- General characteristics Definition of hypoxia
- Development of hypoxia
- Exogenous hypoxia
Hypoxia is a pathological condition in which oxygen deficiency occurs in the body due to its reduced supply from the outside and/or due to dysfunctional utilization in cells.
hypoxia
“Hypoxia” – hypo and oxigenium (lack of oxygen), translation from ancient Greek. Most people understand hypoxia as oxygen starvation (lack of oxygen) , because... in this case, tissues and organs experience dysfunction from oxygen deficiency.
General characteristics of hypoxia
Definition of hypoxia
Hypoxia is a typical and dangerous pathological process that occurs in the body during a wide range of diseases and acute conditions, and provokes them. For example, hypoxia can be caused by various factors, and also accompany a wide range of diseases, and may even be the main link in the appearance of pathological changes or diseases.
Based on this:
hypoxia is a typical general pathological process and does not relate to either a diagnosis or a syndrome.
The effect of hypoxia at the cellular level is divided into two types - adaptive reactions and decompensation .
During the occurrence of hypoxia, the body launches adaptive protective reactions that maintain for a short time the almost normal functioning of organs and tissues. With prolonged exposure to hypoxia, the body's reserves run out and adaptive defense reactions are switched off - decompensation occurs.
Decompensation is characterized by the occurrence of irreversible disorders in organs and tissues - from organ failure to death.
Development of hypoxia
Compensatory reactions during hypoxia are expressed by oxygen deficiency at the cellular level, and their task is to restore the amount of oxygen in tissues. The complex of compensatory reactions to eliminate the influence of hypoxia includes the organs of the cardiovascular and respiratory systems, and changes in biochemical processes in tissues and organ structures that suffer most from oxygen deficiency are triggered. Until the supply of compensatory reactions is completely exhausted, organs and tissues will not suffer from a lack of oxygen. However, if, when compensatory mechanisms are depleted, the supply of oxygen is not normalized, then irreversible decompensation will begin in the tissues with damage to cells and dysfunction of the entire organ.
In acute and chronic hypoxia, the nature of compensatory reactions is different. Thus, during acute hypoxia, compensatory reactions consist of increased breathing and blood circulation, that is, blood pressure rises, tachycardia occurs (heart rate more than 70 beats per minute), breathing becomes deep and frequent, the heart pumps a larger volume of blood per minute than normal . In addition, in response to acute hypoxia, all “reserves” of red blood cells, which are necessary to carry oxygen to the cells, are released into the systemic circulation from the bone marrow and spleen.
hypoxia
All these reactions are aimed at normalizing the amount of oxygen delivered to the cells by increasing the volume of blood passing through the vessels per unit of time and increasing the amount of oxygen transferred. With very severe acute hypoxia, in addition to the development of these reactions, centralization of blood circulation also occurs, which consists of redirecting all available blood to vital organs (heart and brain) and a sharp decrease in blood supply to the muscles and organs of the abdominal cavity. The body directs all the oxygen to the brain and heart - organs critical for survival, and, as it were, “deprives” those structures that are currently not needed for survival (liver, stomach, muscles, etc.).
If acute hypoxia is eliminated without depleting the body's reserves, then the person will survive, and all his organs and systems will function completely normally after some time. If hypoxia continues longer than the period of effectiveness of compensatory reactions, then irreversible changes will occur in organs and tissues.
Compensatory reactions during chronic hypoxia develop against the background of severe long-term diseases or conditions. First, to compensate for oxygen deficiency, the number of red blood cells in the blood increases, which allows the volume of oxygen carried by the same volume of blood per unit time to increase. Also, in red blood cells, the activity of an enzyme increases, facilitating the transfer of oxygen from hemoglobin directly to the cells of organs and tissues. New alveoli are formed in the lungs, breathing deepens, the volume of the chest increases, additional vessels are formed in the lung tissue, which improves the supply of oxygen to the blood from the surrounding atmosphere. The heart, which has to pump more blood per minute, hypertrophies and increases in size. Changes also occur in tissues - the number of mitochondria (organelles that use oxygen to ensure cellular respiration) increases in cells, and many new capillaries are formed in tissues. It is precisely because of the activation of microcirculation and a large number of capillaries during hypoxia that a person develops a pinkish coloration of the skin, which is mistaken for a “healthy” blush.
Adaptive reactions during acute hypoxia are reflexive, and therefore, when oxygen starvation is eliminated, they cease their effect, and the organs completely return to the mode of functioning in which they existed before the development of the episode of hypoxia. In chronic hypoxia, adaptive reactions are not reflexive; they develop due to the restructuring of the functioning mode of organs and systems, and therefore their action cannot be quickly stopped after oxygen starvation is eliminated.
With chronic hypoxia, the body can change its functioning mode in such a way that it completely adapts to conditions of oxygen deficiency and does not suffer from it at all. For example, this is how the body of residents of megacities adapts.
In acute hypoxia, complete adaptation to oxygen deficiency cannot occur, since the body simply does not have time to rearrange its functioning modes, and all its compensatory reactions are designed only to temporarily maintain the functioning of organs until adequate oxygen delivery is restored.
That is why a person can have a state of chronic hypoxia for many years without interfering with his normal life and work, while acute hypoxia in a short period of time can lead to death or irreversible damage to the brain or heart.
Compensatory reactions during hypoxia always lead to changes in the functioning of the most important organs and systems. These manifestations of compensatory reactions can be conditionally considered symptoms of hypoxia.
Why does hypoxia occur?
The myocardium suffers from oxygen deficiency for the following reasons:
- insufficient oxygen concentration in the environment - occurs in a stuffy room, in a smoky environment, in mountainous areas, in scuba cylinders during underwater travel;
- impaired adaptive reaction - in stressful situations, increased physical activity, the heart requires more oxygen;
- disruption of the proper functioning of the respiratory system - bronchospasm, insufficient area of lung tissue to exchange carbon dioxide for oxygen (with bronchial asthma, emphysema, pneumonia, pulmonary artery thrombosis, respiratory tuberculosis);
- disturbances in the number of red blood cells, a decrease in hemoglobin levels leads to a decrease in the binding of oxygen molecules and its delivery (anemia, severe stage of erythremia, leukemia);
- the effect of poisons, intoxication - cause blocking of enzymes involved in the processes of assimilation of energy-producing substances;
- circulatory hypoxia - for diseases of the heart and blood vessels that cause a decrease in systolic blood output due to myocardial weakness (acute infarction, cardiopathy, ischemia, heart failure due to defects).
X-ray of the lungs of a patient with tuberculosis: dark spots on the left and right indicate the absence of normal lung tissue
In most cases, patients have a mixed form; 2 or more factors are involved in the disease.
In the occurrence of myocardial hypoxia, the main “culprit” is most often a disruption of the neurohumoral regulation of cardiac activity. Changes in the medulla oblongata or hypothalamus, where the control centers of the cardiovascular system are located, should compensate for the needs of the heart muscle. Violation of this connection is fraught with manifestations of energy hunger.
Types of hypoxia
Hypoxia, depending on the mechanism of development, is divided into:
- Exogenous hypoxia (hypoxic hypoxia) is caused by environmental factors.
