- What symptoms of a microinfarction do women experience?
- What symptoms of a microinfarction do men experience?
- General signs of microinfarction
- Causes
- What complications does a microinfarction lead to?
- How to act if you suspect a small focal infarction
- Therapy
- Prevention for people with heart disease
- General methods of prevention
“Microinfarction” is the popular name for the disease - small-focal myocardial infarction. Often the symptoms of the disease are attributed to fatigue or a cold, so many do not attach importance to the ailments they experience during an attack.
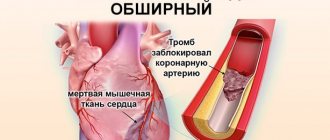
The cause of myocardial infarction is disruption of blood flow to the heart muscle due to a blood clot that blocks a coronary artery.
A heart attack can be recognized by chest discomfort, fever, weakness and aching bones.
What symptoms of a microinfarction do women experience?
The disease is very “insidious”, since the symptoms of a microinfarction in women are not always noticeable. Because of this, the diagnosis is made after the fact when other diseases occur.
One of the first symptoms is sudden chest pain. Pain may be present in the left side of the shoulder girdle, shoulder blade and jaw.
According to statistics, women are less likely to pay attention to the symptoms of a heart attack, as they are less sensitive to pain. Also, microinfarction often goes unnoticed by patients over 55-60 years of age and diabetics.
Microinfarction carried on the legs
Microinfarction, especially asymptomatic ones, can develop unnoticed. Many patients learn about a previous attack when undergoing electrocardiography, when the doctor determines the characteristic ECG signs.
If symptoms do develop, they are usually mistaken for another disease or illness. Acute pain in the heart often occurs, although it may be completely absent. Nausea, a feeling of pressure, and general malaise are often associated with mild poisoning, gastrointestinal upset, and not with a microinfarction. The condition may stabilize on its own, or complications may arise.
What symptoms of a microinfarction do men experience?
Men experience microinfarction less often and usually do not endure it on their feet. The first sign is chest pain, however, unlike women, men feel radiating pain in the abdomen. There may be a sensation of a foreign object in the chest. In men, the symptoms are more pronounced. During an attack, the patient may experience cold sweat, increased anxiety, bluish lips and an increase in body temperature up to 38 degrees.
Despite the fact that the risk of a small-focal heart attack is lower in men, the likelihood of encountering a real heart attack in the stronger sex is higher, since they are more susceptible to stress.
Risk factors for myocardial infarction
The main risk factor for myocardial infarction is atherosclerosis of the coronary arteries.
There are a number of factors that significantly increase the risk of developing this acute condition:
- Atherosclerosis. A disorder of lipid metabolism, in which the formation of atherosclerotic plaques on the walls of blood vessels occurs, is the main risk factor in the development of myocardial infarction.
- Age. The risk of developing the disease increases after 45–50 years of age.
- Floor. According to statistics, this acute condition occurs 1.5–2 times more often in women than in men; the risk of developing myocardial infarction is especially high in women during menopause.
- Arterial hypertension. People suffering from hypertension have an increased risk of cardiovascular accidents, since elevated blood pressure increases the myocardial oxygen demand.
- Previous myocardial infarction, even small focal ones.
- Smoking. This harmful habit leads to disruption of the functioning of many organs and systems of our body. With chronic nicotine intoxication, the coronary arteries narrow, which leads to insufficient oxygen supply to the myocardium. Moreover, we are talking not only about active smoking, but also passive smoking.
- Obesity and physical inactivity. If fat metabolism is disrupted, the development of atherosclerosis and arterial hypertension accelerates, and the risk of diabetes mellitus increases. Insufficient physical activity also negatively affects the body's metabolism, being one of the reasons for the accumulation of excess body weight.
- Diabetes. Patients suffering from diabetes have a high risk of developing myocardial infarction, since elevated blood glucose levels have a detrimental effect on the walls of blood vessels and hemoglobin, impairing its transport function (oxygen transfer).
Symptoms of myocardial infarction
This acute condition has quite specific symptoms, and they are usually so pronounced that they cannot go unnoticed. However, it should be remembered that atypical forms of this disease also occur.
In the vast majority of cases, patients experience a typical painful form of myocardial infarction, thanks to which the doctor has the opportunity to correctly diagnose the disease and immediately begin its treatment.
The main symptom of the disease is severe pain. The pain that occurs during myocardial infarction is localized behind the sternum, it is burning, dagger-like, and some patients characterize it as “tearing.” The pain can radiate to the left arm, lower jaw, and interscapular area. The occurrence of this symptom is not always preceded by physical activity; pain often occurs at rest or at night. The described characteristics of the pain syndrome are similar to those during an attack of angina, however, they have clear differences.
Unlike an attack of angina, pain during myocardial infarction persists for more than 30 minutes and is not relieved by rest or repeated administration of nitroglycerin. It should be noted that even in cases where a painful attack lasts more than 15 minutes, and the measures taken are ineffective, it is necessary to immediately call an ambulance team.
