;
- Selective action;
- Possibility of use for prophylactic purposes;
- Bioavailability;
- Prolonged effect;
- Decreased heart rate and blood pressure.
Flaws:
- Withdrawal syndrome;
- Risks of side effects.
The standard treatment regimen is 100 mg in one or two doses per day, gradually increasing the dose to 200-400 mg. The product is not recommended for low blood pressure, heart failure, impaired peripheral blood supply, or lactation.
Anaprilin
Tablets for arrhythmia of non-selective action, designed to normalize heart rhythm by influencing blood pressure, the sympathetic nervous system, and pulse. The active substance is propranolol hydrochloride, which reduces the frequency of muscle contractions and blood pressure. The list of indications also includes tachycardia, angina pectoris, extrasystole, and hypertension.
The tablet form can be of 3 types depending on the concentration of the active substance - 10, 50, 100 mg. Medical practice shows that the correct use of Anaprilin has a beneficial effect on the myocardium, eliminates dizziness, shortness of breath, and discomfort in the chest area. Improvement occurs within 30 minutes, even faster if administered by injection.
Advantages:
- Calm, lower blood pressure;
- Quick relief;
- Help with VSD, panic attacks;
- “First aid” for rhythm disturbances;
- Availability;
- Inexpensive.
Flaws:
- Lots of side effects;
- Specific taste.
Treatment in this way is unacceptable for acidosis, acute infarction, peripheral circulatory disorders, bronchospasms, and sinus bradycardia. Otherwise, start with 20 mg three times a day with a gradual increase in dose. For better digestibility, this should be done half an hour before meals.
How to take medications and control your condition?
Each patient taking tablets for arrhythmia should be regularly monitored by a doctor. Timely examination allows you to assess the effectiveness of therapy, identify side effects in the early stages and take measures to eliminate them. During the examination, the doctor evaluates the following indicators:
- General condition and complaints of the patient.
- Blood pressure numbers.
- Pulse.
- Heart rate.
- Heart rhythm according to electrocardiogram or Holter monitoring results.
- State of the cardiovascular system according to ultrasound and echocardiography.
- General blood test, coagulogram, biochemical parameters, lipid profile.
- Electrolytes in the blood.
- Kidney and liver tests.
- Hormones.
The best calcium and potassium channel blockers for arrhythmia
When potassium and sodium leave the myocardial cells, they become excited. Therefore, doctors can prescribe special medications to prevent this. Calcium channel blockers will also help, as they slow down the formation of signals in the sinus node, the speed of their movement through the myocardium, and also contribute to partial inhibition of atrioventricular conduction.
Amiodarone
List of modern iodine-based anti-arid drugs for widespread use in hospital settings. The drug promotes vasodilation, which has a beneficial effect on heart rate. It also prevents the excretion of intracellular potassium, thereby slowing down repolarization. The tablet form assumes a dosage of 200 mg of the active ingredient, 30 or 60 pieces per package.
Indications for use: ventricular flutter, tachycardia. Unlike many analogues, this remedy is highly effective for supraventricular and ventricular cardiac arrhythmias. A long elimination period ensures that tablets are taken infrequently. In addition, Amiodarone is approved for people with heart failure, since it does not affect ventricular function.
Advantages:
- High arrhythmolytic efficiency;
- Elimination of ventricular fibrillation;
- Moderate a-blocking, antioxidant;
- Long removal process;
- Children allowed;
- No effect on ventricular function.
Flaws:
- Risks of arrhythmogenic effect;
- Possibility of extracardiac side effects.
A common prescription regimen is 600 mg per day for a week, usually divided into 3 doses. After this, the dosage is gradually reduced until normal health is restored. For children, 200 mg per day is sufficient. Tablets are prohibited for pathologies of the thyroid gland, respiratory system, pregnancy, and lactation.
Cordaron
The leader among drugs for atrial fibrillation, which has a positive effect on energy metabolism in the myocardium. It is based on the substance amiodarone hydrochloride, which blocks the electrical signals that cause irregular heartbeats. In addition, the composition will partially block potassium, calcium, and sodium channels. The product is presented in tablet form, as well as liquid for injection.
Uniqueness - a combination of calcium/sodium/potassium blocker properties with a beta-adrenergic blocking effect. Regular use reduces the sensitivity of the heart to stress hormones and the effect of thyroid hormones on the myocardium. Cordarone is highly valued because it is approved for chronic heart failure. The therapeutic properties develop gradually and last up to 3-6 months.