- Endogenous hypoxia is caused by various diseases or disorders that a person has:
- Respiratory (respiratory, pulmonary) hypoxia.
- Circulatory (cardiovascular) hypoxia: Ischemic; Stagnant.
- Hemic (blood) hypoxia: Anemic; Caused by inactivation of hemoglobin.
- Tissue (histotoxic) hypoxia. Substrate hypoxia.
- Overload hypoxia. Mixed hypoxia.
Depending on the speed of development and course:
- Lightning fast (instant) – develops within a few seconds (no longer than 2 – 3 minutes);
- Acute – develops within several tens of minutes or hours (no longer than 2 hours);
- Subacute – develops within several hours (no longer than 3-5 hours);
- Chronic – develops and lasts for weeks, months or years.
Depending on the prevalence of oxygen starvation , hypoxia is divided into general and local .
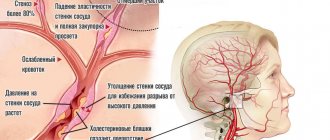
Exogenous hypoxia
Exogenous hypoxia (hypoxic) is caused by a decrease in the amount of oxygen in the inhaled air. Accordingly, blood leaves the lungs that is not sufficiently saturated with oxygen and a small amount of gas is brought to the cells of various organs/tissues. Exogenous hypoxia is manifested by cyanosis (blueness of the skin and mucous membranes), dizziness and fainting.
exogenous hypoxia normobaric
Depending on atmospheric pressure, exogenous hypoxia is divided into hypobaric and normobaric.
Hypobaric hypoxia is caused by low oxygen content in rarefied air with low atmospheric pressure. Such hypoxia develops in mountainous areas and at high altitudes.
Normobaric hypoxia develops when there is a low oxygen content in air with normal atmospheric pressure. Normobaric exogenous hypoxia can develop when being in mines, wells, on submarines, in diving suits, in cramped rooms with large crowds of people, with general air pollution or smog in cities, as well as during surgery if anesthesia-respiratory equipment malfunctions.
Respiratory (respiratory, pulmonary) hypoxia
respiratory hypoxia
Respiratory (respiratory, pulmonary) hypoxia develops in diseases of the respiratory system (bronchitis, pulmonary hypertension, any lung pathologies, etc.), when the penetration of oxygen from the air into the blood is difficult. Against the background of respiratory hypoxia, complications may develop, such as respiratory failure, cerebral edema and gas acidosis.
Circulatory (cardiovascular) hypoxia
circulatory hypoxia
Circulatory (cardiovascular) hypoxia develops against the background of various circulatory disorders (for example, decreased vascular tone, decreased total blood volume after blood loss or dehydration, increased blood viscosity, increased coagulability, centralization of blood circulation, venous stagnation, etc.). If a circulatory disorder affects the entire network of blood vessels, then systemic . If blood circulation is disrupted only in the area of an organ or tissue, then hypoxia is local .
During circulatory hypoxia, a normal amount of oxygen enters the blood through the lungs, but due to circulatory disorders, it is delivered to organs and tissues with a delay, as a result of which oxygen starvation occurs in the latter.
According to the mechanism of development, circulatory hypoxia is ischemic and stagnant. The ischemic form of hypoxia develops with a decrease in the volume of blood passing through organs or tissues per unit of time. This form of hypoxia can occur with left ventricular heart failure, heart attack, cardiosclerosis, shock, collapse, vasoconstriction of some organs and other situations.
The stagnant form of hypoxia develops when the speed of blood movement through the veins decreases - with thrombophlebitis of the legs, right ventricular heart failure, increased intrathoracic pressure and other situations when blood stagnation occurs in the venous bed. In the stagnant form of hypoxia, venous blood does not return to the lungs in time to remove carbon dioxide and saturate with oxygen. As a result, there is a delay in the delivery of the next portion of oxygen to organs and tissues.
Hemic (blood) hypoxia
Hemic (blood) hypoxia develops when quality characteristics are impaired or the amount of hemoglobin in the blood decreases. Hemic hypoxia is divided into two forms - anemic and caused by changes in hemoglobin quality .
hemic hypoxia
Anemic hemic hypoxia is caused by a decrease in the amount of hemoglobin in the blood, that is, anemia of any origin or hydremia (dilution of the blood due to fluid retention in the body). During anemic hypoxia, oxygen is normally bound and transported by the blood to organs and tissues. But due to the fact that there is too little hemoglobin, insufficient oxygen is brought to the tissues and hypoxia occurs in them.
Hypoxia, caused by a change in the quality of hemoglobin, is associated with poisoning by various toxic substances, which lead to the formation of forms of hemoglobin that are not capable of carrying oxygen (methemoglobin or carboxyhemoglobin). When the quality of hemoglobin changes, its quantity remains normal, but it loses its ability to carry oxygen. As a result, when passing through the lungs, hemoglobin is not saturated with oxygen and the blood flow does not deliver it to the cells of all organs and tissues. A change in the quality of hemoglobin occurs when poisoned by a number of chemicals, such as carbon monoxide (carbon monoxide), sulfur, nitrites, nitrates, etc.
Tissue (histotoxic) hypoxia
Tissue (histotoxic) hypoxia develops against the background of impaired ability of organ cells to absorb oxygen. The cause of tissue hypoxia is reduced activity or deficiency of mitochondrial respiratory chain enzymes, which convert oxygen into forms in which it is used by cells to carry out all life processes.
Disruption of respiratory chain enzymes can occur in the following cases:
- Suppression of the activity of respiratory chain enzymes in case of poisoning with cyanide, ether, urethane, barbiturates and alcohol;
- Lack of enzymes of the respiratory chain due to deficiency of vitamins B1, B2, PP and B5;
- Disruption of the enzymes of the respiratory chain due to poisoning with nitrates, microbial toxins, exposure to large amounts of thyroid hormones, etc.;
- Damage to the structure of enzymes due to exposure to radioactive radiation, uremia, cachexia, severe infectious diseases, etc.
Tissue hypoxia can exist for a long period of time.
Substrate hypoxia
substrate hypoxia
Substrate hypoxia develops with normal oxygen delivery to tissues, but in conditions of a lack of basic nutrients that undergo oxygen oxidation. Substrate hypoxia can develop during fasting, diabetes and other conditions when there is not enough glucose and fatty acids in the cells.
Overload hypoxia
overload hypoxia
Overload hypoxia can develop during heavy physical work, when cells intensively consume oxygen. In such cases, the cells simply do not have enough oxygen delivered. Such physiological hypoxia is not dangerous and goes away after completing the stage of high physical activity.
Mixed hypoxia
Mixed hypoxia is a combination of several types of endogenous hypoxia and occurs with severe, life-threatening lesions of various organs and systems, such as shock, poisoning, coma, etc.
Acute hypoxia
Acute hypoxia develops quickly, within several tens of minutes, and persists for a limited period of time, ending either with the elimination of oxygen starvation, or with irreversible changes in organs that will lead to severe illness or even death. Acute hypoxia usually accompanies acute conditions in which blood flow, quantity and quality of hemoglobin sharply change, such as, for example, blood loss, cyanide poisoning, heart attack, etc.
acute hypoxia
Any variant of acute hypoxia must be eliminated as soon as possible, since the body will be able to maintain the normal functioning of organs and tissues for a limited period of time until compensatory and adaptive reactions are exhausted. And when the compensatory-adaptive reactions are completely exhausted, the most important organs and tissues (primarily the brain and heart) will begin to die under the influence of hypoxia.