Atypical forms of myocardial infarction
Myocardial infarction occurring in an atypical form can cause difficulties for a doctor when making a diagnosis.
Gastritis variant. The pain syndrome that occurs with this form of the disease resembles pain during exacerbation of gastritis and is localized in the epigastric region. On examination, tension in the muscles of the anterior abdominal wall may be observed. Typically, this form of myocardial infarction occurs when the lower parts of the left ventricle, which are adjacent to the diaphragm, are affected.
Asthmatic variant. Reminds me of a severe attack of bronchial asthma. The patient experiences suffocation, cough with foamy sputum (but can also be dry), while the typical pain syndrome is absent or mildly expressed. In severe cases, pulmonary edema may develop. Upon examination, cardiac arrhythmias, decreased blood pressure, and wheezing in the lungs may be detected. Most often, the asthmatic form of the disease occurs with repeated myocardial infarctions, as well as against the background of severe cardiosclerosis.
Arrhythmic option. This form of myocardial infarction manifests itself in the form of various arrhythmias (extrasystole, atrial fibrillation or paroxysmal tachycardia) or atrioventricular block of varying degrees. Due to heart rhythm disturbances, the picture of myocardial infarction on the electrocardiogram may be masked.
Cerebral option. Characterized by impaired blood circulation in the vessels of the brain. Patients may complain of dizziness, headache, nausea and vomiting, weakness in the limbs, and consciousness may be confused.
Painless option (erased form). This form of myocardial infarction causes the greatest difficulties in diagnosis. Pain syndrome may be completely absent; patients complain of vague chest discomfort and increased sweating. Most often, this erased form of the disease develops in patients with diabetes and is very difficult.
Sometimes the clinical picture of myocardial infarction may contain symptoms of different variants of the disease; the prognosis in such cases, unfortunately, is unfavorable.
General signs of microinfarction
Since the symptoms of a microinfarction can easily be confused with a regular illness, it is important to pay attention to the appearance of several signs at the same time.
What symptoms indicate a microinfarction:
- increased temperature, which causes necrosis of cardiac tissue;
- feeling of pain and aches in the joints;
- dizziness, weakness, possible loss of consciousness;
- swelling;
- sudden pain in the chest, radiating to the stomach, shoulder, shoulder blade;
- the appearance of shortness of breath, acute lack of air;
- pain in the solar plexus area;
- cyanosis of the nasolabial triangle, lips.
Usually the attack lasts 40 minutes, and if no serious consequences occur, the symptoms go away. But this does not mean that they can be ignored. If signs of a microinfarction appear, you should immediately consult a doctor.
Causes
In 95% of cases, myocardial infarction is associated with blockage of an artery by a blood clot. The cause of illness is a lack of oxygen and nutrients in the heart muscle.
The supply of oxygen in the heart cells lasts for 10 seconds. Over the next 30 seconds, the muscle remains viable, after which the pathological process begins. 3-6 hours after the onset of the attack, the heart muscle in the damaged area dies. If a small area has died, then the infarction is considered small-focal.
The clinical picture of the disease is varied, which makes diagnosis difficult, and it can be difficult for specialists to confirm the disease in a short time.
The diagnosis is based on 3 indicators:
- medical history, complaints of pain typical of a heart attack;
- ECG indicators;
- results of a biochemical blood test.
If the doctor has doubts, he may prescribe additional studies, for example, identifying the lesion using the radioisotope method.
Prevention
- Check your blood pressure at home. High blood pressure can lead to a heart attack. Sit and rest for 5 minutes before taking your readings. Measure your blood pressure at least 2 times a day at the same time, for example, in the morning and evening.
- Quit smoking. Nicotine and other chemicals in cigarettes and cigars can cause damage to the lungs and heart. Electronic cigarettes or smokeless tobacco also contain nicotine and are no less dangerous.
- Eat a heart-healthy diet. A heart-healthy diet is one that is low in saturated, unhealthy fats and sodium (salt). It helps reduce the risk of heart disease and stroke. Limit the amount of fat you consume to 25-35% of your total daily calories. Your doctor may recommend an eating plan that lowers your cholesterol and blood pressure.
- Limit your sodium (salt) intake. Too much sodium can affect fluid balance. Do the exercises. Ask your doctor about the exercise plan that's best for you. Exercise strengthens the heart, lowers blood pressure and helps prevent heart attacks. The goal is 30 to 60 minutes of activity almost every day.
- Maintain a healthy weight. Ask your doctor how much you should weigh. He can help you create a safe weight loss plan if you are overweight.
- Manage stress. Stress can increase your risk of heart attack. Learn ways to control stress, such as relaxation, deep breathing and music. Talk to someone about what's upsetting youSource: Innovative Methods to Prevent Myocardial Infarction. Volodkin A.A. , Zaikov G.E. NBI-technologies, 2013. p. 103-106.