Advantages:
- Prevention of angina attacks;
- Pulse equalization;
- Multifunctionality;
- Protection from the negative effects of hormones;
- Allowed for heart failure;
- Long-lasting cumulative effect.
Flaws:
- List of contraindications, risks;
- Price.
The initial dose is 800 mg, divided into several doses. Then, as they feel better, they are reduced to 400 mg by the second week. And after that, to maintain the results obtained, 200 mg will be enough. Cordarone is definitely not allowed for people under 18 years of age or for pregnant or breastfeeding women.
The best anticoagulant for arrhythmia
To facilitate blood circulation through the vessels and through the heart, anticoagulants are used. They thin the blood and prevent the formation of blood clots. It is especially important to take such drugs for atrial fibrillation. In this case, tablet forms are used to complete the course. One nominee, approved by leading cardiologists, is recognized as the leader of this category.
Aspirin
An antiplatelet drug with clinically proven efficacy and safety. The mechanism of action is inhibition of platelet cyclooxygenase-1, due to which platelets are released and the blood thins. Patients with arrhythmia are prescribed this drug for the purpose of primary prevention of stroke; these are persons no older than 65 years. The antiplatelet effect also prevents heart attack.
Acetylsalicylic acid is well absorbed from the gastrointestinal tract, making it active within 1-2 hours and throughout the day. The tablet form is available in different dosages - 50-150 mg. Despite the safety of the composition, it is important to consult a doctor due to its ulcerogenic effect, which can cause ulcers, bleeding, and erosion of the gastric mucosa. Aspirin is allowed from 15 years of age.
Advantages:
- Blood thinning;
- Antipyretic, analgesic effect;
- Prevention of blood clots, heart attack, stroke;
- Anti-inflammatory effect;
- No negative effect on blood pressure;
- Inexpensive.
Flaws:
- Risks of bleeding, ulcers, erosions;
- Contraindications.
The daily dose recommended by doctors is from 40 to 1000 mg, divided into several doses (from 2 to 6 times). If the patient has diabetes mellitus, thyrotoxicosis, ischemia, as well as over the age of 65-75 years, Aspirin is contraindicated.
Diagnostics
Of course, the central role in the diagnosis of arrhythmias is played by electrocardiogram analysis, single ECG recording or 24-hour (Holter) monitoring.
An ECG with stress and functional studies are performed. Sometimes a revil-implantable device is installed that continuously records the ECG for several months. Additionally, an electroencephalogram, genetic testing, MRI or CT scan of the heart, and echocardiography are performed. Laboratory methods for diagnosing arrhythmias in order to identify electrolyte disturbances and signs of inflammation deserve special attention. Blood, urine, nail or hair tests are taken to determine the levels of magnesium, potassium, sodium, and chlorine. Blood tests are more revealing.
You can perform a complex laboratory test "Cardiorisk", including determination of troponin levels, NT-pro BNP; C-reactive protein, homocysteine, triglycerides, lipoprotein, creatine kinase, LDH, cholesterol, low and high density lipoproteins, D-dimer.
To monitor the effectiveness of treatment, a study of the level of drugs amiodarone, lidocaine, procainamide in the blood is prescribed using high-performance liquid chromatography.
Other antiarrhythmic drugs for arrhythmia
Cardiovascular pathologies are one of the most common problems of humanity, so pharmaceutical companies and medical specialists are constantly creating new drugs. We conducted a study of new products presented by pharmacy chains. The review included the 2 best drugs for cardiac arrhythmia of the latest generation.
Coraxan
Antianginal, anti-ischemic drug in tablet form for oral administration, which is based on the new agent ivabradine. It effectively prevents increased heart rate. At the same time, there is no negative effect on contractility, intracardiac conduction, or ventricular repolarization processes, which reduces the likelihood of side effects.
The uniqueness of this substance lies in the dose-dependence of the reduction in heart rate. The plateau effect (no increase in therapeutic effect) prevents the risk of developing bradycardia. Coraxan is approved even for people with diabetes, since the active ingredient, which relieves anxiety symptoms, does not affect the metabolism of lipids and glucose.
Advantages:
- Fast safe absorption;
- Normalization of pulse;
- Lack of influence on other processes of the heart and blood vessels;
- Elimination of symptoms of angina pectoris, tachycardia;
- No withdrawal syndrome;
- Allowed for diabetics.
Flaws:
- Contraindications based on age, health status;
- Price.