In principle, acute hypoxia is more dangerous than chronic hypoxia, since it can quickly lead to disability, organ failure or death. And chronic hypoxia can exist for years, giving the body the opportunity to adapt and live and function quite normally.
Chronic hypoxia
chronic hypoxia
Chronic hypoxia develops over several days, weeks, months or even years, and occurs with long-term diseases. The body adapts to chronic hypoxia by changing the structure of cells to new conditions, which allows organs to function quite normally. In principle, chronic hypoxia is safer than acute hypoxia, because develops slowly and the body is able to adapt to new conditions using compensation mechanisms.
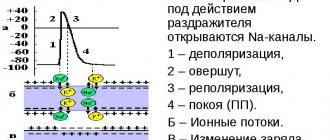
Pathogenetic therapy of hypoxia conditions of organs and tissues at the cellular level
Cytochrome C is a mitochondrial protein with a molecular weight of 12,500 Da, containing an iron atom as part of the prosthetic group, capable of transitioning from divalent to trivalent and back, participating in the transfer of electrons between the complexes of coenzyme Q - cytochrome C - reductase and cytochrome C - oxidases, not binding oxygen and participating in tissue respiration [7, 29]. The molecule is folded into a compact globule, in which most hydrophilic groups are located on the outside and hydrophobic groups on the inside (Fig. 1) [3].
The raw material for the manufacture of the drug cytochrome C is usually obtained from the hearts of cattle, but it can also be obtained from salmon fish, such as chum salmon [3]. The chemical synthesis of cytochrome C and its modified analogues has also been described [35].
The main pharmacological effect of exogenously administered cytochrome C is considered to be antihypoxic. This drug, in essence, performs the function of replacement therapy, since during hypoxia, due to structural disorders, mitochondria lose some of their components, including electron carriers. Experimental studies have proven that exogenous cytochrome C, during hypoxic damage to cell membranes and mitochondria, is able to penetrate through them and integrate into the respiratory chain, contributing to the restoration of energy-producing oxidative phosphorylation (Fig. 2).
The antihypoxic effect of cytochrome C increases significantly when the drug is placed in liposomes, which provide better penetration through membranes [11, 25]. The liposomal form of cytochrome C (in complex with phosphatidylethanolamine) was first obtained by Scaife and Hill in 1963 [33].
Cytochrome C may be a useful means of combination therapy for various diseases in the pathogenesis of which hypoxic damage is important.
Cardiovascular diseases
A fairly large number of studies have been devoted to studying the effectiveness and safety of cytochrome C in acute coronary syndrome. The prerequisites for clinical testing of the drug were preclinical studies, where experimental models of myocardial infarction showed an increase in the contractile and pumping functions of the myocardium [5].
In a study by K. Yu. Yuldashev et al., conducted in 1990 on 25 patients (36–71 years old) with myocardial infarction, 11 patients received traditional therapy, and 14 received additional cytochrome C 5 mg 3 times a day for weeks. A beneficial effect of the drug on the functional state of the myocardium and its contractile function, as well as systemic hemodynamics, was noted [31].
M. M. Agaev describes a study of the effectiveness of cytochrome C in the complex therapy of 42 patients aged 30 to 70 years with anterior myocardial infarction with a Q wave. The patients were divided equally into two groups. In group 1 (mean age 57.8 ± 2.1 years) fosinopril with propranolol was used, in group 2 (mean age 56.9 ± 2.3 years) fosinopril with cytochrome C was used. In group 2, observed faster stabilization of blood pressure, decrease in end-systolic and diastolic volumes, increase in left ventricular ejection fraction. In the same group, heart failure developed less frequently [1].
The effect of cytochrome C on systemic hemodynamics was studied in a clinical study by G. A. Boyarinov. Clinical studies were conducted on 52 patients with acute infective endocarditis and heart valve disease requiring surgery under cardiopulmonary bypass. The patients were divided equally, with the first group using pharmacocold cardioplegia, and the second group receiving an intravenous bolus of cytochrome C at a dose of 0.5 mg/kg 10 minutes before opening the aorta as a cardioprotector. The use of cytochrome C ensured rapid restoration of cardiac blood flow and systemic hemodynamics, and prevented the activation of lipid peroxidation. Against the background of a slight positive inotropic effect, there was a decrease in afterload, restoration of the bioelectrical and pumping function of the myocardium, and a decrease in postoperative hospital mortality from acute heart failure [5].
A study of the effectiveness of cytochrome C in the combination of coronary artery disease (CHD) and chronic heart failure (CHF) was conducted in 2010–2013. on the basis of the cardiology department of the St. Petersburg Clinical Hospital of the Russian Academy of Sciences. The study included 60 patients (52–87 years old) with IHD complicated by arrhythmias and/or CHF. The patients were divided into two groups, one of which received 20 mg of cytochrome C per day intravenously for 10 days, and the second received potassium chloride and magnesium sulfate. The use of the study drug turned out to be effective in the treatment of patients with coronary artery disease complicated by arrhythmias and/or FC I–II CHF (NYHA) - in this case, improvements in clinical symptoms, exercise tolerance (6-minute walk test), and quality of life indicators were observed. At the same time, the proBNP level decreased and there was a tendency to decrease the number of ventricular extrasystoles and the incidence of ischemic changes in the myocardium [23].
A comparative study of the effectiveness of cytochrome C and ethylmethylhydroxypyridine succinate in the complex treatment of 87 patients with coronary artery disease (average age 73.9 years), complicated by CHF and/or arrhythmias, demonstrated a greater increase in exercise tolerance and a significant decrease in the frequency of ventricular extrasystoles in the group receiving cytochrome C [4, 29].
The data obtained on the effectiveness of cytochrome C in the combination of IHD and CHF do not contradict the trend towards expanding the use of antihypoxants in this pathology [6, 15].
Cerebrovascular disorders
In chronic experiments on rabbits with microelectrodes implanted into the cerebral cortex, thalamus and hypothalamus to record local blood flow, reactions of cerebral vessels, oxygen tension and the water-electrolyte state of brain tissue, I. V. Polevik showed that during hypoxic effects on the brain, prophylactic administration of cytochrome C at a dose of 0.3 mg/kg has a cerebroprotective effect, preventing or reducing pathological changes that develop without the use of the drug. The effect of the drug was characterized by a decrease in the severity of hypoxia in the cerebral cortex and prevention or weakening of the development of intracellular and extracellular edema of brain tissue [20].
A number of authors are considering the possibility of using cytochrome C as an auxiliary drug for cardioembolic stroke (4–8 ml of 0.25% lyophilisate intramuscularly or 200 ml of isotonic sodium chloride solution intravenously drip) or a neuroprotective agent after an ischemic stroke (0.25–0.5 mg/kg per day) [12, 28].
Liver lesions
Using models of acute and chronic intoxication with carbon tetrachloride, it was shown that parenteral administration of cytochrome C increases the concentration of exogenous cytochrome C in the liver and activates the processes of oxidative phosphorylation while simultaneously increasing the ATP content, reducing ADP and AMP, and increasing the energy charge of the adenine nucleotide system [24].