Sources:
- Myocardial infarction. Zhmurov D.V., Parfenteva M.A., Semenova Yu.V. Colloquium-journal, 2021. p. 56-61
- Outcomes of recurrent myocardial infarction. Shulaev A.V., Muradimova Z.R., Marapov D.I., Zakirov I.K., Mazitov M.R. Practical medicine, 2021. p. 142-144
- Complications of myocardial infarction in the elderly. Khalmukhamedov B.T. Eurasian Journal of Cardiology, 2021. p. 29-30
- On the issue of overdiagnosis of myocardial infarction. Kim A.O., Kausova G.K. Bulletin of the Kazakh National Medical University, 2018. p. 28-29
- Innovative methods for preventing myocardial infarction. Volodkin A.A. , Zaikov G.E. NBI-technologies, 2013. p. 103-106
How to act if you suspect a small focal infarction
The first thing to do is call an ambulance. Pre-medical care for the patient consists of creating conditions of maximum comfort in order to alleviate the condition.
The patient needs to take a lying or semi-lying position, ensure a flow of fresh air into the room (avoid drafts). Eliminate light and sound stimuli. If necessary, remove the patient from restrictive clothing. For medications, you can use nitroglycerin (dissolve under the tongue) or Corvalol (30-40 drops).
How to provide first aid to a patient?
The care regimen does not differ from that for suspected angina or large-focal infarction. If a person has pain in the heart area, it is recommended:
- at home, put him to bed, in public places try to give him a horizontal position, if he has shortness of breath, he can sit;
- ensure peace and sufficient air flow;
- from the medications available “at hand”, it is allowed to give up to three Nitroglycerin tablets under the tongue, one Aspirin;
- do not leave the patient unattended;
- Be sure to call an ambulance.
Therapy
The patient is taken to intensive care, where complex therapy is carried out. When treating a heart attack, the speed of reaction is very important: the faster the patient gets to the hospital and receives proper care, the higher the chances of a positive outcome and the absence or minimum number of complications.
Doctors use drugs that help dissolve a blood clot, painkillers, and medications to lower blood pressure and reduce blood circulation. Also, as part of treatment, it is necessary to achieve a decrease in heart rate, which is achieved by taking beta-blockers.
The rehabilitation period after inpatient treatment is no less important than the therapy itself. The recovery period lasts up to 6 months. The patient may be prescribed medications that must be taken constantly. Also, to maintain normal condition, it is necessary to follow a diet, in particular, eliminating fatty and fried foods from the diet, as well as stopping smoking and drinking alcohol.
If the doctor's recommendations are followed, the patient can count on a long and fulfilling life.
Anaprilin
- Has a hypotensive effect, reduces heart rate;
- Increases the resistance of the heart muscle to oxygen starvation;
- Prevents the development of arrhythmia.
More details
THERE ARE CONTRAINDICATIONS. BEFORE USE, READ THE INSTRUCTIONS CAREFULLY OR CONSULT A DOCTOR
Treatment
Assistance for microinfarction should be provided only in the cardiology department of the hospital. The task of my colleagues is to relieve pain, localize the focus of necrosis and take measures so that the heart can function as before.
The following groups of drugs are used for treatment:
- anticoagulants;
- neuroleptanalgesia or narcotic analgesics;
- polarizing mixture, droppers with a solution of glucose and salts;
- beta blockers;
- antiarrhythmic drugs;
- prolonged nitrates.
The patient is advised to follow bed rest and a diet excluding salt and fatty foods. After discharge, physical, mental and social rehabilitation is desirable. If the patient’s professional activity is associated with constant overload, he is sent to a commission for transfer to easier work.
Prevention for people with heart disease
People with chronic diseases of the cardiovascular system need to undergo an annual medical examination in order to receive timely and adequate medical care.
As a preventive measure, patients with coronary heart disease are prescribed an assessment of the condition of the coronary arteries, during which the degree of narrowing and localization of atherosclerotic plaques will be identified. If necessary, the vessels are expanded from the inside using angioplasty. Another method is to implant a metal frame into the artery. It will prevent the passage from narrowing.
Some patients are prescribed coronary artery bypass grafting. During the operation, additional vessels are transplanted to the aorta, which go around the narrowing site and create additional pathways for blood flow to the heart.
Diagnostics
Understanding that a microinfarction is a condition that is very dangerous to health, at the first sign of it you need to call an ambulance. After taking the first measures to alleviate the person’s condition, he will be taken to the hospital, where the examination will be carried out. It is as follows:
- physical examination of the patient;
- collecting anamnesis, studying medical history;
- measuring blood pressure and pulse;
- taking an ECG;
- Ultrasound of the heart.
The patient must also donate blood and urine for analysis and undergo Holter monitoring if indicated. It will allow you to track the work of the heart over a long period of time, obtaining the most complete information about the patient’s condition.