The daily dosage is selected by the doctor individually for each patient; it is divided into 2 doses. Usually start with 5 mg, gradually increasing after 3-4 weeks. Contraindications – pregnancy, age under 18 years, bradycardia, acute heart attack, unstable angina, etc.
Panangin
This nominee belongs to the group of electrolytes that replenish the lack of important microelements for the full functioning of the cardiovascular system. The vitamin composition includes 2 components - magnesium and potassium salts. In this regard, “Panangin” acts as an auxiliary means of complex treatment. By improving metabolic processes, it provides an antiarrhythmic effect.
The nominee is especially useful for rhythm disturbances associated with electrolyte imbalance. Despite the safety of the components, irrational use can cause problems with the respiratory system. Parallel use with other medications against such pathologies enhances their effectiveness and improves nervous regulation.
Advantages:
- Vitamin composition;
- Safety;
- Increasing the effectiveness of antiarrhythmics;
- Beneficial effect on nervous regulation;
- Ease of use;
- Price.
Flaws:
- Risks of respiratory depression;
- Only an aid.
For better absorption, the tablets should be taken with meals, the optimal regimen is 2 tablets per day for a month. After this, be sure to take a break so as not to provoke an overdose. "Panangin" is prohibited in case of acid metabolism disorders, kidney or liver failure.
How to choose a drug for arrhythmia
It is impossible to choose medications for the treatment of abnormal heart rhythms on your own. To avoid harm to your health, consult your doctor. What to buy at the pharmacy largely depends on the form of arrhythmia determined by the cardiologist and concomitant pathologies. There are also a number of other factors in individual development of a treatment regimen.
The doctor's consultation
The list of medications and the regimen for taking them is prescribed only by a specialist, a cardiologist. We are talking about a whole group of antiarrhythmic drugs, which are selected only after diagnosis. If you do not solve the problem comprehensively, there is a high probability of relapses and complications. Self-medication, incorrect choice of dosages, all this threatens with serious side effects.
Form of arrhythmia
The choice of medications depends on what form of heart rhythm disturbance the doctor has diagnosed. The generally accepted classification considers nootropic, heterotropic form, atrioventricular block, changes/disturbances in excitability, conductivity or excitatory function. The type of pathology depends on the reasons that provoke it. Each case is individual, as is the treatment plan.
Presence of other diseases
Since we are talking about a disease of the cardiovascular system, there is a high probability of developing associated disorders. Medical practice considers sinus bradycardia or tachycardia, atrial fibrillation or flutter, reciprocal AV nodal or ventricular tachycardia, atrial/ventricular extrasystole. Depending on this, auxiliary means are selected.
Other selection factors
There are a number of minor factors that determine which agents are appropriate in treatment. The first is the severity of the pathology. The specialist also takes into account the patient’s age, for example, drugs for arrhythmia for older people should not affect blood pressure. Take into account the contraindications in the instructions so as not to encounter side effects.
Which drug for arrhythmia is better?
As part of drug therapy, the doctor selects primary and auxiliary drugs. The most popular groups are considered in our rating. The assessment criteria and recommendations of Vyborexperta.ru will simplify the choice of how to treat such a pathology:
- Propanorm is a sodium channel blocker with local anesthetic action for the prevention of attacks;
- Metoprolol is a selective beta1-blocker with good bioavailability and prolonged effect;
- Cordarone – 2 in 1 remedy against atrial fibrillation, calcium/sodium/potassium blocker + beta-adrenergic blocking agent;
- Aspirin is the best prevention of blood clots, stroke, heart attack, anti-inflammatory, antipyretic properties;
- Panangin is an electrolyte with an antiarrhythmic effect, a source of magnesium and potassium, prevention for the elderly.
Two patients with a similar clinical picture may benefit from different treatment regimens. Therefore, self-medication, which increases the risk of worsening the situation to a critical condition, is strictly prohibited. Our rating is designed to help narrow your search for reliable, proven drug names.
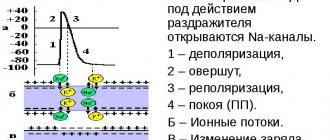
Mechanism of action
The mechanisms of action of antiarrhythmic drugs have not yet been clarified. However, many drugs have similar effects. Antiarrhythmic drugs change the flow of sodium, potassium and calcium ions across the cardiomyocyte membrane, resulting in a change in its electrical potential. The main electrophysiological effect is a change in the speed and duration of AP phases, the speed of electrical impulse conduction, refractoriness and automaticity of the heart muscle.