The most interesting results are the use of cytochrome C for toxic liver damage. Thus, intravenous administration of the drug (20 mg per day for 15 days) in complex therapy of 18 patients aged 32 to 60 years with chronic hepatitis due to alcohol abuse allowed achieving rapid clinical and laboratory remission with good tolerability of the drug [10]. Also, a pronounced positive effect of the use of cytochrome C (20 mg/day intravenously for 15–20 days) in the form of a decrease in total bilirubin and a decrease in the manifestations of edematous-ascitic syndrome was detected in toxic alcoholic hepatitis and cirrhosis of the liver. The study included 68 patients with hepatitis of various etiologies, including 47 in the cirrhotic stage [18].
Intoxication
Cytochrome C is traditionally considered as a means of complex therapy for various intoxications. The drug was first used as a detoxifier in 1953 to treat a patient with cyclobarbital poisoning. After two injections of 30 mg of cytochrome C, the patient, who had been in a comatose state for 59 hours, regained consciousness, reflexes were restored, cyanosis disappeared, and after the third injection, complete recovery occurred [34].
The effectiveness of the drug in traumatic toxicosis and poisoning with sleeping pills and narcotic drugs, combustion products, carbon monoxide and other toxicants has been shown [13].
Yu. A. Atsybushev conducted a study in which a group of 22 patients with acute intoxication with alcohol and drugs in a coma received cytochrome C by injection. After 1–2 injections, patients emerged from a comatose state, and the time of stay in the ICU was reduced by 3–5 days [14].
Fetal hypoxia, hypoxia and asphyxia of newborns
In 1973, A. Ya. Polyak published an article reporting intravenous administration of cytochrome C at a dose of 0.5 mg/kg to women in labor for the prevention and treatment of intrauterine fetal hypoxia. The study included 27 women who received the drug before and during childbirth. Improvement in fetal cardiac activity occurred within an hour after administration, which the author associated with improved function of the placenta, which loses cytochrome C under hypoxia, and a direct effect on the fetal cardiovascular system [21].
A fairly large study was conducted at the VMA named after. S. M. Kirov in the clinic of obstetrics and gynecology. The effect of cytochrome C on the state of cardiac activity was assessed in 196 newborns, among whom 18 had severe asphyxia, 60 had mild asphyxia and 118 without asphyxia. The drug was injected into the umbilical vein of the newborn during the first two minutes after birth at a dose of 10 mg. The administration of cytochrome C contributed to a decrease in the duration of the cardiac cycle, especially in severe asphyxia, a reduction in mechanical and total systole and a change in the total systole/diastole ratio. In cases of severe asphyxia with intracranial hemorrhage, cytochrome C was not effective [2]. In addition, slow intravenous jet administration of the drug at this dose reduces post-hypoxic brain damage in newborns in the first days of life [30].
In neonatology, to correct hemodynamics in newborns who have suffered hypoxia, cytochrome C is administered intravenously as a pharmacological agent at a dose of 1.25–2.5 mg/kg daily during the first days of life after birth [22]. For transient disorders of the cardiovascular system in newborns, the drug is used at a dose of 2.5 mg/kg 1 time/day for a course of 4 days [27], and in the presence of connective tissue dysplasia of the heart in children and adolescents, cytochrome C can be administered intramuscularly at a dose of 15 mg 2–4 courses of 10 injections per year [17].
In addition, cytochrome C can be used to compensate for energy deficiency in muscle tissue in the complex therapy of muscle hypotension syndrome in newborns and young children [9].
Eye diseases
A study of the therapeutic effectiveness of 0.25% cytochrome C eye drops in 42 patients (18–45 years old) with corneal opacification after keratitis demonstrated an increase in visual acuity due to a decrease in corneal opacification and an improvement in the condition of its epithelium during drug therapy with good tolerability and the absence of unwanted drugs reactions [26].
In patients with various diseases of the retina, including degenerative processes of the macular region, intravenous administration of cytochrome C at a dose of 10 mg/day for 10–14 days made it possible to achieve an increase in visual acuity by 0.2–0.4 units and expand the fields vision [2].
Fertility disorders
In 1990, M.I. Kramar and the doctors of Kharkov Maternity Hospital No. 5 managed to demonstrate an increase in sperm fertility, increase their survival by more than 30% by adding cytochrome C to the seminal fluid in a dose of 1 µmol, which contributed to an increase in the pregnancy rate during in vitro fertilization [ 8]. Also, in idiopathic pathozoospermia, the use of cytochrome C contributed to an increase in the concentration, motility and content of normal forms of sperm in the ejaculate [16].
The main indications for use and dosage regimens for cytochrome C are presented in Table.
Thus, the use of cytochrome C has quite broad prospects, since it affects the energy of the cell, which determines all other functions. Its use in cases where a hypoxic component is present in the pathogenesis of the disease can prevent the development of irreversible changes in organs. Rational treatment regimens using cytochrome C should be based on the results of controlled clinical trials and economic feasibility.
Literature
- Agaev M. M. Efficacy of angiotensin-converting enzyme inhibitors, β-blocker and antihypoxant in the phase of inpatient rehabilitation of myocardial infarction in patients working in environmentally unfavorable conditions // Clinical Medicine. 2010. No. 1. P. 58–62.
- Andriyanova I.G., Sidorova N.D., Selivanov E.A. Results of clinical use of the drug cytochrome C // Polyclinic. 2011. No. 1. pp. 39–41.
- Ayushin N. B., Kovalev N. N. Cytochrome C from salmon hearts: methods of production and properties // Izvestia TINRO. 2006. T. 146. pp. 288–293.
- Balluzek M.F., Semenova I.G. Rational choice of therapy with drugs of metabolic groups for coronary heart disease // Practical Medicine. 2013. No. 3 (73). pp. 47–51.
- Boyarinov G. A., Yakovlev A. Yu., Tezyaeva S. A., Mukhina I. V., Boyarinova L. V. Use of cytochrome C for the prevention of myocardial reperfusion damage during heart valve replacement under artificial circulation // Bulletin of Surgery. 2001. No. 1. P. 15–20.
- Vasyuk Yu. A., Shkolnik E. L., Kulikov K. G., et al. The effect of Preductal MV therapy on the course of CHF in patients with stable angina pectoris who have suffered acute myocardial infarction. Results of the PRIMA study // Heart failure. 2009. T. 10, No. 1. P. 34–36.
- Vashchenko V.I., Hanson K.P., Shabanov P.D. Cytochrome C as a medicine: past, present, future // Review. Wedge. Pharmacol. lek. ter. 2005. T. 4, No. 1. P. 27–37.
- Grishchenko V. I., Alekseevskaya E. I., Kramar M. I. A method for increasing the viability of chilled human sperm. Patent No. 38000 A Ukraine. 2001. Bulletin. No. 4.
- Evtushenko S.K., Morozova T.M., Shaimurzin M.R. Muscular hypotension syndrome in newborns and young children // News of medicine and pharmacy. 2011. No. 4 (384). pp. 50–63.
- Clinical use of the drug “Cytochrome C” in patients with chronic hepatitis in combination with toxic liver damage // Polyclinic. 2009. No. 5. P. 48.
- Krivoruchko B. I., Kashina E. A., Zarubina I. V. et al. Antihypoxants and actoprotectors: Results and prospects. St. Petersburg, 1994. Issue. 1. P. 52.
- Kutashov V. A., Skorokhodov A. P., Khakhanova O. N. On the issue of treatment of cardioembolic strokes in the acute period // Central Scientific Bulletin. 2021. Vol. 1, No. 14. pp. 33–40.
- Levchenkova O. S., Novikov V. E., Pozhilova E. V. Pharmacodynamics and clinical use of antihypoxants // Reviews on clinical pharmacology and drug therapy. 2012. T. 10, No. 3. P. 3–12.
- Loginov S.I., Oboznaya E.I. Method of treating exotic lumps. Patent No. 1822761. 1993. Bulletin. No. 21.
- Mareev V. Yu., Minina Yu. V., Begrambekova Yu. L. Kudesan® (drops 3% for oral administration) in the treatment of patients with heart failure: effectiveness and safety in combination with standard therapy (Kudesnik). Design and results of a prospective, randomized, double-blind study of Magician // Heart failure. 2021. Vol. 17, No. 4. pp. 236–249.
- Mikhailichenko V.V., Fesenko V.N., Novikov A.I., Fesenko S.V. Efficacy of cytochrome C in the correction of pathozoospermia // Terra Medica. 2012. No. 3. pp. 17–20.
- Nishchaeva N. F., Barkun G. K., Lysenko I. M., Zhuravleva L. N., Ivanova L. G. Diagnosis and treatment of minor cardiac anomalies in children and adolescents / Achievements of fundamental, clinical medicine and pharmacy. Materials of the 71st scientific session of university staff. Vitebsk State Medical University, 2021. pp. 197–198.
- Nosikova E.V., Ivanova S.V. Results of using the drug “Cytochrome C” in patients with chronic hepatitis of various etiologies // Remedium Privolzhye. 2010. No. 6.
- Okovityy S.V. Clinical pharmacology of antihypoxants. FARMIndex-Practician, 2005. Vol. 7. pp. 48–63.
- Polevik I. B. Assessment of the cerebroprotective effects of cytochrome c on the mind of hypoxia, which occurs during the modeling of space sickness of the roc // Theoretical Medicine. 2010. T. XV, No. 1. P. 10–14.
- Polyak A. Ya. Use of cytochrome C for the prevention and treatment of intrauterine fetal hypoxia. In the book: Physiology and pathology of pregnancy and children. L.: B.I., 1973. pp. 136–140.
- Prakhov A.V., Shilenok I.G. A method for correcting hemodynamics in newborns who have suffered hypoxia. Patent 2067454 dated 10.10.1996.
- Semenova I. G., Ballyuzek M. F., Novikov Yu. A., Tugusheva F. A. Efficiency of treatment of patients with chronic heart failure and cardiac arrhythmias with the drug cytochrome C // Farmateka. 2013. No. 10. pp. 91–96.
- Smirnov A.V., Krivoruchko B.I. Antihypoxants in emergency medicine // Anesthesiology and Reanimatology. 2008. No. 2. P. 50–55.
- Smirnov A.V., Krivoruchko B.I., Zarubina I.V. et al. Current problems in the creation of new drugs. St. Petersburg, 1996. pp. 163–164.
- Sokolov V. O., Morozova N. V., Florentseva S. S., Veselov A. V., Morozov M. A. Evaluation of the effect of the drug “Cytochrome C” on the restoration of visual functions in patients with corneal opacities after keratitis // Ophthalmological statements. 2021. Vol. 10. No. 2. pp. 79–86.
- Sukalo A.V., Tkachenko A.K., Khrustaleva E.K., Chichko A.M., Marochkina E.M. Transient disorders of the cardiovascular system in newborns // Journal of the Grodno State Medical University. 2015. No. 3. P. 5–11.
- Usenko L.V., Maltseva L.A., Tsarev A.V. Ischemic stroke from the perspective of a resuscitator: modern approaches to intensive care // General resuscitation. 2005. No. 1. P. 60–70.
- Cheltsov V.V., Martynov A.I., Gushchina Yu.Sh., Illarionova T.S., Korovyakova E.A. Metabolic therapy for chronic heart failure // Therapy. 2021. Vol. 4, No. 8. pp. 54–60.
- Shabalov N.P. Yaroslavsky V.K. Khodov D.A. Lyubimenko V.A. Asphyxia of newborns. L.: Medicine, 1990. pp. 170–171.
- Yuldashev K. Yu., Samandrov M. Ya., Velizade E. M. Effect of cytochrome C on central hemodynamic parameters in acute myocardial infarction // Polyclinic. 2010. No. 2. P. 57–58.
- Bai YW, Sosnick TR, Mayne L., Englander SW Protein folding intermediates: Native-state hydrogen exchange // Science. 1995. Vol. 269. P. 192–197.
- Scaife JF, Hill B. The uncoupling of oxidative phosphorylation by ionizing radiation // Can J Biochem Physiol. 1962. Vol. 40. P. 1025–1042.
- Van Bekkum DW Oxidative phosphorilation in some radiosensitive tissues after irradiation // Ciba Pound. Symp. Jonizing Radiation Cell Metab. 1965. P. 77–89.
- Wallace CJA, Mascagnill P., Chait BT, Collawn JF, Patersons Y., Proudfoot AEI, Kent SBH Substitutions engineered by chemical synthesis at three conserved sites in mitochondrial cytochrome C // The journal of biological chemistry. 1989. Vol. 264, No. 26. P. 15199–15209.
D. Yu. Ivkin, Candidate of Biological Sciences S. V. Okovity1, Doctor of Medical Sciences, Professor
FSBEI HE SPHFA Ministry of Health of the Russian Federation, St. Petersburg
1 Contact information
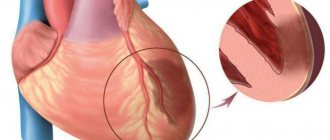
Myocardial hypoxia
myocardial hypoxia
Myocardial hypoxia is one of the most dangerous diseases and is characterized by insufficient oxygen supply to the heart muscle.
This condition occurs when there is a sudden decrease in oxygen supply to the heart muscle. Cells do not have time to adapt to changed conditions. Metabolism continues in them, but it becomes incomplete, and under-oxidized metabolites accumulate. If hypoxia persists, cardiac muscle tissue dies.
Clinically, this condition is manifested by attacks of chest pain, increasing their duration and intensity. Subsequently, myocardial infarction develops - necrosis of the heart muscle with loss of its contractile function.
Myocardial hypoxia can be caused by the following reasons:
- low oxygen content in atmospheric air;
- diseases of the lungs with impaired gas exchange in them;
- decrease in the amount of blood flowing through the myocardium due to pathology of the coronary arteries;
- deterioration of the blood's ability to carry oxygen, for example, with carbon monoxide poisoning;
- disruption of oxygen utilization by the cells themselves, for example, in case of poisoning with cyanides and heavy metals.
Treatment with medications
Hypoxia is treated using medications from various groups:
- Analgesics. You can use any medications, but only after consulting a doctor. Usually pain is relieved with Akamol, Pentalgin, Bupranal or Anopyrine.
- Antidotes. Designed to get rid of hypoxia that occurs after poisoning. When intoxicating the body, medicinal drugs are used: “Flumazenil”, mushrooms – “Diazepam” or “Atropine”, heavy metals – “Cuprenil” or “Unithiol”, organic acids – “Almagel”, carbon monoxide – glucose.
- Dilatating bronchi. Most often it is recommended to use Truvent, Berodual, Atrovent and Salbumatol.
- Antispasmodics. The drugs are used if a stroke condition occurs as a result of the disease.
- Vitamins. In case of poisoning, the patient is prescribed K1, C and B6. The multivitamin complex is recommended for patients with any form of the disease.
Consequences of hypoxia
The consequences of hypoxia can be different and depend on the period of time during which oxygen starvation was eliminated and how long it lasted. If hypoxia was eliminated during a period when the compensatory mechanisms were not exhausted, then there will be no negative consequences; after some time, the organs and tissues will completely return to their normal mode of operation. But if hypoxia was eliminated during the period of decompensation, when compensatory mechanisms were exhausted, then the consequences depend on the duration of oxygen starvation. The longer the period of hypoxia against the background of decompensation of adaptive mechanisms, the stronger and deeper the damage to various organs and systems. Moreover, the longer hypoxia lasts, the more organs are damaged.
During hypoxia, the brain suffers the most, since it can withstand without oxygen for 3-4 minutes, and from the 5th minute necrosis will begin to form in the tissues. The heart muscle, kidneys and liver are able to tolerate a period of complete absence of oxygen for 30-40 minutes.
The consequences of hypoxia are always due to the fact that in cells, in the absence of oxygen, the process of oxygen-free oxidation of fats and glucose begins, which leads to the formation of lactic acid and other toxic metabolic products that accumulate and ultimately damage the cell membrane, leading to its death. When hypoxia lasts long enough from the toxic products of improper metabolism, a large number of cells in various organs die, forming entire areas of dead tissue. Such areas sharply worsen the functioning of the organ, which is manifested by corresponding symptoms, and in the future, even with the restoration of oxygen flow, will lead to a persistent deterioration in the functioning of the affected tissues.
The main consequences of hypoxia are always caused by disruption of the central nervous system, since it is the brain that suffers primarily from oxygen deficiency. Therefore, the consequences of hypoxia are often expressed in the development of a neuropsychiatric syndrome, including parkinsonism, psychosis and dementia. In 50-70% of cases, neuropsychiatric syndrome can be cured. In addition, a consequence of hypoxia is exercise intolerance, when with minimal exertion a person experiences palpitations, shortness of breath, weakness, headache, dizziness and pain in the heart area. Also, the consequences of hypoxia can be hemorrhages in various organs and fatty degeneration of muscle, myocardial and liver cells, which will lead to disruptions in their functioning with clinical symptoms of failure of one or another organ, which can no longer be eliminated in the future.
Folk remedies
Photo: xcook.info
There are no traditional medicines that can relieve a person from hypoxia. To begin treatment measures, it is necessary to establish the cause that caused oxygen starvation. Treatment of hypoxia is carried out exclusively by a qualified doctor, who preliminarily prescribes a range of necessary studies. That is why, when the first symptoms appear, you should immediately seek help from a medical facility. Self-medication at home is strictly prohibited, since these actions can lead to aggravation of the pathological process. In addition, it is important to remember that early access to a medical facility is the basis for a successful treatment outcome.
As you know, there are various oxygen cocktails, which, according to manufacturers, are capable of enriching organs and tissues with oxygen. However, there is no clinical evidence or medical evidence to support this theory. Many will ask why the benefits of oxygen products have not been proven. In fact, everything is simple: oxygen is absorbed exclusively in the lungs; the body cannot receive oxygen through the stomach and intestines.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Hypoxia - causes
The causes of exogenous hypoxia may be the following factors:
- Thin atmosphere at altitude (mountain sickness, altitude sickness, pilot sickness);
- Being in tight spaces with large crowds of people;
- Being in mines, wells or in any enclosed spaces (for example, submarines, etc.) with no communication with the outside environment;
- Poor ventilation of premises;
- Working in diving suits or breathing through a gas mask;
- Severe air pollution or smog in the city of residence;
- Malfunction of anesthesia-respiratory equipment.
The causes of various types of endogenous hypoxia may be the following factors:
- Respiratory diseases (pneumonia, pneumothorax, hydrothorax, hemothorax, destruction of alveolar surfactant, pulmonary edema, pulmonary embolism, tracheitis, bronchitis, emphysema, sarcoidosis, asbestosis, bronchospasm, etc.);
- Foreign bodies in the bronchi (for example, accidental swallowing of various objects by children, choking, etc.);
- Asphyxia of any origin (for example, due to compression of the neck, etc.);
- Congenital and acquired heart defects (non-closure of the foramen ovale or the duct of Batal, rheumatism, etc.);
- Damage to the respiratory center of the central nervous system due to injuries, tumors and other diseases of the brain, as well as when it is suppressed by toxic substances;
- Impaired breathing mechanics due to fractures and displacements of the chest bones, damage to the diaphragm or muscle spasms;
- Cardiac dysfunction caused by various heart diseases and pathologies (heart attack, cardiosclerosis, heart failure, electrolyte imbalance, cardiac tamponade, pericardial obliteration, blockade of electrical impulses in the heart, etc.);
- A sharp narrowing of blood vessels in various organs;
- Arteriovenous shunting (transfer of arterial blood into veins through vascular shunts before it reaches organs and tissues and releases oxygen to cells);
- Stagnation of blood in the inferior or superior vena cava system;
- Thrombosis;
- Poisoning with chemicals that cause the formation of inactive hemoglobin (for example, cyanide, carbon monoxide, lewisite, etc.);
- Anemia;
- Acute blood loss;
- Disseminated intravascular coagulation syndrome (DIC syndrome);
- Impaired metabolism of carbohydrates and fats (for example, diabetes, obesity, etc.);
- Shock and coma;
- Excessive physical activity;
- Malignant tumors of any location;
- Chronic kidney and blood diseases (for example, leukemia, anemia, etc.);
- Deficiency of vitamins PP, B1, B2 and B5;
- Thyroid diseases;
- Damage to cells by radiation, tissue breakdown products due to cachexia, severe infections or uremia;
- Drug and alcohol abuse;
- Prolonged fasting.
Classification of hypoxia
According to genesis, four types of hypoxia are distinguished:
- respiratory, which occurs when ventilation of the lungs and gas exchange at the level of the alveolo-capillary membrane are impaired
- circulatory, which occurs when blood flow, microcirculation and gas exchange at the blood-tissue level are disrupted
- hemic, caused by impaired delivery of oxygen to tissues due to anemia or hemoglobin binding; this happens with cyanide or CO poisoning
- combined genesis (the above 3 components are combined)
It is also relevant to divide hypoxia by duration and development into the following forms:
- lightning fast
- subacute
- chronic
Symptoms (signs) of hypoxia
symptoms of hypoxia
In the fulminant form of hypoxia, clinical symptoms do not have time to appear, since death occurs within a very short period of time (up to 2 minutes).
The acute form of hypoxia lasts up to 2-3 hours, and during this period there is a failure of all organs and systems at once, primarily the central nervous system, respiration and heart (heart rate becomes less frequent, blood pressure drops, breathing becomes irregular, etc.). If hypoxia is not eliminated during this period, then organ failure progresses to coma and agony, followed by death.
Subacute and chronic forms of hypoxia are manifested by the so-called hypoxic syndrome. Against the background of hypoxic syndrome, symptoms from the central nervous system first appear, since the brain is most sensitive to oxygen deficiency, as a result of which foci of necrosis (dead areas), hemorrhages and other types of cell destruction quickly appear in its tissues. Due to necrosis, hemorrhage and death of brain cells against the background of oxygen deficiency at the initial stage of hypoxia, a person develops euphoria, he is in an excited state, and he is tormented by motor restlessness. One's own condition is not assessed critically.
With further progression of hypoxia, the following signs of depression of the cerebral cortex appear, which are similar in manifestations to alcohol intoxication:
- Drowsiness;
- Lethargy;
- Headache and dizziness;
- Noise in ears;
- Lethargy;
- Impaired consciousness;
- Involuntary passage of urine and feces;
- Nausea and vomiting;
- Movement coordination disorder;
- Cramps.
Convulsions during hypoxia appear when exposed to external stimuli. Moreover, a convulsive attack usually begins with twitching of the muscles of the face, hands and feet with the addition of random muscle contractions of the abdomen. Sometimes during convulsions opisthotonus , which represents a person arched with straightened neck and back muscles, head thrown back and arms bent at the elbows. The posture of a person in opisthotonus resembles the gymnastic figure “bridge”.
In addition to symptoms of depression of the cerebral cortex, a person also experiences pain in the heart area, irregular breathing, shortness of breath, a sharp decrease in vascular tone, tachycardia (an increase in heart rate of more than 70 beats per minute), a drop in blood pressure, cyanosis (blueness of the skin), decrease in body temperature. But when poisoned with substances that inactivate hemoglobin (for example, cyanides, nitrites, nitrates, carbon monoxide, etc.), human skin becomes pinkish in color.
With prolonged hypoxia with the slow development of damage to the central nervous system, a person may develop mental disorders in the form of delirium (“delirium tremens”), Korsakov’s syndrome (loss of orientation, amnesia, replacement of real events by fictitious events, etc.) and dementia.
With further progression of hypoxia, blood pressure drops to 20-40 mmHg. Art. and a coma occurs with loss of brain function. If blood pressure drops below 20 mmHg. Art., then death occurs. In the period before death, a person may experience agonizing breathing in the form of rare convulsive attempts to breathe.
How to saturate the myocardium with oxygen
Chronic patients are advised to spend more time in the fresh air. Walking in parks and squares allows you to breathe cleaner air and increase lung ventilation.
In case of exacerbation, it is recommended to limit motor activity.
In the diet, it is necessary to exclude foods that require oxidation and are difficult to digest (meat, fried and smoked foods, any fats). It is recommended to predominantly eat vegetable dishes and increase the proportion of salads and fresh fruits in the diet. Beets, carrots, dill, onions, and garlic are antihypoxic agents.
Medicines that increase myocardial resistance to oxygen deficiency are called antihypoxants. They are divided into 3 groups:
- having a wide spectrum of action (direct);
- indirect influence;
- mixed.
Group 1
Direct-acting antihypoxants stimulate energy processes in the tissues of the heart muscle due to:
- restoring aerobic and enhancing anaerobic methods of obtaining energy through activation of the respiratory enzymes cytochrome C, ubiquinone;
- disposal of accumulated waste and acid residues;
- reducing the impact of free oxidizing radicals;
- protection of coronary vessels;
- relieving myocardial ischemia;
- existing antiarrhythmic properties;
- restoration of connections with the centers of the brain.
The group includes the following drugs:
- Mildronate,
- Mexidol,
- Actovegin,
- sodium hydroxybutyrate,
- Betimil,
- Neoton,
- Piracetam,
- Preductal,
- Cytomac.
They are used in the treatment of myocardial hypoxia in hospital and outpatient settings. Prescribed by injection in courses with a transition to a tablet maintenance dosage. Especially indicated for acute forms of hypoxia. Equated to first aid.
Group 2
With indirect exposure, the effect is ensured by transferring the heart to a lower level of oxygen consumption. The drugs simultaneously reduce all metabolic processes. They are needed in a short-term emergency to increase tissue survival. Long-term administration is impossible, since the mental functioning of the brain will decrease.
The following have a similar effect:
- sedatives and sleeping pills;
- drugs used for general anesthesia;
- some calcium channel blockers;
- part of α-blockers.
These remedies allow you to survive a difficult period, stimulate adaptive processes in the heart, but do not provide sustainable adaptation to stress.
Group 3
Mixed-action drugs have the properties of both previous groups. These include medicines developed and obtained from plants in combination with vitamin complexes (vitamins E, A, group B, D, C) and microelements necessary for the myocardium (potassium, magnesium, iron, selenium, chromium and others).
Indicated for chronic hypoxia, especially in the treatment of children and the elderly.
A modern direct-acting agent, used for acute and chronic forms of myocardial and brain hypoxia, not indicated during pregnancy and nursing mothers
Degrees of hypoxia
Depending on the severity and severity of oxygen deficiency, the following degrees of hypoxia are distinguished:
- Mild (usually detected only during physical activity);
- Moderate (phenomena of hypoxic syndrome appear at rest);
- Severe (the symptoms of hypoxic syndrome are strongly expressed and there is a tendency to transition to a coma);
- Critical (hypoxic syndrome has led to coma or shock, which can result in agony and death).
Features of chronic hypoxia
The chronic form of myocardial oxygen deficiency develops gradually and depends on:
- the predominant mechanism of pathology development;
- degree of severity and duration of hypoxia;
- environmental conditions in which the patient lives;
- individual sensitivity of a person to lack of energy.
A person with a well-developed immune system is characterized by a high level of metabolic processes in tissues, so adaptive mechanisms remain and work for a long time.
Treatment of oxygen starvation
In practice, mixed forms of hypoxia usually develop , as a result of which the treatment of oxygen deficiency in all cases should be comprehensive, aimed simultaneously at eliminating the causative factor and maintaining an adequate supply of oxygen to the cells of various organs and tissues.
To maintain a normal level of oxygen supply to cells in any type of hypoxia, hyperbaric oxygenation (HBO) - barotherapy - is used. In barotherapy, pressure chambers are used in which a person is under increased pressure with a high oxygen content. Due to the increased pressure, oxygen is additionally dissolved directly in the blood plasma, without contacting red blood cells, which allows its delivery to organs and tissues in the required quantity, regardless of the activity and functional usefulness of hemoglobin. Thanks to hyperbaric oxygenation, it is possible not only to supply organs with oxygen, but also to dilate the blood vessels of the brain and heart, so that the latter can work at full capacity.
In addition to hyperbaric oxygenation, cardiac drugs and drugs that increase blood pressure are used for circulatory hypoxia. If necessary, a blood transfusion is performed (if blood loss incompatible with life has occurred).
For hemic hypoxia, in addition to hyperbaric oxygenation, the following therapeutic measures are carried out:
- Blood or red blood cell transfusion;
- Introduction of oxygen carriers (Perftoran, etc.);
- Hemosorption and plasmapheresis to remove toxic metabolic products from the blood;
- Introduction of substances capable of performing the functions of enzymes of the respiratory chain (vitamin C, methylene blue, etc.);
- Introduction of glucose as the main substance that provides cells with energy to carry out vital processes;
- Administration of steroid hormones to eliminate severe oxygen starvation of tissues.
Treatment
Photo: neurolikar.com.ua
Therapeutic measures are prescribed depending on the cause of hypoxia, aimed at combating the lack of oxygen and correcting disorders that occur in the hemostatic system.
In some cases, to combat hypoxia, it is enough to walk in the fresh air or ventilate the room in which there is a person suffering from lack of air. However, if hypoxia is associated with diseases of the lungs or cardiovascular system, more serious measures are required.
If necessary, various oxygen equipment is used, for example, oxygen masks, oxygen pillows or oxygen cartridges. In some cases, a person needs to be connected to a ventilator. The ventilator provides a forced supply of a gas mixture to the lungs, due to which the blood is saturated with oxygen and carbon dioxide is removed from the lungs.
The following medications can be used:
- bronchodilators;
- antihypoxants;
- respiratory analeptics;
- drugs with a cardiotropic effect (for example, cardiac glycosides);
- antiplatelet agents, anticoagulants.
If the cause of hypoxia is poisoning of the body, special antidotes are introduced, the action of which is aimed at weakening or completely stopping the effect of the poison on the human body. The choice of antidote depends on the nature of the action of the substance that caused the poisoning. The effectiveness of application depends on the accuracy of identifying the appropriate antidote and the time of assistance.
In emergency situations, surgical interventions are performed to eliminate acute hypoxia.
Prevention of hypoxia
Effective prevention of hypoxia is to avoid conditions in which the body may experience oxygen starvation. To do this, you need to lead an active lifestyle, be in the fresh air every day, exercise, eat well, and promptly treat existing chronic diseases. When working in an office, you need to periodically ventilate the room (at least 2-3 times during the working day) to saturate the air with oxygen and remove carbon dioxide from it.
prevention of hypoxia in a pressure chamber
It is also recommended to undergo a course of barotherapy (oxygen capsules and pressure chambers) several times a year, which helps reduce cases of oxygen starvation in the body.
Diagnostics
Photo: clinica-blagodat.ru
The simplest way to determine hypoxia is pulse oximetry - a non-invasive method for determining the degree of oxygen saturation in the blood. The research method is based on the use of various properties of oxygenated and deoxygenated hemoglobin. To measure indicators, the sensor is installed on a finger or earlobe. After a few seconds, the result of determining blood oxygen saturation is displayed. Normally, this figure should not be lower than 95%.
The gas composition and acid-base balance of arterial and venous blood are also examined. During the study, the following indicators of the body's homeostasis are determined: partial pressure of oxygen, partial pressure of carbon dioxide, blood pH, state of carbonate and bicarbonate buffer, etc.
Based on these indicators, it is possible to identify oxygen starvation of the body. However, for successful treatment it is important to establish the cause of hypoxia. For this purpose, laboratory blood parameters are additionally studied, instrumental diagnostic methods are used (electrocardiography, chest radiography, ultrasound examination of the heart, abdominal organs, etc.).
How to identify hypoxia: symptoms and diagnosis
The modern level of medicine makes it possible to detect the presence of hypoxia “without delay”, at its earliest stage. There are a number of diagnostic methods for this:
- analysis of the biochemical composition of blood and hormones;
- listening to heart sounds with a stethoscope (detection of bradycardia and tachycardia);
- amnioscopy - analysis of amniotic fluid (a sign of hypoxia - the presence of meconium in its composition);
- ultrasonography;
- cardiotocography;
- ECG;
- Dopplerometry (study of the circulatory system, analysis of blood circulation in all its areas).
What should you pay attention to? Very strong, sharp kicks of the child that cause pain in the mother are an alarming sign. They may be a consequence of the development of hypoxia: these are reflex movements when the child experiences a lack of oxygen and wants to increase the incoming blood flow. The next symptom is the weakening and complete disappearance of tremors.
Important! The child’s activity norm is at least ten movements in 12 hours.
At what point should fetal activity be monitored? Doctors recommend monitoring your sensations, frequency and strength of kicks, starting from the 28th week of pregnancy. However, the risk of developing hypoxia exists from the first weeks, when it is impossible to monitor fetal activity.
If there are risk factors, then obstetrician-gynecologists recommend a set of measures to prevent oxygen deficiency. In addition, the mother needs to eat in a timely and nutritious manner, avoid lack of sleep and overwork, spend more time outdoors, and ensure regular ventilation in the room.
Assessment of the baby's condition using the Apgar scale . At birth, obstetricians evaluate the baby's condition using Apgar scores (named after the author of this technique, Virginia Apgar). This method analyzes five criteria - breathing, skin color, muscle tone, and heart rate. The child's condition is assessed twice - immediately after passing through the birth canal, and five minutes after that.
- Norm (from 8 to 10 points);
- The condition requires control (from 4 to 7 points). Moderate hypoxia is possible, compensation may be required, prognosis is favorable;
- Asphyxia ( from 0 to 3 points). Severe hypoxia, in which the child requires immediate resuscitation measures.
Low scores on this scale are not always given due to hypoxia, but in most cases it is oxygen deficiency that causes the difficult condition of the newborn.
Traditional methods of treating hypoxia
Traditional methods of treatment should be used only in combination with methods prescribed by your doctor. After all, the causes and types of hypoxia can be different, which also affects the means of treatment. Among folk remedies, woodlice and warty birch have been used since ancient times. Many recipes have been developed. One of them is this: pour 1 tablespoon of dried wood lice into a thermos, pour boiling water over it, let it brew for 8-10 hours. You should take the infusion before meals, 3-4 times a day. You need to drink up to 50 grams at a time.
Traditional healers recommend taking warty birch sap in the desired doses and quantities, but up to 1 liter. Before traditional treatment of hypoxia, you need to find out about your own allergies to these herbs. After all, allergic reactions are serious conditions, especially for pregnant women. Keep in mind that taking medicinal herbs during pregnancy can lead to abortion, so you need constant monitoring from your doctor.
Prevention and treatment of fetal hypoxia
In order for your baby to be born without any abnormalities and not be affected by the problem of hypoxia, you should think about whether you lead a healthy lifestyle. A pregnant woman should give up bad habits even at the stage of planning conception. First of all, this applies to alcoholic beverages, even beer, smoking (even hookah and rolled tobacco) and any drugs. A pregnant woman needs to move from the metropolis to a cleaner area as soon as possible. Fresh air will ensure the health of the unborn child. Regular walks in nature should take place without freezing or overheating.
A pregnant woman should undergo regular examinations with a doctor in order to identify a problem in time if it arises. It is important not only to diagnose the condition, but to discover the causes in order to eliminate them. The doctor can prescribe vitamins individually in each specific case.